Children with cancer or associated disorders may be referred by primary, secondary or tertiary care. Appropriate investigations to establish the correct diagnosis and stage of disease is the responsibility of the consultant.
Similarly it is the responsibility of the child’s consultant to arrange all necessary investigations to monitor response to treatment, including any toxicities and to investigate suspected or confirmed relapse. Each new patient will be discussed at the disease specific MDT where the diagnosis will be confirmed and treatment agreed. These decisions are recorded on a proforma which is signed off and filed in the patient’s case record. A copy is sent to the patient’s GP. Patients are re-discussed at the MDT at the time of relapse or following any event which might require a change of treatment. They are also discussed at disease specific weekly on-treatment meetings with particular emphasis on toxicities and chemotherapy planning/ordering.
It is the responsibility of each consultant to obtain informed consent for treatment for all patients irrespective of whether the patient is on or off trial.
As per CEL 30 (2012) all staff involved in SACT must have the appropriate skills, knowledge and training in their field of practice. Evidence of this training is documented in each staff member’s training record and must include the following:
- principles of safe use and relevant national guidance
- local policy and procedures on safe use
- principles of SACT
- CMGs and SACT protocols relevant to area of clinical practice
- consent and information giving
- holistic assessment of patients receiving SACT
- prevention and management of adverse effects
- selection and use of equipment
- safe handling of cytotoxic chemotherapy
It is also a consultant responsibility to allocate treatment and to ensure that the relevant up to date treatment protocol is available. Copies of all protocols and guidelines are maintained by the Clinical Trial Coordinators.
All children are treated on NCRI trials if these are open for their particular disease. In the absence of a clinical trial they will be treated on a national guideline. The exceptional child with an extremely rare disorder may be treated according to best practice. The diagnosis and treatment with expected benefits, outcomes and risks are explained to the parents/child.
Written trial specific and age-appropriate information is given to the parents/patient and following an appropriate period of time to allow parental/patient understanding, written consent is obtained. The information given is noted on the CR-UK consent form.
Consent will be documented on a generic consent form for all patients (this will be on the generic CR-UK form or the ALL specific consent form) and in addition on a trial specific consent form if recruited to a clinical trial. Patients who are initially consented before the age of 16yrs will be re-consented when they reach their 16th birthday.
The site file for each trial will list the medical practitioners who can take consent (ie Consultant/HSCT Associate Specialist). Patients/parents/carers for whom English is not their first language will be offered the services of an interpreter at the time of diagnosis, when consent is taken, and later as required.
All patients will be assessed by a doctor or ANP immediately prior to receiving chemotherapy. This assessment will include general fitness for chemotherapy, performance status (PS), necessary critical tests and the presence of associated toxicities.
The results of any clinical test required prior to chemotherapy commencing, PS and grading of any toxicity / co-morbidity MUST be completed and signed off by the doctor/ANP prior to authorising any new course of chemotherapy. Haematological toxicity does not have to be completed for patients with acute leukaemia/lymphoma during maintenance treatment when blood counts are reviewed regularly and doses of chemotherapy titrated accordingly
In the very rare circumstance where a chemotherapy trained doctor or ANP is not available to authorise a patient’s treatment a member of the Schiehallion medical team can sign the authorisation, but only after discussion with a Consultant. This must be clearly documented on the prescription and the entry must be counter-signed by the Consultant at the earliest opportunity.
The medical practitioner will have received structured education on the principles of chemotherapy. They will have completed induction training within the unit and will have been deemed competent prior to prescribing cytotoxic drugs. Consultants, speciality doctors and trainees of ST4 level and above will prescribe chemotherapy and only after appropriate training. However, Clinical Fellows who are already familiar with the Unit may also be permitted where appropriate (see HAEM-ONC-036) and also specific nursing staff can prescribe maintenance SACT (see section 6.3).
This SOP assumes that local practices and policies for education are implemented and carried out within the haematology/oncology unit and that adherence to these will be regularly monitored, audited and updated.
The individual practitioner must be familiar with, and adhere to, related policies and protocols noted in section 8 – Related Documentation.
Intrathecal cytotoxic drugs will only be administered by doctors of ST4 level and above, staff in non-Consultant Career Grades and Consultants who have Division certification and are listed on the intrathecal register. Clinical Fellows who are already familiar with the Unit may also be trained where appropriate (see HAEM-ONC-036).
