Nasal injuries
exp date isn't null, but text field is
November 2023: This guidance is currently under review as it has gone beyond the standard review date. It reflects best practice at the time of authorship / last review and remains safe for use. If there are any concerns regarding the content then please consult with senior clinical staff to confirm.
Establish the mechanism of injury. Establish whether this is an isolated nasal injury or if there is associated head trauma ( see HI guideline), or injury elsewhere. If you have suspicion of NAI discuss with senior. Multiple facial injuries should increase the index of suspicion that an injury is inflicted.
The initial management of the child is dependant on their condition, using an ACBCDE approach. In terms of the nose injury itself:-
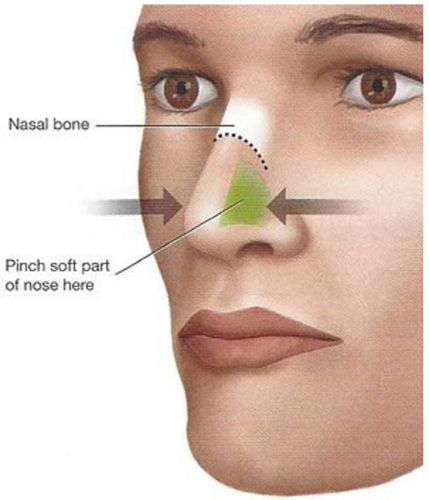
Control epistaxis if present [See Epistaxis Management in Children Guideline]
The majority of nose bleeds will stop with 10-30 minutes of firm pressure upon the soft tissues of the nose, compressing Little’s area, on the anterior septum. The nose should be held for 10 minutes initially, resisting temptation to release and see if bleeding has stopped. Ideally the child should sit upright with head tilted forward, spitting out blood that collects in their mouth.
If bleeding persists obtain IV access and send bloods for FBC, group and save, and coagulation. It is rarely necessary to pack a child’s nose. If bleeding persists despite a firm hold of adequate duration seek ENT advice.
Examination in nose injuries must include inspection of the nasal cavities. Look for and document-
- Septal haematoma – this can cause cartilage damage – aseptic necrosis- or can lead to abscess formation. Abscess formation is also associated with cartilage damage, and sometimes complicated by meningitis, or cavernous sinus thrombosis. If there is a septal haematoma present refer to ENT at initial presentation. Septal haematomas can present days after the nasal injury. If there is a delayed presentation associated with systemic features, particularly elevated temperature, a septal abscess should be suspected.

- Septal deviation- refer to ENT at initial presentation.
- Associated facial bone fracture e.g orbital rim fracture, maxilla fracture. If facial bone fractures are suspected discuss with maxillary facial registrar. Facial views are rarely performed in children, and are not performed without discussion with the maxillary facial service. CT of the facial bones may be required. This would usually follow maxillary facial review.
- Associated skull fracture- e.g. base of skull # which can lead to CSF rhinorrhoea. If skull fracture is suspected patient should be discussed with the ED consultant on call to arrange imaging.
- Patency of nares
- Evident deformity- if present refer to the emergency ENT clinic within one week of the time of injury.
- Swelling +/- contusion
Nasal injuries should not be followed up in ED clinic. If there is minimal swelling and no deformity, thus no suspicion of fracture, patient can be discharged with HI and Nasal Injury leaflet.
If at the time of examination swelling prevents confident assessment of deformity ask parents to look at the nose in 3-4 days time when the swelling has improved, and return to the emergency department for review if they have ongoing concerns. Ask parents to return between 9am and 1pm, Monday to Friday to facilitate follow up arrangements or ENT review if required. It is necessary to ensure that once swelling has settled there is no deformity, and that both nostrils are patent.
Deformities are ideally manipulated before the nose has healed in its altered position, so it is important to stress to parents to look at their child’s nose once swelling subsides and seek review in a timely fashion if concerned. Ensure parents have discharge leaflet re nasal injury.
If there is strong clinical suspicion of a fracture, but no immediate intervention required, patient should be referred to emergency ENT clinic within one week of the initial injury for assessment once swelling has subsided.
- Kidd AJ, Beattie TF, Campbell-Hewson G. Facial injury patterns in a UK paediatric population aged under 13 years. Emerg Med J 2010;27:603-606
- Haug RH, Foss J. Maxillofacial injuries in the pediatric patient. Oral Surg Oral Med Oral Path 2000;90(2):126-134
- Ryan ML, Thorson CM et al. Pediatric Facial Trauma: A Review of Guidelines for Assessment, Evaluation and Management in the Emergency Department. The Journal of Craniofacial Surgery 2011;22(4):1183-1189
- Middleton P. Epistaxis. Emergency Medicine Australasia 2004;16:428-440
- Olsen KD, Carpenter III RJ, Kern EB. Nasal Septal Trauma in Children. Pediatrics 1979;64(1):32-35
- Desroriers AE, Thaller SR. Pediatric Nasal fractures: Evaluation and Management. The Journal of Craniofacial Surgery 2011;22(4):1327-1329
- Alvarez H, Osorio J, Diego JI, Prim MP, De La Torre C, Gavilan J. Sequelae after nasal septum injuries in children, Auris Nasus Larynx 2000;27:339-342
Last reviewed: 10 November 2016
Next review: 30 April 2024
Author(s): S Sweeney
Approved By: Clinical Effectiveness
Reviewer Name(s): Paediatric Clinical Effectiveness & Risk Committee

