Jaundice : neonatal guideline
The management of neonatal jaundice is a particular challenge to the neonatologist. Mild jaundice is a common and usually harmless feature of the neonatal period, seen on a daily basis by staff in a huge variety of settings. This is set against the occasional but devastating complication of kernicterus (with its long term implications) in those who are more severely affected.
Balancing the desire to avoid excessive intrusive investigations for the healthy majority against attempts to capture those who would go on to develop kernicterus if untreated is a significant challenge.
NICE has produced guidance for England and Wales on this subject 1. This gives detailed recommendations for recognition and management of neonatal jaundice. This has been the source of a great deal of discussion, with divergent opinions; some praising the approach2 for its thoroughness, others stating concerns that it is too permissive3 and many being concerned about the practicalities of implementing the guidance in disparate healthcare settings.
Whilst there is no statutory obligation to follow NICE guidance in Scotland, it was felt that local guidance should be developed that ensured that practice was not too divergent from that described. This document attempts to address these issues in a practical manner.
Click here to download the NICE Neonatal Jaundice treatment threshold graphs (excel spreadsheet).
This section gives guidance on the management of jaundice noted in the first two weeks of life. Separate guidance on management of infants over 2 weeks old is contained in the prolonged jaundice section further into this document.
Testing guidance
Hospital
Key points:
- Healthcare professionals should use every opportunity to assess infants for the development of visible jaundice.
- Higher risk babies should receive an additional inspection.
- If jaundice is visible then a bilirubin level must be measured using a transcutaneous bilirubinometer or serum testing.
- A serum bilirubin must be obtained in babies less than 35 weeks gestation or less than 24 hours old with visible jaundice
- Visual estimation of the severity of jaundice is no longer acceptable.
Detailed guidance
In all babies:
- examine the baby for jaundice at every opportunity especially in the first 72 hours. When looking for jaundice (visual inspection):
- check the naked baby in bright and preferably natural light
- examination of the sclerae, gums and blanched skin is useful across all skin tones.
- The presence or absence of jaundice should be recorded in the notes whenever a baby is examined by a healthcare professional.
High risk infants:
At delivery the midwife looking after the mother should check whether there are factors associated with an increased likelihood of developing significant hyperbilirubinaemia soon after birth:
High risk criteria:
- Gestational age under 38 weeks.
- A previous sibling with neonatal jaundice requiring phototherapy
- This should be recorded clearly on Maternity Badger whenever this
information comes to light during pregnancy.
- This should be recorded clearly on Maternity Badger whenever this
- Mother’s intention to breastfeed exclusively.
Arrangements should be made for identification of infants in these categories, and particular attention made to assessing for jaundice. If visible jaundice is noted by any member of staff prior to this additional check taking place then immediate action should be taken rather than awaiting this additional check.
Urgent additional care for babies with visible jaundice in the first 24 hours:
Measure and record the serum bilirubin level urgently (within 2 hours of detection) in all babies with suspected or obvious jaundice in the first 24 hours of life.
Continue to measure the serum bilirubin level every 6 hours for all babies with suspected or obvious jaundice in the first 24 hours of life until the level is below the treatment threshold and stable and/ falling (this decision should be made by a middle grade or consultant).
How to measure the bilirubin level
A bilirubin level should be measure in all jaundiced babies. When measuring the bilirubin level:
- use a transcutaneous bilirubinometer in babies with a gestational age of 35 weeks or more and postnatal age of more than 24 hours.
- if a transcutaneous bilirubinometer is not available, measure the serum bilirubin
- if a transcutaneous bilirubinometer measurement indicates a bilirubin level greater than 250 micromol/litre a serum bilirubin should be obtained.
- if the transcutaneous bilirubin is within 25micromols/l of the treatment line a serum bilirubin should be obtained (use treatment threshold graph).
- always use serum bilirubin measurement to determine the bilirubin level in babies with jaundice in the first 24 hours of life.
- always use serum bilirubin measurement to determine the bilirubin level in babies less than 35 weeks gestational age.
- always use serum bilirubin measurement for babies at or above the relevant treatment threshold for their postnatal age, and for all subsequent measurements.
Additional tests
In addition to a full clinical examination by a suitably trained healthcare professional, carry out all of the following tests in babies with significant (i.e. requiring treatment) hyperbilirubinaemia as part of an assessment for underlying disease (see threshold chart in appendix 1)
- serum bilirubin (for baseline level to assess response to treatment)
- Full blood count
- blood group (mother and baby)
- DAT (Coombs’ test). Interpret the result taking account of the strength of reaction, and whether mother received prophylactic anti-D immunoglobulin during pregnancy.
