Early onset sepsis in the neonate: prevention and treatment
exp date isn't null, but text field is
Objectives
This guideline supersedes previous guidance for the prevention and treatment of Group B Streptococcal infection in the neonate. It is relevant to all medical, nursing and midwifery staff working with neonates in the hospital or community settings. Staff using this document should also be familiar with additional guidance on the use of antibiotics in the neonate and the monographs of the drugs referred to in this guidance. Staff should also refer to the NICE guideline "Neonatal infection: antibiotics for prevention and treatment: NG195" and the RCOG Green-top guideline “Group B Streptococcal Disease, Early-onset” which have been used as the basis for this document.
NB: Some centers use the ‘Kaiser Permanente neonatal sepsis calculator’ as an alternative system to determine risk of sepsis. NICE currently recommends using this calculator only as part of a prospective audit. This guideline follows the current NICE guidance and uses risk factors and clinical indicators to determine risk of infection
Early Onset Sepsis (EoS) in the Neonate is defined as infection in the first 72 hours after birth, although, in practice, most of these infections present within the first 24h of life. The organisms responsible for EoS in the neonate are predominantly those which may colonise the vagina or lower gastrointestinal tract in the mother. Such colonisation is frequently asymptomatic however it may be associated with rupture of the membranes and preterm labour. Less frequently these organisms may lead to chorioamnionitis which may in turn lead to sepsis in the mother or the neonate.
Causative organisms
- Group B Streptococcus (GBS)
- Gram negative bacteria (E. Coli, Enterobacter, Klebsiella)
- Staphylococci (Predominantly St. Aureus)
- Streptococci (other than GBS)
- Listeria
The commonest organism is GBS. The incidence of early onset sepsis in the neonate due to GBS may be reduced by offering intrapartum antibiotic prophylaxis (IAP) to mothers who are at risk of transmitting this organism to their baby during the birth. Those women who may benefit from IAP have been identified in two ways: firstly by screening for GBS carriage during the pregnancy and secondly by identifying clinical risk factors. The most cost-effective method depends on local epidemiology including maternal GBS carriage rates and the incidence of neonatal sepsis in the population. In the UK a risk-factor based approach is employed which is outlined in detail in the RCOG guideline “Group B Streptococcal Disease, Early-onset” (Green-top Guideline No. 36 2017)
The following groups of women should be offered IAP with an intravenous antibiotic which is effective against group B Streptococcus. This will be Benzylpenicillin or, for penicillin sensitive women, another antibiotic with activity against GBS should be used. (This will usually be either Vancomycin, Teicoplanin, or Clindamycin dependent on local antibiotic policy)
- are in pre-term labour or
- have group B streptococcal colonisation, bacteriuria or infection during the current pregnancy or
- have had group B streptococcal colonisation, bacteriuria or infection in a previous pregnancy, and have not had a negative test for group B streptococcus by enrichment culture or PCR on a rectovaginal swab samples collected between 35 and 37 weeks' gestation or 3-5 weeks before the anticipated delivery date in the current pregnancy or
- have had a previous baby with an invasive group B streptococcal infection or
- have a clinical diagnosis of chorioamnionitis.
IAP should be given, where possible, at least 2 hours prior to delivery for optimum efficacy
Note: - Women with GBS in a previous pregnancy
Women with GBS detected in a previous pregnancy have a 50% risk of recurrent GBS carriage and should be offered routine IAP or the option of bacteriological testing in late pregnancy, followed by IAP if still positive.
If performed, bacteriological testing should be carried out at 35-37 weeks gestation or 3-5 weeks prior to the anticipated delivery date, i.e. 32-34 weeks gestation in multiple pregnancies. A single (Amies charcoal) swab should be taken from the lower vagina and anorectum. Healthcare professionals should indicate that the swab is being taken for GBS.
Potentially infected women who require antibiotics that also cover GBS
For the following women, antibiotic therapy should be determined by Obstetric guidelines for sepsis, but in addition must include specific GBS prophylaxis (as above).
- Where chorioamnionitis is suspected
- Who have a pyrexia during labour (> 38°C) or a temperature of ≥ 37.5°C on 2 separate occasions at least 1 hour apart or maternal sepsis with a temperature < 36°C
- For whom the sepsis 6 bundle is triggered
N.B. IAP should be started as soon as possible after labour starts (or as soon as infection is suspected, in the case of chorioamnionitis), and continue until the birth of the baby.