NB: Doctors in training will not administer bolus vinca alkaloids by peripheral venous access. This will only be done by SACT Intravenous bolus trained nursing staff.
Written informed consent for treatment must be taken at an appropriate period of time after the patient/parent has been provided with verbal and written information, which includes the potential risks and anticipated benefits.
This information should be provided by the Paediatric Consultant Haematologist or Oncologist responsible for starting or initiating the next course of SACT and, following this discussion, the Consultant should sign off Box 1 on Page 4 of the generic consent form (HAEM-ONC-TEMP-002) “Health care professional obtaining consent”.
6.1 Initial Treatment Decision and Consent
- The initial decision to treat a patient with SACT and the selection of the SACT protocol must be made by a Paediatric Consultant Haematologist or Oncologist. The ALL form should be used for leukaemia patients and the paediatric form should be used for all other patients.
- Informed and written consent must be obtained after relevant verbal and written information have been provided. Box 1 on Page 4 of HAEM-ONC-TEMP-002 must be signed by the Consultant. It was agreed by the Consultant group that Box 2 will be left blank/unused as consent is verbally confirmed with the patient/carer by the nursing team prior to the SACT course commencing and any questions raised would be directed to the Consultant. Where oral SACT is issued to a patient/carer by a pharmacist they will check consent as per same procedure.
- The decision to treat must be documented in the patient notes.
- The treatment plan, a copy of the treatment protocol and flowsheets (signed and dated by Consultants) must be filed in the patient’s shadow notes prior to SACT administration and copied to the extended scanning folders (see section 3.5). This information must also be communicated to the GP by the CTC or Research Team using the generic GP letter and trial GP letter template (where appropriate). This must take place within 14 days of diagnosis where possible or, at a minimum, within 14 days of first discharge.
- The performance status and any co-morbidities at diagnosis must be documented in the patient’s notes. In patients with a poor performance status the rationale for treatment should be clearly documented as well as any additional monitoring arrangements in a patient specific treatment plan.
- The protocol or guideline must be clearly documented in the patient’s records by the Paediatric Haematologist or Oncologist
- All SACT drugs to be administered, as directed by the protocol or guideline, must be included on the consent form. Drugs on the consent form must match the drugs given and the trial name must also be included.
- Consent to chemotherapy will be checked by the Clinical Trial Coordinator or Admin Assistant before being scanned onto Clinical Portal (under the Research tab).
- Where electronic case records are being used a summary of the diagnosis, treatment protocol and associated supportive care must be added to the appropriate e-form on Clinical Portal.
6.2 SACT Protocol
- The treatment protocol or guideline should contain the following information:
- Eligibility and exclusion criteria
- Drugs, doses, scheduling, number of cycles and supportive care
- Dose modifications (see Section 7)
- Critical tests required prior to each course or cycle
- Potential toxicities
- Frequency of disease evaluation
6.3 Prescribing
Medical Prescribers
Only a doctor of ST4 and above who has completed the appropriate medical training on chemotherapy can prescribe SACT. However, where appropriate Clinical Fellows who are already familiar with the Unit may be permitted (see HAEM-ONC-036).
Independent Prescribers
Hydroxycarbamide and oral maintenance chemotherapy can be prescribed by named SACT trained nurse prescriber (see below):
- Wendy Taylor & Judy Taylor, Advanced Nurse Practitioners (Hydroxycarbamide)
- Wendy Taylor & Jane Baird, Advanced Nurse Practitioners (oral maintenance chemotherapy)
Guidance for all prescribers:
- SACT prescribers must have access to all relevant protocols and guidelines to support safe and appropriate prescribing (see Section 7)
- SACT prescribers must have access to relevant individual patient information on previous modifications to SACT prescriptions (see Section 7).
- The patient must be assessed for adverse effects at appropriate intervals as determined by the trial protocol. . These must be graded using the appropriate CTCAE criteria and documented appropriately on either the chemotherapy template prescription or on the toxicity tab on ChemoCare. In addition to required adverse events, SAEs and SARs should be reported to the sponsor as directed in the protocol.