When assessing the baby for underlying disease consider whether the following tests are clinically indicated:
- blood glucose-6-phosphate dehydrogenase levels, taking account of ethnic origin
- microbiological cultures of blood, urine and/or cerebrospinal fluid (if infection is suspected).
Timing of repeat samples where the initial measurement is below the treatment threshold:
In 2016 NICE revised their guidance around the timing of repeat samples for infants of 38 weeks gestation or more to the following:
- Within 50micromols/l of the treatment line:
- No additional risk factors- recheck within 24 hours
- Additional risk factors- recheck within 18 hours
Testing frequency guidance is not given for more immature infants. Given their greater susceptibility to kernicterus it would be prudent to ensure that they are retested within 18 hours, less where there are additional risk factors.
Where the bilirubin level is more than 50 micromols/l below the treatment line routine retesting is not required, unless the rate of rise based on serial measurements is a concern, or the clinical situation changes.
Community testing guidance
Timely and accurate measurement of bilirubin levels in the community is a particular practical challenge. With early discharge now the norm it must be recognised that a significant proportion of the assessment of jaundice occurs outwith the hospital setting and away from easy access to measurement resources.
At present the following is recommended:
- Every opportunity should be used while infants are in hospital to accurately measure bilirubin if jaundice is visible.
- Where a bilirubin has been measured the result and subsequent plans for follow up should be made clear to the community midwifery team
- The inaccuracy of visual estimation of bilirubin levels should be borne in mind at all times and if in any doubt a level should be measured, either using transcutaneous bilirubinometry or blood testing.
- It is preferable that measurement takes place in the community rather than by referral to hospital (unless there are other concerns about the infant).
Community teams should seek to improve access to transcutaneous bilirubinometers and/or ensure that staff are able to take, and have processed, blood samples for serum bilirubin.
Remote and rural areas should develop robust guidance with their referral neonatal units to facilitate this process.
When to treat
Treatment should be commenced one a serum bilirubin has confirmed that the bilirubin level is over the treatment threshold. Exceptions to this would be where a transcutaneous bilirubin measurement is so high that there is concern about the time taken to confirm with a serum sample (a serum sample must be taken, treatment may be started without it), or where the rate of rise is clearly going to take the bilirubin level above the treatment threshold in the next 6 hours.
Thresholds
All level must be plotted on the treatment charts available in appendix 1. Care must be taken to ensure that the baby’s age in hours has been accurately calculated and plotted appropriately. Treatment thresholds will vary with gestation and postnatal age so it is vital that plotting is accurate.
How to treat
Phototherapy
Type of phototherapy
The effectiveness of phototherapy is dependent on the light output of the device and the exposure of the infant rather than whether it is an overhead or under baby device. Under-baby devices have advantages in terms of the ability to continue use when breastfeeding, less light pollution for others in the area and no need for the baby to be undressed etc, so where devices with appropriate outputs are available should be the first choice.
NICE suggests the following as evidence that the bilirubin is not coming under control and suggests moving to multiple phototherapy:
- the serum bilirubin level is rising rapidly (more than 8.5 micromol/litre per hour)
- the serum bilirubin is at a level that is within 50 micromol/litre below the threshold for which exchange transfusion is indicated after 72 hours (see treatment threshold chart, appendix 1).
- the bilirubin level fails to respond to single phototherapy (that is, the level of serum bilirubin continues to rise, or does not fall, within 6 hours of starting single phototherapy). Care must be taken to ensure that phototherapy is being adequately delivered at all times.
- Single phototherapy can be reverted back to once the serum bilirubin has fallen greater than 50micromol/litre below the exchange transfusion threshold and is stable/falling (this decision should be made by a middle grade or consultant).
Care while receiving phototherapy
- place the baby in a supine position unless other clinical conditions prevent this
- ensure treatment is applied to the maximum area of skin
- monitor the baby’s temperature and ensure the baby is kept in an environment that will minimise energy expenditure (thermoneutral environment)
- monitor hydration by daily weighing of the baby and assessing wet nappies
- support parents and carers and encourage them to interact with the baby.
- Give the baby eye protection and routine eye care during overhead phototherapy.