[For optimum efficacy IAP needs to have been commenced at least 2 hours prior to delivery]
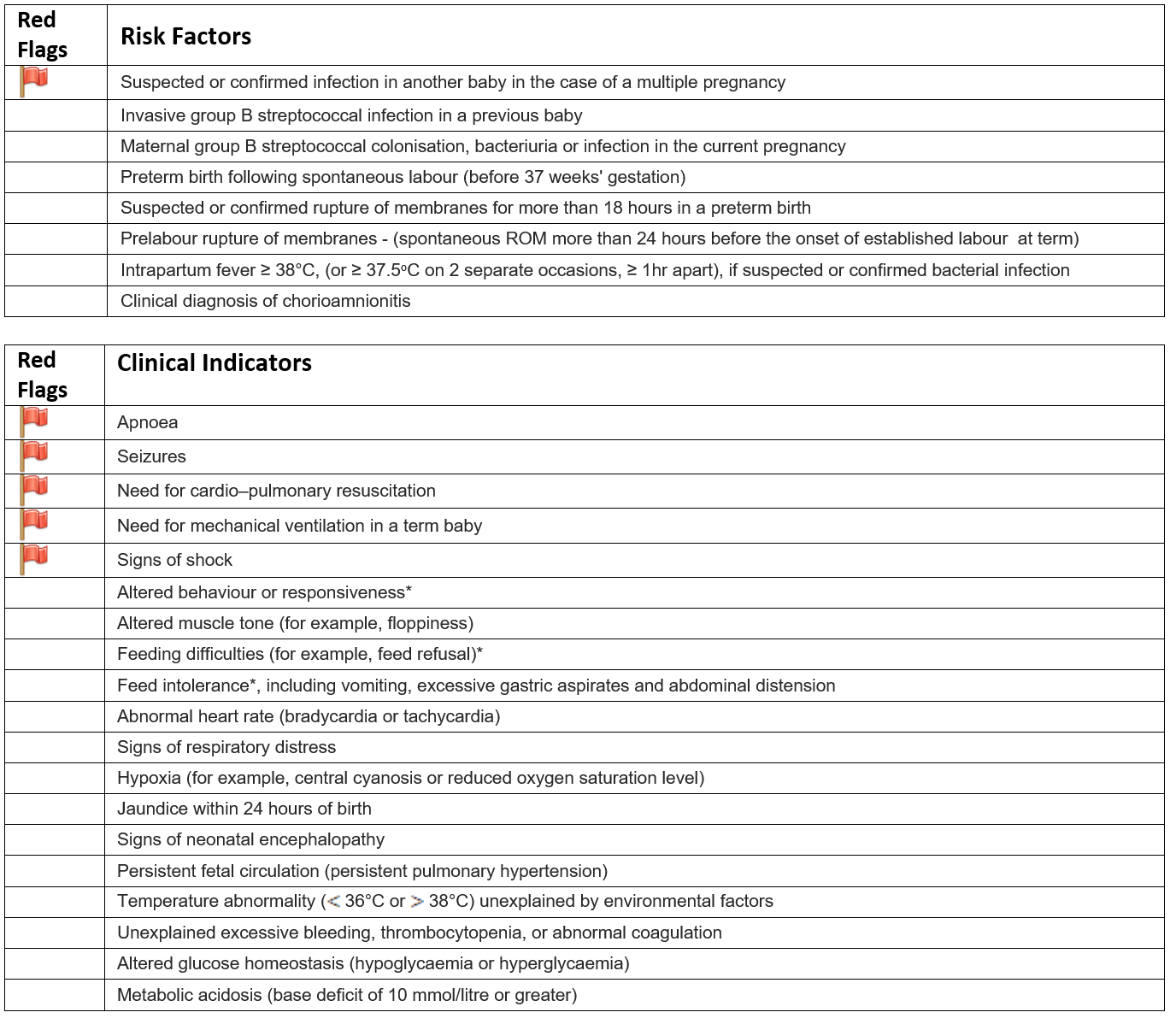
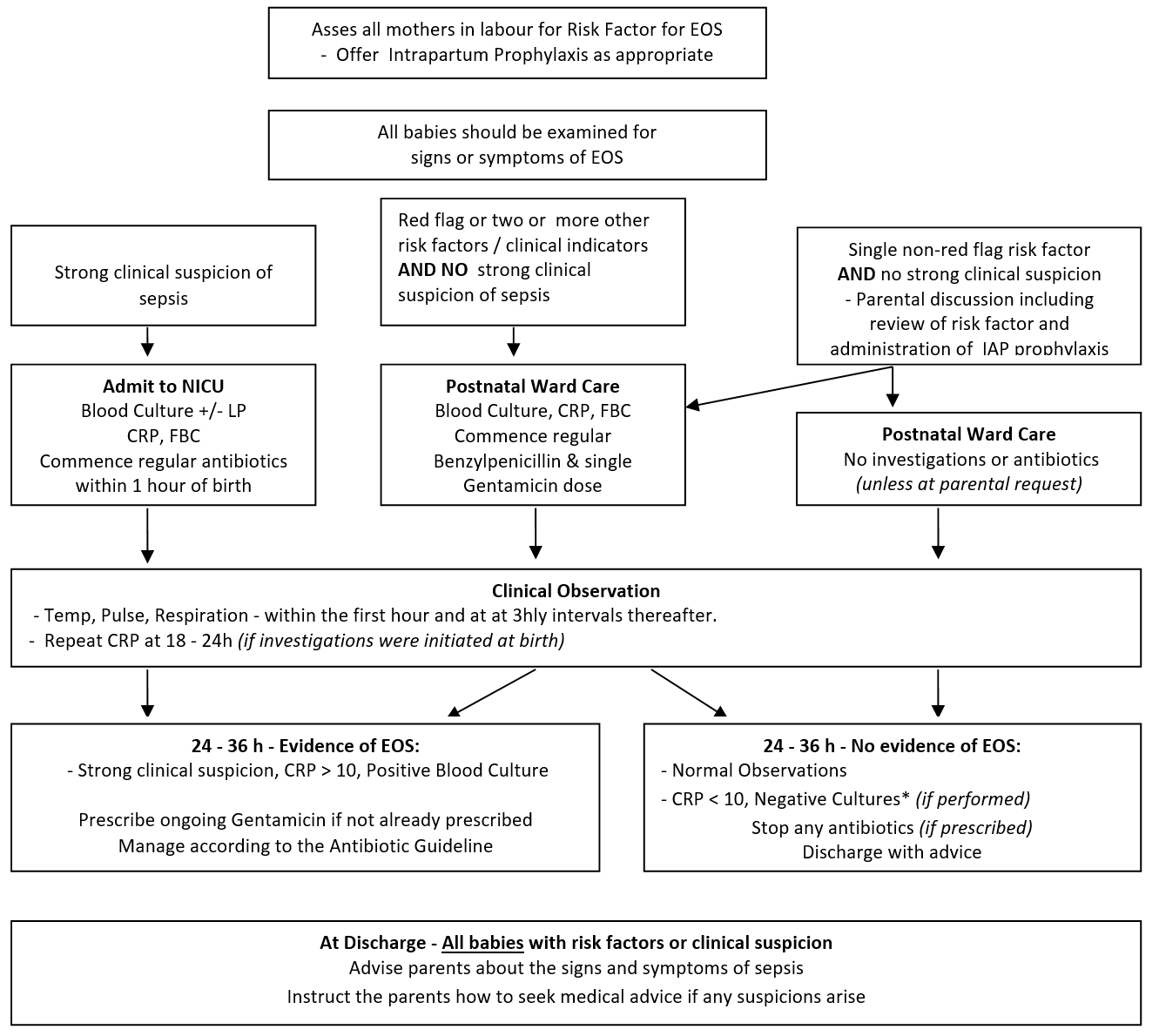
The NICE guideline determines the risk of early onset sepsis in the neonate using a framework of risk factors and clinical indicators. These are used to guide management and identify babies who require IV antibiotics.
See Table 1 below for a list of the risk factors and clinical indicators for early onset sepsis.
Document your clinical assessment and any discussions with parents clearly in the baby’s notes
Babies with ‘red flags’, multiple risk factors or abnormal clinical indicators
In this scenario, NICE recommends the prompt introduction of intravenous antibiotics.
