Oral hygiene is a fundamental aspect of nursing care and significantly affects the health and well being of the individual. In paediatrics, oral hygiene is essential for the development of healthy teeth and to minimize the risk of infection. In children tooth development begins in utero with the first teeth, known as the deciduous or milk teeth, erupting at around 6 months of age. Permanent teeth then begin to erupt between the ages of 6 to 12 years of age with the final permanent teeth erupting at 17 to 25 years of age. Teeth act as hosts for dental plaque, which in turn acts as a host for harmful pathogens.1
Dental plaque is the accumulation of mainly oral micro-organisms and their products on the surface of the tooth and surrounding soft tissues. Normally, oral health is maintained by regular eating and drinking, regular maintenance such as tooth brushing and by saliva production. Saliva plays a vital role in cleansing the mouth. It keeps the mucous membranes moist, it regulates the pH of the mouth and aids in the digestion of food. 2 Furthermore, saliva contains natural antimicrobial proteins that protect the mouth against invading pathogens and contributes to the formation of a biofilm or pellicle, which acts as a protective layer on teeth.3
Poor oral hygiene leads to the accumulation of dental plaque and dental caries, and the development of gingivitis. In paediatric critical care, poor oral hygiene and the resulting increase in dental plaque, is associated with an increase in bacterial colonisation of the oropharynx and a higher risk of ventilator-associated pneumonia (VAP).4,5,6 VAP has been documented as being the second most common hospital acquired infection in paediatric intensive care patients and is associated with increased length of paediatric critical care stay and increased morbidity.7 In Paediatric critical care, the risk of VAP is increased due to the placement of an endotracheal tube, especially an uncuffed tube, which provides a pathway for bacteria into intubated child’s lungs.4,5,8 .
In addition, the acutely or critically ill infant or child may not be able to maintain oral hygiene and normal saliva production due to a number of factors, including the use of sedation, fluid restriction, nil fluid or diet orally and the administration of medicines that can exacerbate xerostomia, thus further increasing the risk of VAP.1,9
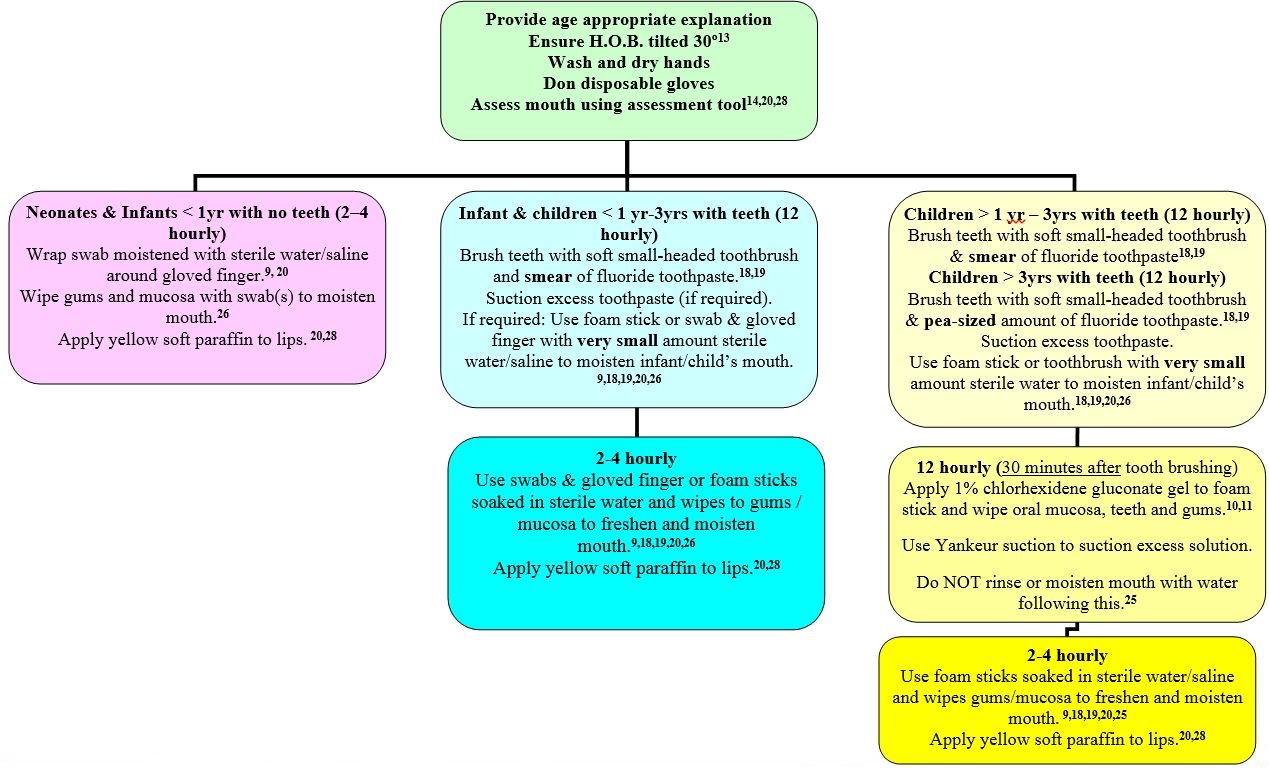
Research suggests that by improving oral hygiene and introducing a VAP prevention care bundle in vulnerable patients, bacteria in the oropharynx can be reduced, which will further impact upon the incidence of VAP.6,10,11 In addition, good oral hygiene will improve the overall comfort and well-being of the child. The nurse caring for those at risk infants and children should be aware of the need to provide comprehensive oral hygiene for the infant or child using appropriate oral assessment methods (Appendix 1 Paediatric critical care unit oral assessment tool) and evidence-based oral hygiene procedures and care bundles.12,13