Endo-Tracheal tubes (ETT) form artificial airways which bypass the normal physiological processes providing an easy route for microbial invasion (Day et al, 2002, Stokowski, 2009). Poor or absent cough caused by sedation, paralysis or disease can result in impaired secretion clearance leading to lung collapse, consolidation and ventilator associated pneumonia (VAP) (Paratz and Stockton, 2009). Therefore, endotracheal suction is essential to prevent airway obstruction whilst optimising oxygenation and ventilation (Morrow et al, 2006, Hannes et al, 2005).
Suctioning can be described as the mechanical aspiration of secretions from an artificial airway (Edmunds and Scudder, 2009, Day et al, 2002). Paratz and Stockton (2009) suggest that suctioning of a tracheal tube is one of the most common procedures performed within a Critical Care setting. However this procedure is associated with numerous potential complications (Trevisanuto et al, 2009, Edmunds and Scudder, 2009, Perinat, 2005, Morrow et al, 2006).
Complications of Endo-tracheal (ET) Suctioning:
- Bradycardia due to vagal nerve stimulation
- Hypoxemia
- Pulmonary hypertension
These complications include; bradycardia due to vagal nerve stimulation; hypoxemia which may result in cardiovascular instability leading to hypotension and even cardiac arrest; pulmonary hypertension; raised intracranial pressure (ICP); bleeding caused by mucosal trauma; infection; atelectasis; bronchospasm; and severe anxiety and distress to the patient which can result in a cardiovascular stress response or accidental extubation (Penderson et al, 2009, Paratz and Stockton, 2009, Day et al, 2002, Rieger et al, 2005, Edmunds and Scudder, 2009, Morrow et al, 2006, Morrow and Argent, 2008).
Tracheal suction should only be performed when necessary (Edmunds and Scudder, 2009) and not as a routine intervention (Day et al, 2002) but following a comprehensive clinical assessment (Morrow and Argent, 2008).
Indications for Endo-tracheal suction include:
- visible secretions in tracheal tube
- audible secretions on auscultation
- patient coughing
- increased work of breathing
- Reduced oxygen saturations
- Increased carbon dioxide level
- Following chest physiotherapy
- The presence of a saw tooth pattern in pressure volume waveform
- Decreased tidal volumes
- Suspected aspiration of gastric or upper airway secretions
Contraindications of Endo-tracheal suctioning:
- Unexplained haemoptysis (the coughing up of blood from the lungs or bronchi) or known clotting disorder
- Laryngospasm (stridor)
- Bronchospasm
- Basal skull fractures and other causes of cerebrospinal fluid leakage via the ear
- Pneumothorax
- Recent oesophageal or tracheal anastamoses (the joining of the branches of two blood vessels) and other forms of tracheobronchial trauma
- Occluded nasal passages
- Unexplained nasal bleeding
- Severe hypoxaemia / hypoxia
- Raised intracranial pressure
- Acute hypo or hypertension (ACPC, 2015)
Suctioning should not be carried out if any of the above contra-indications are present unless assessed on an individual basis and with the agreement of the medical team.
In preparation for the suctioning event, pre-oxygenation can be performed via mechanical ventilation in order to prevent suction induced hypoxia (Morrow and Argent, 2008, AARC, 2010). Particularly for those patients who have low oxygen saturations or increased work of breathing should be considered to pre-oxygenate. Post-oxygenation using the same method as pre-oxygenation can also be performed via mechanical ventilation following the suctioning event, if the patient subsequently has low oxygen saturations or increases work of breathing (AARC 2010). This method of pre-oxygenating mechanical ventilation can be used in both open and closed Endo-tracheal suctioning procedures. Hand bag ventilation can also be given by a competent practitioner in the case of open endo-tracheal suction procedure only.
