TIVA can be used for GI endoscopy without the use of an endotracheal tube or LMA. This is a well-established technique in many paediatric centres worldwide with patient and procedural benefits including:
- Reduced recovery time
- Quicker resumption of oral intake
- Improved list turnover/throughput
- All the other benefits of TIVA!
However, careful patient selection is required. Contraindications include:
- Patients with GORD
- Patients with reduced gastric emptying
- Patients with active vomiting
- Some obese patients where oxygenation during this technique can be challenging
- Young patients (authors recommend caution if patient <5yr, low threshold for intubation)
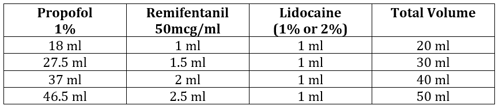
In general, the concentration of remifentanil is less than previously described for general anaesthesia. This helps to maintain spontaneous ventilation in the face of reduced procedural stimulation once the endoscope is inserted.
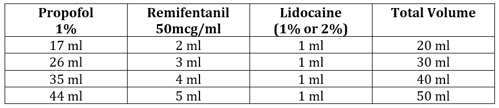
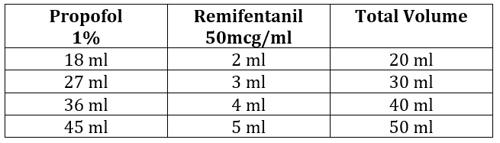
To achieve a solution of 1% propofol with 2.5 micrograms / ml of remifentanil:
- 1mg of remifentanil is diluted in 20ml 0.9% sodium chloride, giving a concentration of 50 micrograms / ml
- 2.5ml of this remifentanil is added to 47.5ml of 1% propofol
Lidocaine is either added to the pump or directly to the vein after cannulation. This choice is one of personal preference, but the authors do recommend the use of lidocaine to reduce pain on induction.
Induction
Although desirable, IV induction is not essential. If required gas induction can be achieved and then TIVA commenced after cannulation. Care must be taken to ensure depth of anaesthesia is maintained as the sevoflurane is washing out and the TIVA is reaching Ce.
If induction is IV, commence infusion at a Cpt of 3.0 mcg/ml and assess response. In older children you may have to titrate to 6-7 mcg/ml before loss of verbal contact.
Apply a gentle jaw thrust and assess response: increase Cpt by 0.2 mcg/ml until jaw thrust tolerated and patient has a stable respiratory pattern. General guide is to aim for a respiratory rate half of normal baseline in younger children or <15/min in adolescents.
How to oxygenate
Preference is to use the anaesthetic face mask initially, but once the patient is asleep with a stable respiratory rate, high flow nasal cannulae are applied and flow commenced as per HFNO guide (attached to Optiflow machine).
Keep the face mask handy and discuss with your assistant the size of ETT you will require should your airway management plan change during the case.
Patients may require basic airway manoeuvres if evidence of obstruction occurs. Insertion of a bite block should be considered to protect the endoscope.
Maintenance
Keep IV access visible and accessible and the TIVA pump near you. Open the airway for the OGD. If there is evidence of insufficient depth of anaesthesia increase Cpt by 0.2mcg/ml and allow equilibrium. Placing the face mask on the chest/abdomen allows for improved visualisation of the respiratory pattern and ensures you know where it is should you require it quickly!
Emergence
Continue to oxygenate the patient and transfer to recovery.
All intravenous cannulae MUST be flushed prior to leaving theatre.
The flushing MUST be documented on the anaesthetic record.
The flushing MUST be verbally handed over to recovery staff.





 Figure 4. Button on Alaris PK pump to change pump pressure alarms
Figure 4. Button on Alaris PK pump to change pump pressure alarms