Eye infections in the neonate: Ophthalmia Neonatorum and the management of systemic Gonococcal and Chlamydial infections
exp date isn't null, but text field is
Objectives
This document is applicable to all medical, midwifery and nursing staff caring for the newborn in hospital or community. The guideline should be used with reference to the relevant pharmacy monographs and guidelines for taking and transportation of specimens for the diagnosis of bacterial and Chlamydia infections. It should be remembered that that strict maternal confidentiality should be observed when either of these pathogens is suspected.
A ‘sticky eye’ is a relatively common problem in infancy and ophthalmia neonatorum refers to any conjunctivitis (defined as conjunctival inflammation) occurring within the first 28 days of life. It is often due simply to a blocked lacrimal duct but may also be caused by a variety of bacterial and viral pathogens (Table One).
|
Aetiology |
Bacterial |
Viral |
Non-infectious |
|
Organisms |
Chlamydia trachomatis Neisseria gonorrhoea Haemophilus influenza Staphylococcus aureus Streptococcus pneumonia Group A and B streptococci Moraxella catarrhalis Escherichia coli Pseudomonas species |
Herpes simplex Adenovirus |
Blocked lacrimal duct Irritants |
Table One: Causative agents of Ophthalmia Neonatorum
The two major causes of infective neonatal conjunctivitis which should be excluded as priority are Chlamydia trachomatis and Neisseria gonorrhoea. Chlamydia is more common and presents later due to a longer incubation period, presenting 5 days to 2 weeks post-birth. By contrast, gonococcal conjunctivitis presents early, often within the first 24 hours of delivery until up to 5 days post-birth. Identification of either of these pathogens in a neonate will require discussion with the obstetrician or GP as well as with ophthalmology for follow up. They are discussed in more details in specific sections below.
Conjunctivitis is a clinical diagnosis that presents with inflammation of the conjunctiva causing conjunctival erythema, blood vessel dilation and tearing. It can involve the eyelid causing swelling and/or the cornea and lacrimal apparatus causing serous or purulent discharge.
Prompt diagnosis is key in establishing treatment and minimising potential complications. Time of onset varies with likely pathogen (Table 2).
|
|
Time of onset |
|
Non-infections |
First 24 hours Usually self limiting No treatment required |
|
Neisseria gonorrhoea |
Birth to 5 days Requires treatment |
|
Chlamydia trachomatis |
5 to 14 days Requires treatment |
|
Other bacteria |
4-5 days but can be any time Often self-limiting |
|
HSV |
1 to 2 weeks Requires treatment |
Table Two: Timing of onset
No conjunctival inflammation
If there is no conjunctival inflammation or other signs of infection then no antibiotics are required.
Advise regular cleansing of the affected eye(s) with sterile water or 0.9% saline, wiping from nose to outer aspect of eye in a single motion, discarding swab or cotton pad following this. A fresh swab or pad should be used if further cleansing is required. This should be done 4 to 6 hourly for 2 to 3 days. Daily firm massage of the nasolacrimal ducts is recommended: advise parents to use a clean index finger to press downwards on the side of the nose from the corner of the eye to the nostril.
If no improvement (discharge persisting for greater than 48 hours) delayed antibiotic prescription may be indicated. A swab must be taken prior to commencement of any antibiotic treatment and should be taken to include conjunctival cells and not exudate alone. Common organisms should respond to topical chloramphenicol, and both eyes should be treated. Gentamicin is not used for routine treatment as it may cause corneal toxicity and confuse the clinical picture.
Inflammation or purulent discharge
If the infant’s eye looks inflamed or if the discharge is purulent, empiric treatment with topical chloramphenicol eye ointment should be commenced pending culture. An extremely purulent discharge in the first few days of life should prompt consideration of Neisseria gonorrhoea (vide infra) . When a sticky eye has not responded to empiric antibiotic ointment, swabs should be sent to the virology laboratory to exclude Chlamydial infection.
The epidemiology of Neisseria gonorrhoea has changed over recent years and, although rare, rates have increased recently in the UK. Treatment has been complicated by increasing resistance to many antibiotics with a decreased susceptibility to 3rd generation cephalosporins and reported treatment failures.
Vertical transmission rates are high with positive conjunctival cultures occurring in 30-50% of cases. It is therefore prudent to treat prophylactically babies born to mums positive for gonorrhoea.
Presentation
Gonococcal conjunctivitis usually develops in the first 5 days after birth and is rapidly progressive; presentation in the second week suggests postnatal exposure. Most affected neonates have profuse purulent conjunctivitis and oedema of the eyelid (Figure 1), but some may have only a mild inflammatory response.

Figure One: Baby with gonococcal eye infection
Pharyngeal colonisation occurs in up to 15% of infants with gonococcal conjunctivitis and carries a risk of haematogenous spread to distal sites. Any infant with proven eye involvement should be assessed for evidence of joint, mucosal surface (rhinitis, stomatitis or anorectal involvement) or CNS infection. Blood and CSF should be obtained from an infant who is febrile or considered unwell.
Suspected or confirmed gonococcal infection in the neonate must be discussed with a senior member of the paediatric team.