Monitoring the baby during phototherapy
During conventional ‘blue light’ phototherapy:
- using clinical judgement, encourage short breaks (of up to 30 minutes) for breastfeeding, nappy changing and cuddles
- continue lactation/feeding support
- do not give additional fluids or feeds routinely. Maternal expressed milk is the
additional feed of choice if available, and when additional feeds are indicated. Donor
EBM may be considered if EBM is unavailable
During multiple phototherapy:
- do not interrupt phototherapy for feeding but continue administering intravenous/enteral feeds
- continue lactation/feeding support so that breastfeeding can start again when treatment stops.
- Maternal expressed milk is the additional feed of choice if available, and when additional feeds are indicated.
Measuring bilirubin after commencing phototherapy.
NICE recommend checking an initial bilirubin 4-6 hours after commencing phototherapy, and 6-12 hourly thereafter if the bilirubin is falling. Decisions regarding the frequency and timing of repeat samples should take into account how far above the treatment line the bilirubin is, the age of the child and may include factors such as avoidance of overly frequent sampling overnight. Patient safety must be the priority however, and deviations from the recommended schedule should be done by an appropriately senior (middle grade level or above) member of staff after due consideration of all relevant factors
Stopping phototherapy
Stop phototherapy once serum bilirubin has fallen to a level at least 50 micromol/litre
below the phototherapy threshold (see threshold table and treatment threshold
graphs).
NICE recommend a check for rebound of significant hyperbilirubinaemia with a repeat
serum bilirubin measurement 12–18 hours after stopping phototherapy. Babies do not
necessarily have to remain in hospital for this to be done, but a clear plan will need to
be made for this to happen, including where appropriate communication with the
community midwifery team. It is recognised that a 12-18 hour wait is not always
practical without unduly delaying discharge, particularly where arrangements for
checking serum samples in the community are not in place. In these circumstances a
sample can be taken earlier, but must be interpreted accordingly.
Intravenous immunoglobulin
Use intravenous immunoglobulin (IVIG) (500 mg/kg over 4 hours) as an adjunct to continuous multiple phototherapy in cases of Rhesus haemolytic disease or ABO haemolytic disease when the serum bilirubin continues to rise by more than 8.5 micromol/litre per hour. The relevant request form will need to be completed to obtain IVIG.
Offer parents or carers information on IVIG including:
- why IVIG is being considered
- why IVIG may be needed to treat significant hyperbilirubinaemia
- the possible adverse effects of IVIG
- when it will be possible for parents or carers to see and hold the baby.
Exchange transfusion
