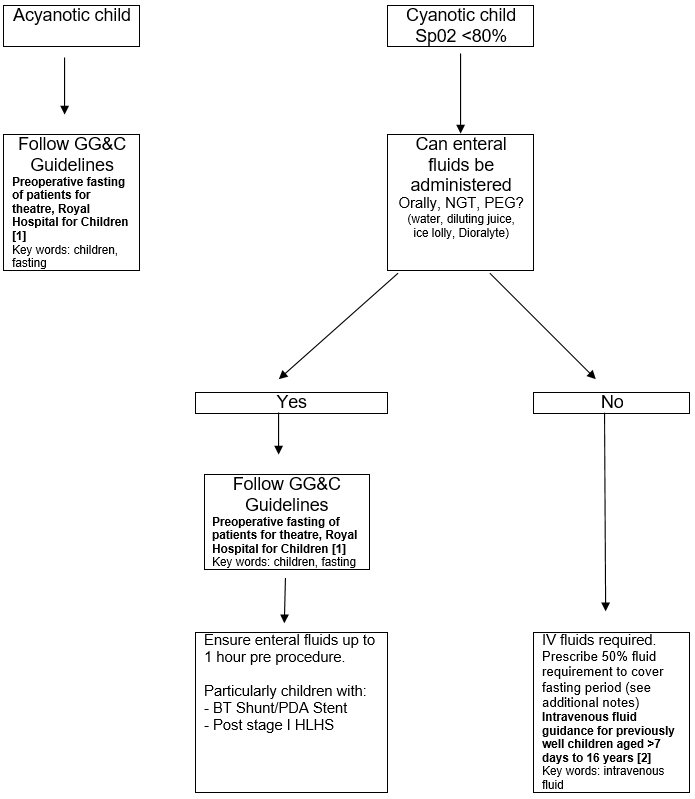
Children with congenital heart disease may be cyanotic, this causes an increase in erythropoietin thereby raising haematocrit, haemoglobin and blood viscosity.
Hyperviscosity is associated with stroke especially in young children in the presence of dehydration and so all children with cyanosis should have fasting kept to a minimum.