All unexpected adverse drug reactions should be reported to www.mhra.gov.uk/yellowcard . In addition, all adverse events occurring in patients not treated on trial will be discussed at the daily handover and the event and management of the SAE will be recorded in the patient’s electronic record. Those requiring treatment modification will be recorded on the treatment plan within the shadow notes (CTC will copy to the extended scanning folders as per section 3.5).
- The performance status must be assessed and recorded prior to each course of chemotherapy
- Appropriately trained medical staff at ST4 level and above, staff in a non consultant career grade, and Consultants, will prescribe SACT. However, where appropriate, Clinical Fellows who are familiar with the Unit may be permitted (see HAEM-ONC-036). Additionally there are specific nursing staff who are able to prescribe maintenance SACT (see section 6.3).
SACT should be prescribed electronically on ChemoCare wherever possible. Standardised templates can be used if electronic prescriptions are unavailable, however, these must be fully validated. All SACT prescriptions should comply with current legal requirements and local prescribing policies. Prescriptions must be written in a clear and unambiguous manner and include:
- name, date of birth, CHI
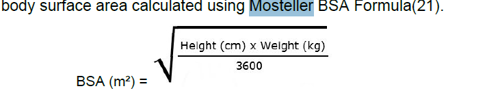
- recent weight (two weights and heights if first course)
- diagnosis
- name of protocol
- cycle number and date of intended treatment
- performance status and toxicity score at the start of each course
- relevant critical tests
- generic names of each drug and calculated doses to be administered
- route and duration of administration
- diluents and infusion volumes where appropriate
- hydration schedules and pre-medication if required
- appropriate supportive care
- a record of any dose modifications (see Section 7)
- indication of concomitant radiotherapy where applicable
- signature of prescriber and date prescription is written or generated (these may be electronic if on ChemoCare)
- signature documenting pharmaceutical verification and date
- signature documenting administration and date
NB: The initial decision to administer cytotoxic chemotherapy is made by an accredited haematology/oncology consultant or an appropriately trained and competent nominated deputy and the decision must be CLEARLY recorded in the patient’s CLINICAL notes.
NB: A validated electronic chemotherapy prescribing system is operating within the Schiehallion Unit. All protocols will in time be available electronically. IN THE EVENT OF A SYSTEM FAILURE, STAFF WILL REVERT TO PAPER based PRESCRIBING as per the contingency sop
6.4 Out of hours
In the absence of medical staff of appropriate grade on site, minor changes to prescribed/scheduled intravenous chemotherapy (such as date/time ) can be made by ST3 medical staff after authorisation from the consultant on call and in consultation with the nurse in charge of the unit. Treatment must be countersigned on the ward prescription chart the next day by the consultant.
In the exceptional circumstances emergency chemotherapy is required out of hours, the requesting consultant will contact the on-call pharmacist who will liaise with a Cancer Care Pharmacist and the out of hours Pharmacy Aseptic Team as per the GG&C Out of Hours Supply of SACT policy.
6.5 Deferring of Chemotherapy
It is very important to record the reason for any deferral of chemotherapy courses. This should be documented in the appropriate section at the front of the chemotherapy template prescription or electronically on ChemoCare. The reason for the deferral and the next intended treatment date will be recorded within the SACT prescription.
If any chemotherapy course is delayed for more than 7 days the patient’s consultant must be informed. If a deferral results in a modification to the intended course of treatment the prescription must be prescribed.
Any change to a prescription must be clearly annotated and signed by an appropriate chemotherapy prescriber and the reason documented on the prescription. Any major change must also be documented on the patient treatment plan which is held within the patient’s shadow notes and copied to the extended scanning folders (as per section 3.5). New major modifications are highlighted at the weekly on-treatment meetings, updated within the treatment plan in the shadow notes and copied to the extended scanning folders.
Any modified/rewritten prescriptions must be given to the appropriate clinical pharmacy team for rescreening.
Any deferral of chemotherapy must be completed on the appropriate prescription (template or ChemoCare) by a member of the clinical team who has reviewed the patient and made the decision to defer.
Within the Schiehallion Ward this must be a chemotherapy trained member of medical staff or ANP. Within DCU this can be a chemotherapy trained member of medical staff, ANP, senior nurse in charge or paediatric oncology outreach nurse specialist.