Investigation
An urgent eye swab should be taken and URGENT gram stain requested, with preliminary results available and chased the same day. The presence of Gram negative diplococci is highly suggestive of gonococcal infection and should prompt treatment pending formal cultures. All eye swabs taken from babies less than 1 month sent to microbiology are routinely be tested for the presence of gonococcus.
Definitive diagnosis is made by subsequent bacteriological culture or Nucleic Acid Amplification Test (NAAT) (discuss with microbiologist). It is advisable to test for Chlamydia at the same time as both infections may be present (see below). Appropriate cultures should also be obtained from the mother if neonatal infection is suspected and/or confirmed. All eye swabs sent to the virus lab from babies of less than 4 weeks will be tested routinely for chlamydia, gonorrhoea, HSV, adenovirus and varicella by PCR. Gonorrhoea testing is not done automatically for those over 4 weeks and will need to be requested separately.
Treatment
- Ophthalmia neonatorum without systemic disease
Cefotaxime 100mg/kg, single dose, IV.
0.9% Normal Saline irrigation until eye discharge clears.
Topical therapy is unnecessary.
- Disseminated gonococcal disease
Cefotaxime 50mg/kg IV three times daily
Treatment should continue for 7 days (or 14 days if meningitis is suspected or proven).
Seek microbiology advice.
- Documented maternal infection: neonatal prophylaxis
Asymptomatic infants born to mothers with known disease should be treated with a single dose of Cefotaxime 100mg/kg IV after birth. If symptoms develop further assessment is indicated. If IV cannulation is considered to be difficult or challenging, then IM route of administration may be considered.
If cephalosporin resistance is suspected seek microbiology advice.
Complications
Corneal involvement with ulceration and scarring is a serious complication of neonatal conjunctivitis which can occur even with treatment and will result in visual impairment. Perforation can also occur
Chlamydia trachomatis is the most common, curable bacterial sexually transmitted disease in the UK affecting 3 - 6% of sexually active women in Scotland. Infection is often asymptomatic, and pregnant mothers are not routinely screened. Overall transmission rate at delivery is around 25%, ranging from 67% for vaginal delivery to less than 10% for infants born by caesarean section. Apparently successful treatment of the mother during pregnancy does not preclude neonatal infection.
When a mother is known to be infected with chlamydia, management of the infant should be expectant. In a symptomatic infant it would be reasonable to commence empiric treatment pending the result of eye swabs or NP secretions.
Presentation
Chlamydial eye infection often presents unilaterally and becomes a bilateral conjunctivitis. This may initially be serosanguineous but later becomes mucoid or mucopurulent in appearance. It is commonly associated with eyelid swelling and marked conjunctival injection (Figure 2). Onset is usually around day 5-14 but may be as late as 60 days. 10-20% of infected neonates develop pneumonia and infants may have feeding difficulties at initial presentation as a consequence of this.
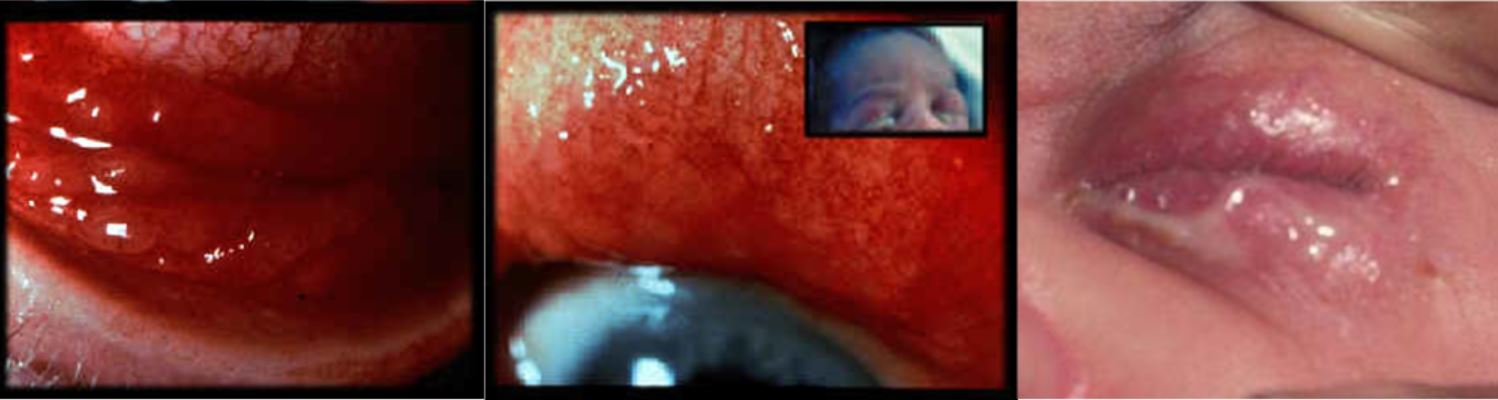
Figure Two: Infants with chlamydial eye infection
Investigation
Chlamydia is detected in conjunctival cells by NAAT. Cells should be obtained by firmly swabbing the everted lower eye lid using a virology swab which is then placed in VPSS transport medium. Samples should be sent to the virology laboratory at Glasgow Royal Infirmary. The laboratory will routinely test eye swabs for chlamydia, herpes simplex, adenovirus and varicella and results will generally be available in 48 hours.