Use a double-volume exchange transfusion to treat babies:
- whose serum bilirubin level indicates its necessity (see treatment charts).
and/or
- with clinical features and signs of acute bilirubin encephalopathy.
During exchange transfusion do not :
- stop continuous multiple phototherapy
- perform a single-volume exchange
- use albumin priming
- routinely administer intravenous calcium.
- Following exchange transfusion:
- maintain continuous multiple phototherapy
measure serum bilirubin level within 2 hours and manage according to the threshold table
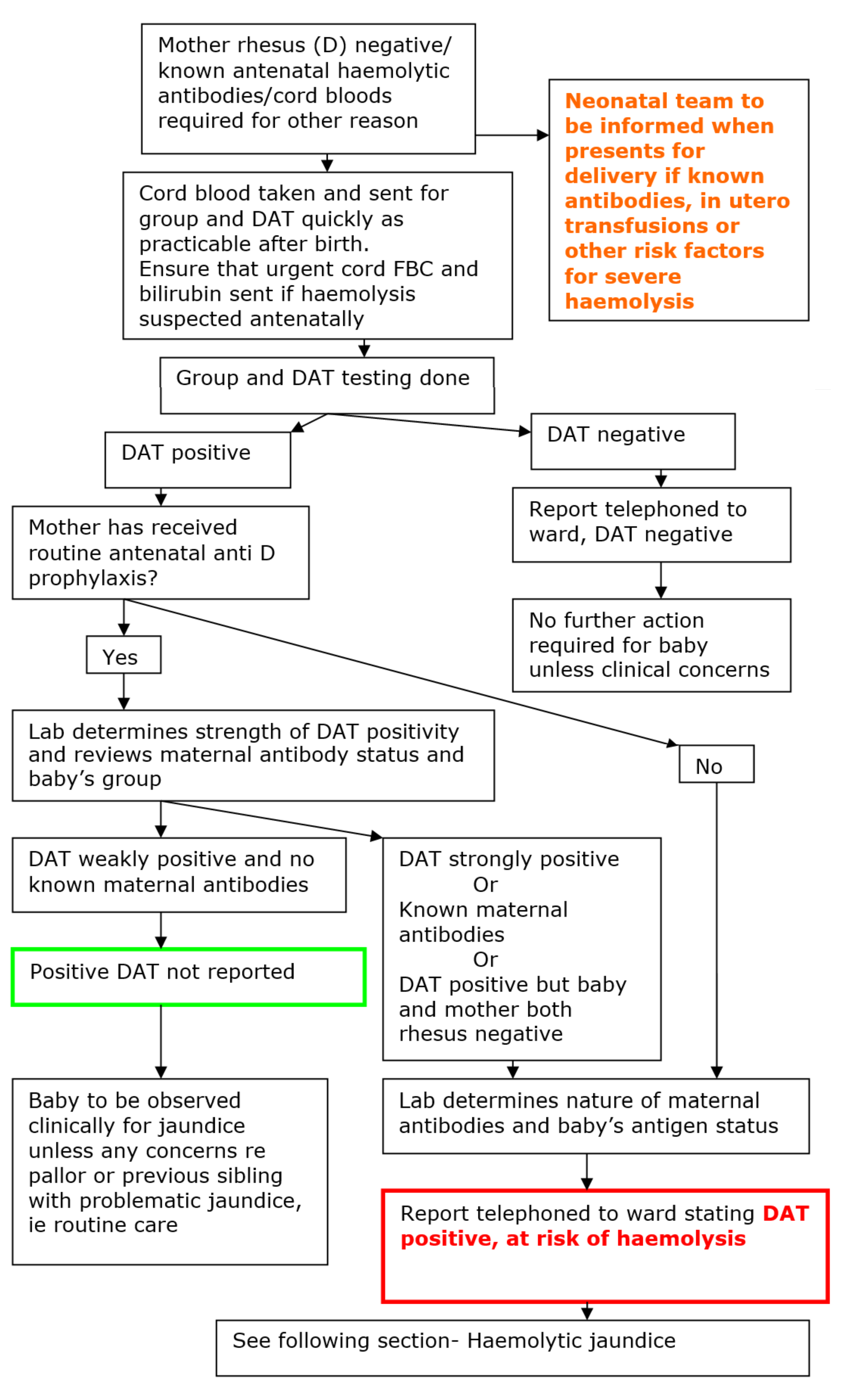
Introduction
The introduction of routine antenatal anti D prophylaxis has resulted in many babies testing
Coombs (more correctly Direct Antiglobulin Test or DAT) positive who are not at risk of
haemolysis. This guideline has been developed in conjunction with blood transfusion services to facilitate identification of those at high risk without unnecessary intervention for those that are not.
This guideline does not replace clinical judgement, if there is a suspicion of active haemolysis in a neonate in any situation then they should be managed as such in the manner described in the section subsequent to this.
Quick guide:
Where a mother has received routine antenatal anti D prophylaxis, only strongly positive DATs will be reported by the lab as Positive
- Unless the baby is also rhesus negative or there are known maternal antibodies
Weakly positive DATs will no longer be reported as positive in this situation, though the lab will give this result if asked (e.g. if the baby has significant jaundice etc)
Background
Current obstetric management of rhesus negative women (routine anti D prophlaxis) means
large numbers of babies testing positive on cord Coombs/Direct Antibody testing (DAT). Local audit and national guidelines (British council for standards in haematology) show that these babies are not liable to significant haemolysis.
National guidelines (British council for standards in haematology) recommend that DAT/Coombs testing is not done in infants born to mothers who have received prophylactic anti D. Abandoning this altogether however runs the risk of missing a baby who has other
haemolytic maternal antibodies (e.g anti-c), which could lead to brisk haemolysis in the days after birth with the associated morbidities that this brings. Therefore this risk analysis based approach has been developed.
The risk analysis is based on the fact that maternal antibodies that lead to haemolysis will
develop prior to the start of the third trimester (2). All women receiving anti D will have an
antibody screen taken before they receive anti D at 28 weeks gestation. Absence of haemolytic antibodies at this time means that there is no increased risk of postnatal haemolysis.
Management
Maternal casenotes should be reviewed on presentation to labour suite for any paediatric alerts on the yellow sheet, and these communicated to the neonatal team.
