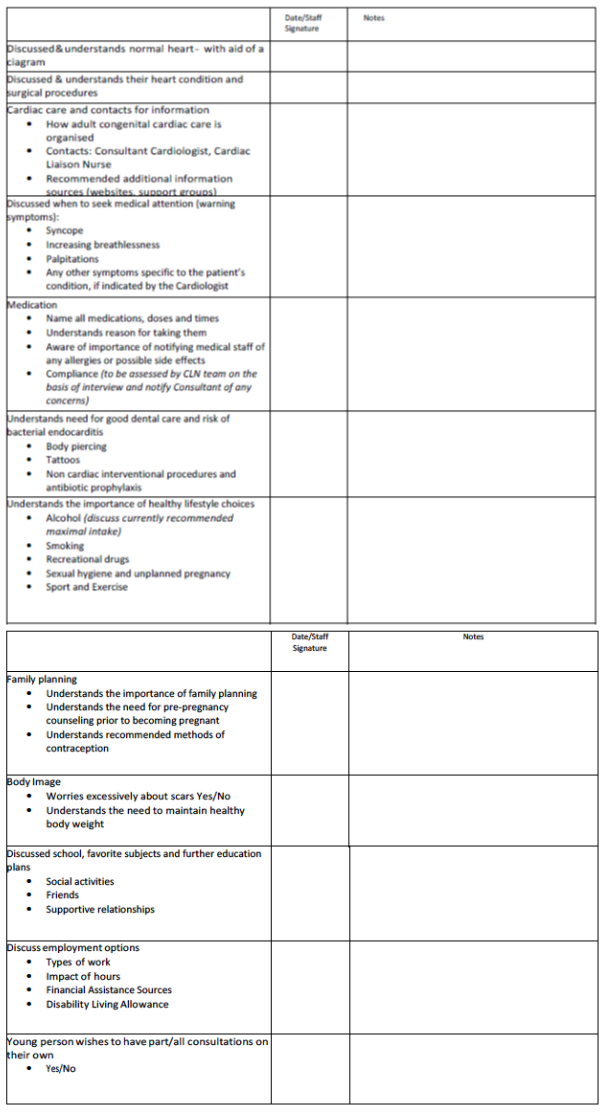
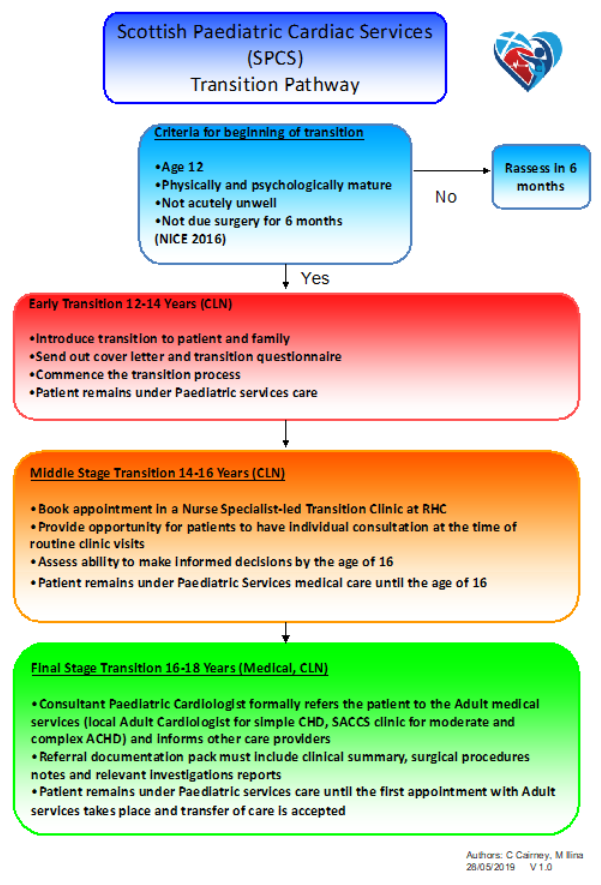
The aim of a transition service is to empower the young person and provide them with the necessary skills to take over responsibility for their healthcare needs. Transition services should be designed with a family-centered approach working with all members of the family, as stakeholders, to prepare the young person for this process and for transfer. This process starts in the pediatric services at approximately 12 years of age (this may be adjusted according to the individual patient’s care requirements) and continues within the adult services long after the patient’s medical care has been transferred. In practice, this support continues until the time of physiological brain maturation at or around the age of 25 years and is sometimes described as “Emerging Adulthood”.2, 3
Several studies have described a high proportion of patients having significant lapses in care during adolescence.6,7 Patchy provision of specialist transition and tailored adult services contributes adversely impacts on outcomes.5 This is true even for patients with complex congenital heart disease. Sub-optimal transition is associated with an increase in lost-to-follow-up rates and to poorer psychological adaptation to chronic health issues. In contrast, the establishment of transition care pathways improves continuity of care and may positively influence other outcome measures such as hospitalisation.8
The leading principle of transition being a process starting when the patient is still well within the paediatric age group, and completing in adult services in early to mid-twenties, distinctly separate from the event of medical care transfer between paediatric and adult services, underpins the guidance document below.
