Confirming the position of a naso-gastric / oro-gastric tube in neonates
exp date isn't null, but text field is
Objectives
This guideline is applicable to all medical, nursing, midwifery and nursing support staff caring for neonates within the West of Scotland in both hospital and community settings. In addition, this guideline is also applicable to parents who have been trained to administer enteral feeds via a gastric tube. Staff should also be aware of guidelines for hand hygiene. Staff should also familiarise themselves with the Wospghan document entitled “Enteral tube feeding Information pack for healthcare professionals”
Gastric tube position should be checked :-
- Immediately after initial tube insertion
- For babies with feeding tube already in situ –
- Check for evidence of tube displacement before each feed (loose tape, movement of tube marker) - and test for pH level prior to each feed by using the minimum of aspirate (no more than 0.2ml)
- continuous feeds –check for evidence of tube displacement hourly and test aspirate pH prior to syringe changes 4hourly
- Nil orally - test for aspirate pH 6 hourly
- Before medications are given
- Following a bout of coughing, retching or vomiting
- Gather together necessary equipment i.e. pH indicator strip and 10ml syringe.
- Wash and dry hands.
- If parents are present, explain that you are going to check the feeding tube position.
- Remove the stopper from the tube.
- Attach a syringe to the end of the tube.
- Aspirate the gastric contents by gently pulling back on the plunger until a small amount of liquid appears in the syringe (0.2-1.0ml).
- Detach the syringe from the tube remembering to replace the stopper.
- Test the pH of the fluid using pH indicator strip. Allow 10 - 60 seconds for any colour change to take place.
- If the aspirate has a pH5.5 or below, proceed to feed. (Aspirates testing pH 5.5 or below should indicate correct placement in most infants).
Gastric Aspirate pH 6 or above
If the pH reading is 6 or above, do not feed and consider the following:
- Is there any evidence of tube displacement? (loose tape, movement of tube marker) Confirm that tube length is correct (refer to documentation in baby’s care plan).
- Is the infant on medication that would affect the pH?
- Is the infant receiving continuous feeds or had a feed in the last hour? If so, retest after 15-30 minutes.
- Have you obtained large quantities of feed coloured aspirate? (Although it is reassuring to obtain a large volume of milk on aspirate, this is not a definitive test.)
- Has a feed been administered very recently? Milk has a pH of 6 to 7 and will temporarily raise the pH by diluting the acidic stomach contents
- Has the infant consistently had a gastric pH ≥6.0?
If the answer to any of the above questions is “Yes”, discuss with medical staff /senior nursing staff prior to administering the feed.
If not, or in any doubt, seek advice from a member of medical/senior neonatal nursing staff. You may have to reposition or remove the gastric tube and reinsert. However, this should only be done as a last resort.
It is important that actions and their rationale are documented.
No aspirate obtained
If there is any difficulty obtaining an aspirate:-
- Insert 1-2 mls of air via the syringe down the gastric tube in an attempt to push the tube’s port away from the stomach wall. Try again to aspirate the tube and test with pH indicator strip.
- Lie the baby on his/her side and try again.
- Attempt to retract the tube slightly (1-2cms) and try again. If this is an initial insertion, then consider replacing or re-passing the tube. If any resistance is felt and this is an initial tube insertion, STOP and seek advice from medical staff / senior nursing staff.
- If the tube has been in-situ already, seek advice from senior neonatal nursing staff.
Infants who consistently have an aspirate pH 6.0 or above should have their care discussed and agreed with the multidisciplinary team. Decisions made should be clearly documented in the infant’s medical, nursing and dietetic notes and communicated to all involved in the infant’s care.
N.B. None of the existing methods for testing the position of gastric feeding tubes are totally reliable. The most accurate method for confirming correct tube placement is radiography. However X-Ray for the sole purpose of confirming gastric tube position in a neonate is not recommended.
If a feeding tube is required and it is likely that the baby will need a chest x-ray, it should be passed prior to the x-ray being performed as the x-ray will confirm the position of a tube from which you may be unable to obtain an aspirate.