If no specific action prompted by paediatric alert section or other correspondence, but the mother is rhesus negative cord bloods should be taken and sent for group and DAT/Coombs testing.
Process Summary
Further detail
DAT positive, at risk of haemolysis
Those at highest risk where antibodies have been detected during pregnancy should have been highlighted in Maternity Badger. Accompanying this should be a description of the antibodies detected including quantification and an estimate of the likely risk posed to the infant. The neonatal team should be advised of any women with irregular antibodies on presentation to labour suite to allow time for interpretation of the predicted severity of the situation and liaison with BTS where required.
If there is no alert and the cord bloods are DAT positive the neonatal team should be informed immediately and the result recorded clearly in the baby’s casenotes along with any other information from the lab. The neonatal team should then review the baby and casenotes for further information and manage as below.
Action:
Treat as per haemolytic jaundice below, ie take and send urgent FBC and SBR (or seek results from cord bloods if taken), consider commencing immediate phototherapy.
Haemolytic jaundice is a pathological condition. The baby with haemolytic jaundice is at risk of:
- Anaemia at birth - seen where in-utero haemolysis has been severe and may indicate the need for urgent exchange transfusion
- High levels of unconjugated jaundice with the associated risks of kernicterus and deafness
- Late anaemia; presenting later after days or weeks of persistent haemolysis
The cornerstone of management is close monitoring and the anticipation of treatment requirements.
Anticipation of problems at birth: Babies with marked in-utero haemolysis
The following are indications that the baby may require treatment either immediately upon delivery or shortly thereafter:
- High or rapidly rising titres, in the mother, of antibodies known to be associated with haemolytic disease Rhesus (D, C, E, c, e), Kell. Or where other irregular antibodies are found in the maternal serum associated with a history of severe haemolysis in a sibling
- Evidence of significant anaemia in-utero – hydrops or increased velocity of middle cerebral artery dopplers or a history of in-utero transfusion in this pregnancy
Management of babies at risk of problems at birth
- Neonatal consultant to be informed of intended delivery
- Prior to the delivery it should be ensured that blood is available for exchange transfusion, if required. N.B. 2 units are usually required
- Paediatric staff (SHO and registrar) should attend the delivery
Anticipation of rapid onset of hyperbilirubinaemia: All babies with haemolytic disease
The following groups of babies should be investigated for haemolysis:
- Babies in the above group with known in-utero haemolysis
- All babies born to mothers with irregular antibodies
- All babies who develop jaundice within the first 24 hours or who have a rapidly rising SBR
Investigations
FBC, Blood group, Coomb’s test, Serum Bilirubin (SBR). These should be taken as cord bloods if haemolysis was anticipated antenatally, or from the baby in the case of early onset jaundice.
When haemolysis is confirmed, the following investigations are required to monitor the baby’s progress
FBC – repeat daily initially, reducing once trend is determined
SBR – repeated at 4 hours after the baseline test to determine the rate of rise. Thereafter, based on this rate of rise, the SBR should be repeated 4-8 hourly until the SBR is clearly under control N.B. All SBR results should be plotted accurately, by hour of sampling, on a phototherapy chart.
Phototherapy for haemolytic jaundice
Treatment of haemolytic jaundice is by phototherapy. This may be commenced immediately if severe haemolysis is anticipated. Except where haemolysis is severe (bilirubin rising by>
8.5micromoles/l/hr) this should be by single phototherapy on the postnatal ward. It is important to ensure effective phototherapy i.e. maximal surface area exposure for most of the time. The baby should only come out for feeds, consider using a biliblanket during feeds if these are taking some time.
Where the SBR continues to rise despite effective phototherapy or where exchange transfusion is anticipated the baby should come to SCBU. Double phototherapy may be initiated on SCBU however it is important that the first unit is not moved away from the baby to accommodate the second unit. Units should ensure that they have up to date effective high luminescence devices.
Immunoglobulin
Use intravenous immunoglobulin (IVIG) (500 mg/kg over 4 hours) as an adjunct to continuous intensified phototherapy in cases of rhesus haemolytic disease or ABO haemolytic disease when the serum bilirubin continues to rise by more than 8.5 micromol/litre per hour.
The appropriate request form will be required to obtain IVIG
Indications for exchange transfusion
Exchange transfusions are only performed with consultant approval. Exchange is indicated if one of the following criteria are met
- SBR levels exceed the exchange line or where it is clear that they will do so in the next few hours.