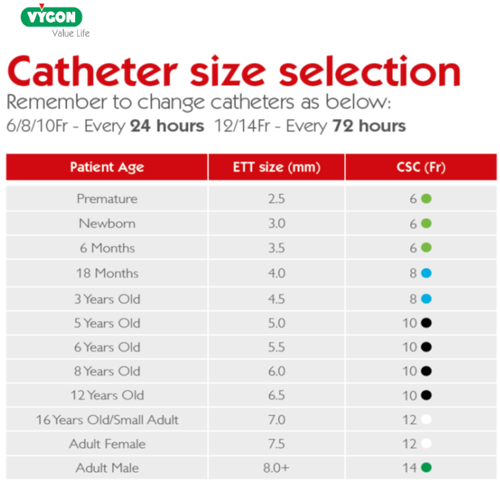
For open suction, suction catheter selection is determined by doubling the internal diameter of the tracheal tube (Morrow and Argent, 2008, Day et al 2002, APCP, 2015), table 1. For close suction circuit, it is dependent on the manufacturer what size is selected for size of Endo-tracheal Tube. In PICU, the current manufacturer of close suction catheter system used is Avanos (See table 2).
Table 1. Open suction catheter size selection
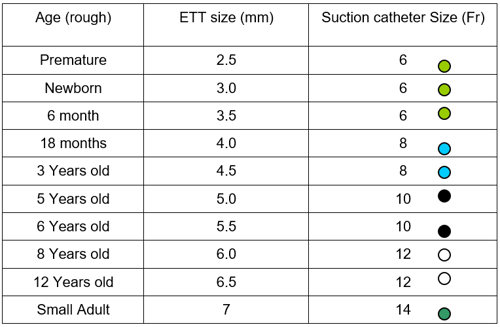
Table 2. Closed Suction catheter (CSC) size selection
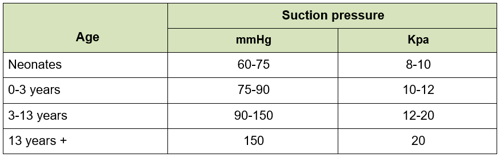
Suction vacuum pressure should be set as low as possible to effectively clear secretions and increasing as required up to a set maximum pressure that is dependent on the age of the child (see table 3).
Table 3. Suction Vacuum pressure
There are no known benefits to performing deep tracheal suction which is related to an increased risk of mucosal trauma and other adverse events (Morrow and Argent 2008, Spence et al 2009, AARC 2010) therefore AARC (2010) advocate shallow suctioning in order to reduce these risks. Morrow and Argent (2008) recommend that the suction catheter should only be passed to the end of the endo-tracheal tube which can be determined by direct measurement (i.e. closed circuit suctioning). Deep suction should only be performed if the patient is retaining secretions and closed circuit suctioning has not been effective at clearing. Deep suctioning should be kept to a minimum to avoid risk of mucosal trauma. Consider referral to chest physiotherapist if the patient is retaining secretions and requiring deep suction regularly.
It is hypothesized that normal saline instillation may loosen secretions, increase the amount of secretions removed, and aid in the removal of tenacious secretions however there is insufficient evidence to support this hypothesis (AARC 2010). Caruso et al (2009) believe that normal saline instillation prior to tracheal suction may be associated with decreased incidence of microbiological proven VAP. However, the majority of authors do not consider the instillation of normal saline to be beneficial and may actually be harmful to patients (Edmunds and Scudder 2009, Kuriakose 2008, Rauen et al 2008, Day et al 2002, Morrow and Argent 2008, Halm and Krisko-Hagel 2008, Ridling et al (2003). Therefore, instillation of normal saline prior to tracheal suction should not be routine practice (AARC 2010, Kuriakose 2008) but may be useful in certain instances or with chest physiotherapy (Paratz and Stockton 2009). Effective humidification of the ventilator circuit prevents the build-up of thick, tenacious secretions thus reducing the need for instillation of normal saline (Halm and Krisko-Hagel 2008, Ridling et al 2003).