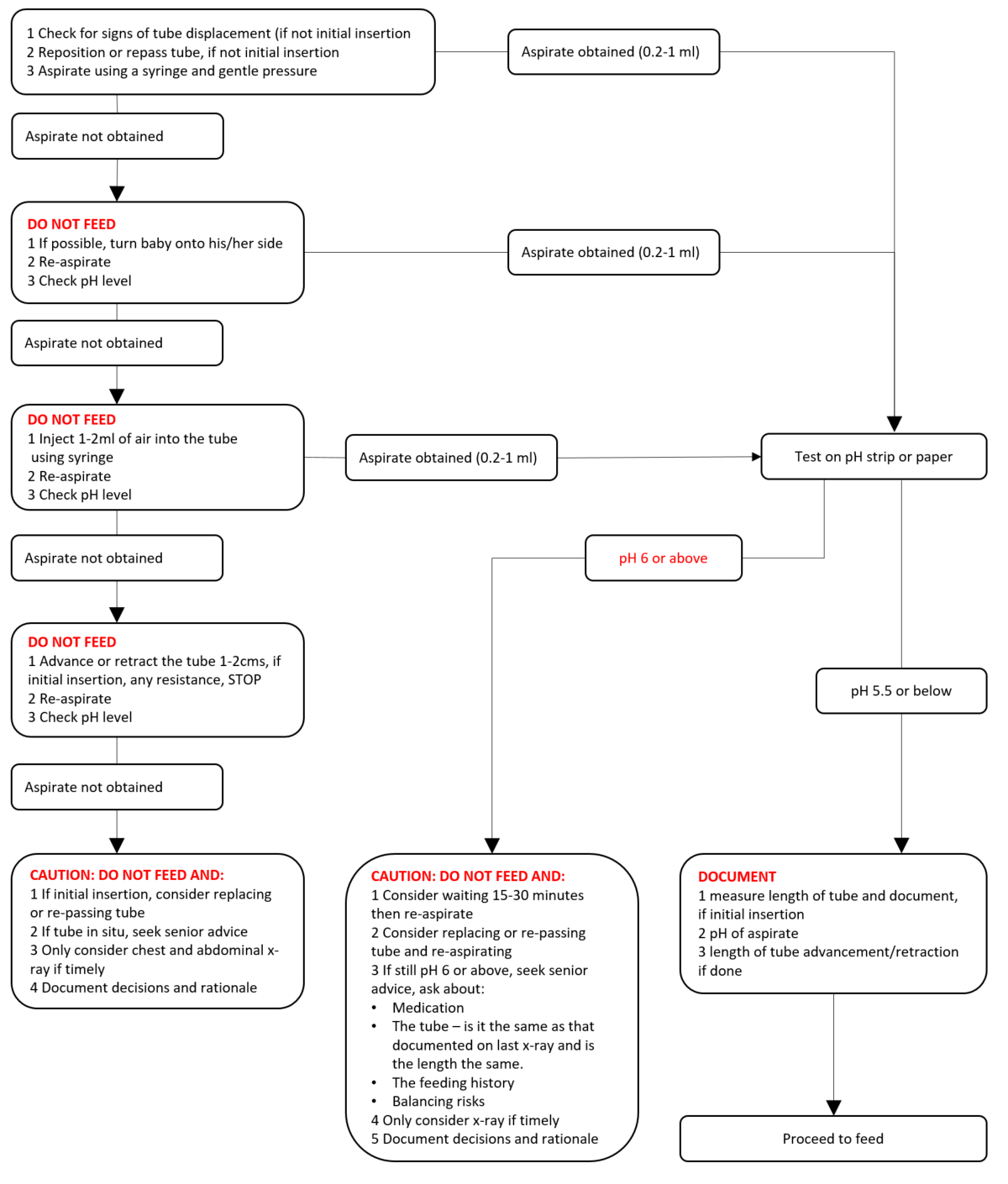
Please see accompanying flow chart on gastric tube position confirmation
 CAUTION: If there is ANY query about position and/or the clarity of the colour change on the pH strip, particularly between ranges 5 to 6. then feeding should not commence.
CAUTION: If there is ANY query about position and/or the clarity of the colour change on the pH strip, particularly between ranges 5 to 6. then feeding should not commence.
Flowchart taken from: National Patient Safety Agency (2005). Reducing the harm caused by misplaced gastric feeding tubes in babies under the care of neonatal units. (Interim advice note: NRLS-0223A).
Huband, S Trigg, E (2002) Practices in children’s nursing : guidelines for hospital and community. Edinburgh : Churchill Livingstone
Metheney, N et al (1993) Effectiveness of pH measurements in predicting feeding tube placement : an update Nursing Research 42(6) 324-331
Metheney, N et al (1998) Testing feeding tube placement: auscultation vs, pH method American Journal of Nursing 98 (5) 37-42
NHS QIS (2003) Nasogastric and Gastrostomy Tube Feeding for children being cared for in the community. Best Practice Statement. Edinburgh NHS QIS
NPSA Patient Safety Alert -“Reducing the harm caused by misplaced naso and orogastric feeding tubes - neonates” September 2005
Spence, K (2003) Nutritional management of the infant in the NICU in Boxwell, G ed. Neonatal Intensive Care Nursing 3rded. Routledge: London Ch.11
Symon, A and Cunningham, S (1994) Naso Gastric Feeding Methods In Neonates Nursing Times 90(35) 56-60
Last reviewed: 14 October 2019
Next review: 01 October 2022
Author(s): Andrena Kelly – Nurse Educator - RHC
Co-Author(s): Other professionals consulted: Anisa Patel, Clinical Pharmacist, NICU, RHC
Approved By: West of Scotland Neonatology Managed Clinical Network

