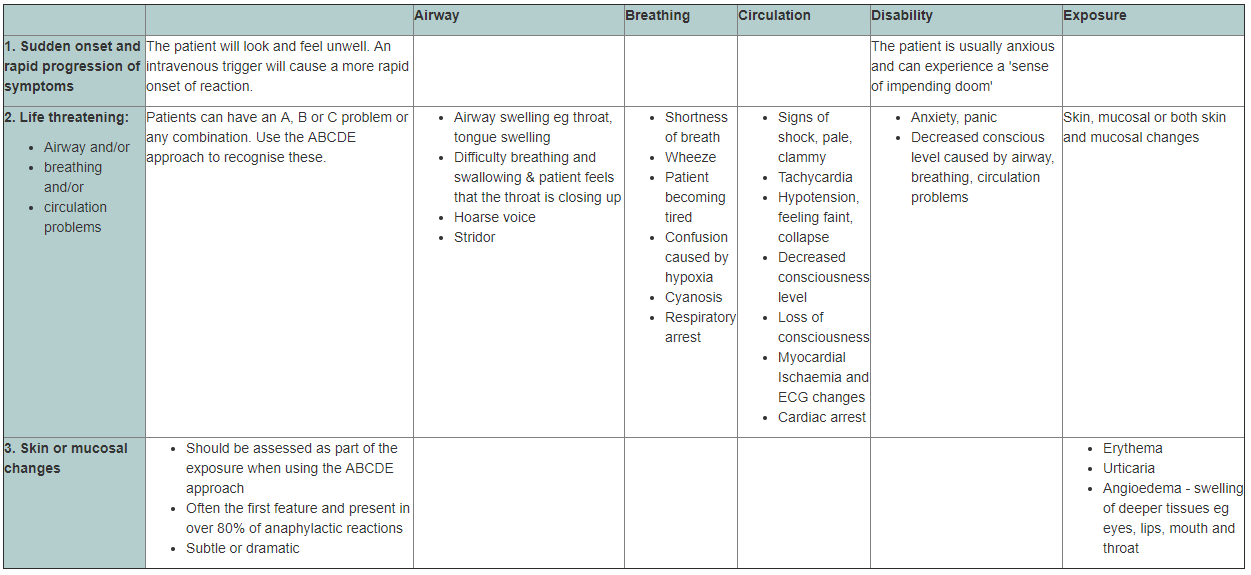
There is no universally agreed definition of anaphylaxis and the following definition is offered by the European Academy of Allergology and Clinical Immunology Nomenclature Committee: ‘Anaphylaxis is a severe, life-threatening, generalised or systemic hypersensitivity reaction’. This is characterised by rapidly developing lifethreatening airway and/or breathing and/or circulation problems usually associated with skin and mucosal changes (Resuscitation Council - 2008)
Anaphylactic Response:
- A hypersensitivity reaction can occur when the immune system is provoked by an antigen such as a cytotoxic drug, stimulating the formation of certain IgE antibodies that attach to receptors on mast cells and basophils. A subsequent exposure to the same antigen will trigger these antibodies, causing degranulation of the cell and thereby releasing chemical mediators such as histamine, serotonin, slow-reacting substance of anaphylaxis (SRS-A), and eosinophil chemotactic factor of anaphylaxis (ECF-A). When released from cells into the circulatory system, the chemical mediators produce an anaphylactic response.
- Anaphylactoid reactions differ from anaphylactic reactions in that no prior exposure to the agent is necessary to induce the response. The agent itself, not the IgE antibodies, will bind directly to the surface of the cells, causing direct degranulation and a release of mediators. Anaphylactoid and anaphylactic reactions have identical signs and symptoms and are treated in the same manner.
- Anaphylaxis is a severe, rapid, systemic and life threatening allergic reaction that presents as a medical emergency. It can be precipitated in susceptible individuals by a wide range of substances, however, for the purpose of this document, the substances are cytotoxic drugs and biological therapies. Anaphylaxis requires rapid recognition, treatment and management by health professionals.
- Cancer chemotherapy drugs are foreign substances capable of inducing anaphylaxis and reactions which range from mild cutaneous symptoms to severe respiratory distress and cardiovascular collapse. This adverse/allergic reaction can occur within seconds or minutes of drug administration with features of an anaphylactic reaction. Nurses need to be aware of the signs and symptoms of such reaction because if doctors are not immediately available, nurses are responsible for not only recognising the symptoms of a hypersensitivity reaction, but also for treating it promptly.
All health care professionals should understand the causes of anaphylaxis, know how to diagnose anaphylaxis and be able to administer effective treatment.