Treatment
Systemic therapy is always required. Although topical therapy may be clinically effective for treatment of the eye infection, it does not eradicate nasopharyngeal carriage or prevent subsequent pneumonia. Systemic treatment is effective with eradication in 80-100% of cases.
First line: Oral erythromycin 12.5 mg/kg/dose, four times daily, 14 days
Second line treatment, oral azithromycin, 20mg/kg, once daily, for 3 days, may be considered if there are any substantive concerns regarding compliance.
There are limited data available on the use of other macrolides. Erythromycin has been associated with development of pyloric stenosis if used in infants under 6 weeks of age but is still the recommended treatment of choice. Parents should be advised of this risk and infants monitored closely following treatment.
Remember maternal screening and treatment will be required.
Complications
Symptoms may resolve spontaneously but infection in untreated or inadequately treated cases can persist for up to a year and may result in corneal scarring. Other systemic complications include pneumonitis, rhinitis and otitis.
Pneumonia
Chlamydial pneumonia presents as an afebrile respiratory illness with paroxysmal cough and wheeze. Symptoms can be very similar to viral bronchiolitis or whooping cough but infection may be atypical in preterm infants. Onset is usually between 2-12 weeks post delivery: antecedent conjunctivitis is not a prerequisite.
Investigations
Laboratory markers may show a marked eosinophilia and the CRP can remain normal.
Chest x-ray: hyperinflated with pulmonary infiltrates
NP or ET secretions should be collected in chlamydia transport medium. All NPAs sent in babies less than 1 month are routinely tested for chlamydia if all other virology is negative. Samples collected late in the day should be refrigerated overnight before being sent to the laboratory first thing in the morning. (NB. In the PRM, samples may be sent at any time via the pod system)
Treatment
Untreated the infection is self-limiting but it can last for several weeks even in term infants. Treatment shortens the duration of the illness. More severe disease can occur in premature infants and those with BPD. An association with reactive airway disease over 1st year of life is reported.
Erythromycin 12.5mg/kg/dose, four times daily, 14 days
Oral or I.V.
Failure rate is 20% and a second or third course of treatment may be required.
Herpes Simplex virus may present within the first two weeks of life in association with systemic herpes infection or local skin lesions. Signs include eyelid oedema, moderate conjunctival injection, and non-purulent and often serosanguineous discharge, which may be unilateral or bilateral. If suspected, refer to the guideline for the management of babies with Herpes Simplex and discuss diagnosis and treatment (aciclovir) with the virologists (call 0141 201 8722 or email west.ssvc@nhs.scot).
Obtaining samples for “test of cure” in ophthalmia neonatorum are not routinely recommended particularly when using NAAT tests as these may continue to detect non viable organisms for weeks after treatment.
SIGN. Management of genital Chlamydia trachomatis infection. A national clinical guideline. Scottish Intercollegiate Guidelines Network, March 2009. Edinburgh.
Yu J, Wu S, Li F, Hu L. Vertical transmission of Chlamydia trachomatis in Chongqing China. CurrMicrobiol 2009; 58:315-20.
McCourt, EA. Neonatal Conjunctivitis. Medscape.
Rours IG, Hammerschlag MR. Ott A. De Faber TJ. Verbrugh HA.de Groot R. Verkooyen RP. Chlamydia trachomatis as a cause of neonatal conjunctivitis in Dutch infants. Pediatrics 2008;121:e321-6.
Woods CR. Gonococcal infections in neonates and young children. Seminars in Pediatric Infectious Diseases. 2005;16:258-70.
Zar HJ. Neonatal chlamydial infections: prevention and treatment. Paediatric Drugs 2005;7:103-10.
Palafox et al. Ophthalmia neonatorum. J Clinic Experiment Ophthalmol 2011
Centers for Disease Control and Prevention (CDC). Sexually transmitted diseases treatment guidelines, 2010. MMWR Recomm Rep2010; 59(RR-12):1–110.
Nwokolo NC et al. 2015 UK National guideline for the management of infection with Chlamydia trachomatis. International Journal of STD & AIDS 2016; 27(4): 251-267
Zloto O et al. Ophthalmia neonatorum treatment and prophylaxis: IPOSC global study. Graefes Arch Clin Exp Ophthalmol: 2016; 254: 577-582
Doan T, Pinsky BA. Current and future molecular diagnostics for ocular infectious diseases. Curr Opin Ophthalmol 2016, 27:561–567
Last reviewed: 01 January 2023
Next review: 01 January 2026
Author(s): Dr Helen Mactier - Neonatal Consultant PRM
Co-Author(s): Reviewed (August 2017): Dr Emily Mullan. Neonatal GRID trainee, West of Scotland. Other specialists consulted: Dr Brian Jones – Consultant Microbiologist GRI ; Dr Fiona Thorburn - ST trainee (Microbiology); Dr Oliver Chadwick - ST4 Ophthalmology
Approved By: WoS Neonatology MCN