NB. Antibiotics are recommended in this group even if adequate intrapartum prophylaxis has been given.
Babies with a strong clinical suspicion of sepsis must receive appropriate treatment promptly to reduce the mortality and morbidity associated with early onset sepsis. Parents should be fully informed regarding their baby's condition and the treatment required. However, this counselling should not delay appropriate therapy.
Babies with a single risk factor and no abnormal clinical signs
- For infants without any "red flags", who have only a single risk factor or clinical indicator for sepsis, use clinical judgement to decide whether it is safe to withhold antibiotics and closely monitoring the clinical condition of the infant over the first 24 hours.
- Parents should be informed about the risk factor / clinical indicator which has prompted this
- In the presence of a risk factor, parents should be told that the clinical examination has not identified any current signs or symptoms of active infection and that we will continue to monitor for these clinical signs throughout the first day of life. (Most babies who develop EOS will become unwell in the first 12-24h).
- In the presence of a clinical indicator, parents should be told that occasionally the indicator could be an early sign of infection and that the baby will be closely monitored throughout the first day of life.
- In either situation the parents should be informed that antibiotics may be recommended depending on clinical course.
- A parental leaflet should be provided which will explain this recommendation and provide information about the signs and symptoms of infection in a baby.
- If the parents are uncomfortable with the decision not to perform any additional investigations, or treat with antibiotics, then this should be taken into account when planning the baby's care. At the discretion of the medical staff the baby could be managed in the same way as babies with multiple risk factors or clinical concerns as outlined above.
* note that sleepiness, minor vomiting and early reluctance to feed are common symptoms in the normal neonate in the first day of life. Clinical judgement must be used to determine whether these are more pronounced than usual for a baby of that gestation and age.
For those babies identified as requiring investigation the following tests should be requested.
Baseline
Babies receiving antibiotic therapy
- FBC and differential
- CRP
- Blood culture
Selected babies
- Lumbar Puncture Perform a lumbar puncture to obtain a cerebrospinal fluid sample before starting antibiotics if it is thought safe to do so and:
- There is a strong clinical suspicion of infection, or
- There are clinical symptoms or signs suggesting meningitis.
If performing the lumbar puncture would unduly delay starting antibiotics, perform it as soon as possible after starting antibiotics.
- Swabs - Routine swabs are not required but should be taken if the baby has:
- A purulent eye discharge. Swabs should be taken using methods that can detect Chlamydia and Gonococcus. See separate guidance in the WoS guideline for eye infection in the neonate
- Clinical signs of umbilical infection, such as a purulent discharge or signs of periumbilical cellulitis. Swabs should be sent for microbiology.
Antibiotic choice may need to be altered in these cases; please seek senior support
18-24 hours
Babies receiving antibiotic therapy
- CRP
If antibiotic therapy continuing
- FBC
- U&E
- LFT
Subsequent investigations
Only babies requiring ongoing antibiotic therapy require additional investigations
- CRP - at appropriate intervals to monitor response to treatment
- Gentamicin levels before 3rd dose
- Lumbar Puncture – reconsider if a baby has a positive blood culture, there is an unsatisfactory response to antibiotics, suspicion of infection becomes strong or there are symptoms/signs suggesting meningitis
Antibiotic choice
- NICE recommends benzylpenicillin and gentamicin as initial antibiotic choice
- Prescribe gentamicin as a once only medication in the first instance.
- N.B. A decision should be made by 36h whether to discontinue antibiotics OR to prescribe regular gentamicin dosage.
- Consider cefotaxime if there is evidence of meningitis
Duration of antibiotics
For babies with a strong clinical suspicion of sepsis, or proven sepsis.
NB – If there is strong evidence, or proof, of Early Onset Sepsis (EOS) the paediatric team should inform their Obstetric colleagues. This may help guide maternal therapy if the mother is also unwell.
These babies will be managed initially on the neonatal unit and treated according to the antibiotic guideline. Antibiotics should be commenced within 1h of decision to treat
Babies with proven sepsis will generally require a minimum of 7d antibiotics. Longer courses may be required dependent on microbiological results, or in the presence of meningitis – see separate guidance for antibiotic therapy.