- Severe anaemia at birth or during the first few days of treatment
- Where there are neurological signs of kernicterus despite SBR levels below the exchange line (rare).
For instructions on the performance of an exchange transfusion see transfusion protocol
Follow up of babies with haemolytic jaundice
Low grade haemolysis may continue in these infants, even in the absence of jaundice. Therefore:-
- All babies with haemolytic jaundice (i.e. DAT positive AND requiring phototherapy) should be discharged on folic acid for 3 months. Dose should as per the WoS Folic Acid drug monograph
Early follow up should be arranged to monitor for anaemia. This should be 1-2 weeks after discharge if there is any noticeable decline in Hb levels leading up to discharge. If in any doubt then discuss follow up with the consultant.
Jaundice persisting beyond day 14 is common, occurring in 2-15% of all neonates and 15-40% of those who are breast fed.4,5 Rarely it can be the earliest manifestation of serious underlying pathology which may benefit from prompt diagnosis (Table 1).6 Biliary atresia (BA) is an uncommon cause of prolonged jaundice, having an incidence of 1 in 14000 to 1 in 21000 live births.7 Early detection and surgical intervention significantly improves outcome. 7-9 Late detection of infants with BA led to the UK “Yellow Alert Campaign”. This encouraged screening of all neonates with jaundice persisting beyond 14 days to facilitate prompt diagnosis.9 However this inevitably lead to the investigation of many normal babies. In addition complications of cholestatic liver disease are rare prior to the third week of life, leading the North American Academy of Pediatric Gastroenterology, Hepatology and Nutrition to recommend that well breast fed infants can have screening delayed until three weeks of age.10, 11 Throughout the UK marked heterogeneity exists in the evaluation of prolonged jaundice, with variation in both timing and laboratory assessment.10-13
Local audit demonstrated that infants identified as having prolonged jaundice were having extensive investigations many of which necessitated repeat appointments (26% of cases) to demonstrate the normalisation of initially abnormal results. However, none were identified as having liver related pathology. The intention of this guideline is to rationalise our approach to the infant with prolonged jaundice in keeping with the guidelines advocated by the “yellow alert” campaign
Clinical guidelines
- Term babies who remain visibly jaundiced beyond 14 days require further assessment.
- Assuming there are no clinical concerns they can be assessed when convenient (within the next week) according to local practice.
- The following points of the history should be reviewed:
- Was the baby term (>37 weeks)
- Method of feeding
- Did the baby receive IM vitamin K
- Is the baby gaining weight adequately
- Has the baby had pale stools
- Has the baby had dark urine
- Is there any family history of note
- Was the baby jaundiced on the first day of life
- Did the baby receive phototherapy in the neonatal unit
- a feeding history
- Stool colour – Refer to stool colour chart (Figure 1).
- Examination, including measurement of the weight, should be carried out
- In the absence of any other concerns further investigations are limited to
- A Split bilirubin (Total bilirubin and conjugated bilirubin fraction)
- G6PD level -If ethnically indicated (See map of affected populations - Figure 2)
- Results are telephoned to the parents. No further follow up is required for a thriving, breast fed baby with a total bilirubin of <250 µmol/l and a conjugated bilirubin of <20 µmol/l
- Any uncertainty / abnormal results, particularly in formula fed babies, should be discussed with a consultant neonatologist
Table 1 below lists potential causes of prolonged jaundice
Fig 1 - Stool chart
Please note that this chart is for guidance only as colours may reproduce differently on different monitors or printers. Please refer to charts available on the neonatal units (provided by the Yellow Alert campaign)