Benefits of effective transition
The importance of an effective transition programme goes beyond simply ensuring medical continuity of care. Knowledge deficits, even in long-term clinic attendees are frequent in young people with heart disease, impacting on successful transition to adulthood.10 Delay in achieving psychosocial milestones is also common in chronic illnesses. There is, therefore, a pressing need for all patients to be empowered to understand their heart condition and make informed decisions about their future health, occupation and lifestyle. Effective transition needs to employ multiple communication modalities to conform to individual preferences, as no two young people are the same.
The transition process has to address the evolving needs of parents, enabling them to be good advocates for their children with appropriate levels of protectiveness and support. Any discrepancies between professional and parental perspectives12, in addition to those between parent and adolescent, need to be acknowledged and sensitively negotiated. For some patients, the ability to attend clinic appointments without their parents positively affects attendance5. Promoting active involvement of the young patient during the consultation helps foster an environment of trust and enables parents to gradually withdraw from being an equal stakeholder and evolve into a more supportive role.
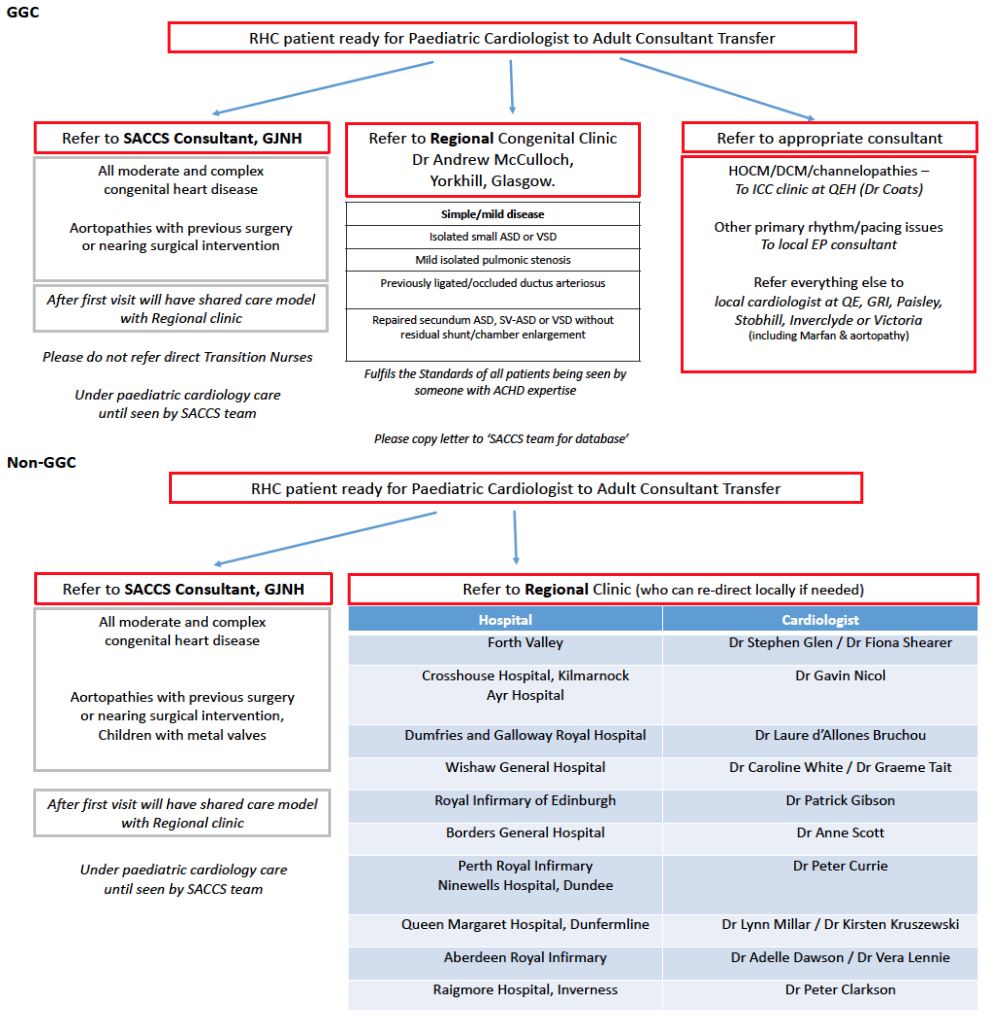
Transition and Transfer Model
A recent multi-centre study13 has demonstrated the effectiveness of a nurse-led transition programme, working in parallel with and acting in a complementary way to the medical congenital cardiac care. The primary focus of the nurse-led Transition Service is patient and family education and empowerment of a young person to gradually assume responsibility for their own healthcare decision and function in an adult environment.
Key principles as outlined in NICE Guidelines14
- The transition process should have the young person’s interests at the centre and should serve to meet the needs of the individual involved
- Transition support must be appropriate in terms of developmental and emotional maturity, social and personal circumstances
- Both the young person and caregiver, where appropriate, should be involved in the planning and decisions about the transition process. The aim of this is that the young person takes responsibility for their own health and has the skills to make informed choices and decisions about their health and wellbeing both now and in the future. National Service Framework for Children, Young people and Maternity Services (2004), Standard 415