In cases of clinically suspected sepsis, if the blood cultures remain negative, the baby has clinically improved, and the CRP falls to below 10, antibiotic therapy may be discontinued earlier in the course of treatment
For babies with a ‘red flag’ OR two or more risk factors or clinical indicators BUT without a strong clinical suspicion of sepsis
NB – follow this guidance whether or not Intrapartum Prophylaxis has been given
These babies may be managed on the postnatal wards after their initial investigations.
Antibiotics should be prescribed as above. Repeat CRP should be taken 18-24h later to enable a decision to be made about the need for further treatment within 36h (NICE recommendation)
If both CRP tests (Baseline & 18-24h later) are <10 AND there are no clinical signs of infection then antibiotics may be discontinued.
If either CRP is >10 then Gentamicin should be prescribed on an ongoing basis commencing alongside the 3rd Benzylpenicillin dose. As above, the duration of treatment will be based on the results of blood cultures and/or the persistence of clinical signs.
N.B. - If continuing antibiotics for longer than 36 hours despite negative blood cultures, [due to persisting clinical signs] review the baby at least once every 24 hours. Consider at each review whether it is appropriate to stop antibiotic treatment, taking account of:
- The level of initial clinical suspicion of infection and
- The baby's clinical progress and current condition and
- The levels and trends of C-reactive protein concentration
The decision to continue antibiotics in this context should be clearly documented.
For babies with a single 'non-red flag' risk factor or clinical indicator and no clinical evidence of sepsis.
For these infants we would recommend the following:
- Withholding antibiotics and observing the baby for 12-24 hours.
Parents should be informed about the risk factor which has prompted this recommendation. The parents should be told that the clinical examination has not identified any current signs or symptoms of active infection and that we will continue to monitor these clinical signs throughout the first day of life. (Most babies who develop EOS will become unwell in the first 12-24h).
We recommend that all such infants are observed for this period irrespective of whether intrapartum prophylaxis was given or not.
A parental leaflet will be provided which will explain this recommendation and to provide information about the signs and symptoms of infection in a baby.
If the parents are uncomfortable with the decision not to perform any additional investigations, or treat with antibiotics, then this should be taken into account when planning the baby's care. At the discretion of the medical staff the baby could be managed in the same way as babies with multiple risk factors or clinical concerns as outlined above.
*It is important to ensure that the local microbiology department regularly monitors blood cultures for growth during the incubation period. This will ensure that the lack of a positive culture report in the period between 24-36h truly indicates a lack of microbial growth.
Decisions regarding investigation and treatment
Babies with a strong clinical suspicion of sepsis must receive appropriate treatment promptly to reduce the mortality and morbidity associated with early onset sepsis. Parents should be fully informed regarding their baby's condition and the treatment required. However, this counselling should not delay appropriate therapy.
Where a baby has only 'non-red flag' risk factors, or clinical indicators, we will recommend withholding antibiotics and keeping the baby under close observation for 24 hours. If the parents are uncomfortable with this recommendation the clinician may, at discretion, manage the baby in the same fashion as an infant with multiple risk factors or clinical signs.
Advice regarding babies who become unwell after discharge
If there have been any concerns about early-onset neonatal infection before a baby is discharged, whether or not the baby received treatment, advise the parents and carers verbally and in writing that they should seek medical advice (for example, from NHS 24, their general practice, or an accident and emergency department) if they are concerned that the baby:
- Is showing abnormal behaviour (for example, inconsolable crying or listlessness),
- Is unusually floppy,
- Has developed difficulties with feeding or with tolerating feeds
- Has an abnormal temperature unexplained by environmental factors (lower than 36°C or higher than 38°C
- Has rapid breathing,
- Has a change in skin colour.
- Are antibiotics started by1h of age if any red flag, or multiple risk factors, at birth
- Are antibiotics started within 1h of decision to treat where clinical concerns identified postnatally
- Is there a decision to continue / stop antibiotics documented by 36h after commencement of antibiotic course
- If antibiotics continued >36h, are the reasons for this clearly documented AND is there a documented daily review of the continued need for antibiotics
- Is appropriate parent information leaflet provided
Last reviewed: 31 October 2022
Next review: 01 October 2025
Author(s): Dr Andrew Powls - Consultant Neonatologist. Princess Royal Maternity, Glasgow
Approved By: WoS Neonatal MCN