Fig 2. Distribution of G6PD worldwide
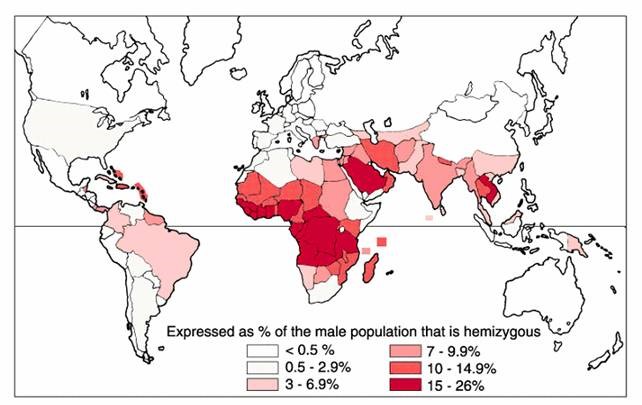
Table 1 - Conditions causing prolonged jaundice in newborns that require a specific treatment approach and therefore benefit from early diagnosis3
|
Bile duct abnormalities |
|
|
Metabolic disorders |
|
|
Infection |
|
|
Endocrine |
|
|
Toxins / injury |
|
|
Vascular |
|
|
Haemolysis |
|
| Who to assess: | All newborns are at risk and should be assessed at every opportunity for the development of jaundice. |
| Who to measure: |
Anyone with visible jaundice Babies with a family history of significant neonatal jaundice, DAT positive babies, breast fed babies and those under 38 weeks should receive special attention in looking for jaundice |
| How to measure: |
Transcutaneous bilirubinometer (unless under 35 weeks, under 24 hours, DAT positive or previous phototherapy) |
| When to take an SBR: | A serum bilirubin should be checked where the transcutaneous value is over 250micromol/l or within 25micomol/l of the treatment threshold. |
|
When to repeat bloods (>38wks): |
Within 50micromol/l of the treatment line:
|
| When to treat: |
Use new gestation specific treatment lines- babies should stay on their gestation specific graph until they are 14 days old. Treat when the serum bilirubin level is over the treatment line, or is clearly going to cross the line |
|
When to recheck after treatment has been started: |
Recheck an initial level after 6 hours, then 6-12 hourly if falling. |
|
When to stop phototherapy: |
Stop phototherapy when the serum bilirubin is at least 50micromol/l below the treatment threshold. |
|
When to recheck after stopping phototherapy: |
Recheck an SBR 12-18 hours after stopping phototherapy. |
- NICE Guideline. Jaundice in newborn babies under 28 days (CG98), 2010 (last updated October 2016)
- Detection and treatment of neonatal jaundice The Lancet, Volume 375, Issue 9729, Page 1845, 29 May 2010 doi:10.1016/S0140-6736(10)60852-5
- NICE guidelines on neonatal jaundice: at risk of being too nice The Lancet, Volume 376, Issue 9743, Page 771, 4 September 2010 doi:10.1016/S0140-6736(10)61376-1
- Hall RT. Hyperbilirubinaemia in breast-fed vs formula fed infants in the first 6 weeks of life. Relationship to weight gain. Am J Perinatol 1983;1: 47-51
- McKiernan PJ. Neonatal Cholestasis. Seminar Neonatol 2002; 7: 153-65
- Tyler W, McKeirnan PJ. Prolonged jaundice in the preterm infant. What to do when and why? Current Paediatrics 2006; 16: 43-50
- McKeirnan PJ, Baker A, Kelly DA. The frequency and outcome of biliary atresia in the UK and Ireland. The Lancet 2000; 355: 25-29
- McClement JW, Howard ER, Mowat AP. Results of surgical treatment for extrahepatic biliary atresia in United Kingdom 1980-2. Survey conducted on behalf of the British Paediatric Association Gastroenterology Group and the British Association of Paediatric Surgeons. Br Med J 1985; 290: 345-7
- Mielli- Vergani G, Howard ER, Portman B, Mowat AP. Late referal for biliary atresia missed opportunities for effective surgery. Lancet 1989; 1: 421-3
- Moyer V, Fresse DK, Whington PF. Guidelines for the evaluation of cholestatic jaundice in infants; Recommendations of the North American Society of Paediatric Gastro-enterology, Hepatology and Nutrition. JPGN 2004; 39: 115-28
- American Academy of Pediatrics. Practice Parameter: Management of hyperbilirubinaemia in the healthy term newborn. Pediatr 1994; 94: 558-65
- Newman TB, Maisels MJ. Evaluation and treatment of jaundice in the term newborn: a kinder gentler approach. Pediatr 1992; 89: 808-18
- Hannam S, McDonnell M, Rennie JM. Investigation of prolonged neonatal jaundice. Acta Paediatr 2000; 89: 694-7
- BSPGHAN guidelines for investigation of conjugated hyperbilirubinaemia.
Last reviewed: 21 March 2023
Next review: 31 March 2026
Author(s): Dr Allan Jackson – Consultant Neonatologist – PRM
Co-Author(s): Dr Andrew MacLaren – Consultant Neonatologist – RHC, Glasgow (2023 review)
Approved By: West of Scotland Neonatology Managed Clinical Network

