Croup
exp date isn't null, but text field is
Objectives
This guideline has been designed to assist in the diagnosis and management of children with croup. It includes a management algorithm and a list of potential differential diagnoses.
Scope
Children presenting with the signs of croup.
Audience
Healthcare professionals involved in acute paediatric medicine.
November 2023: This guidance is currently under review as it has gone beyond the standard review date. It reflects best practice at the time of authorship / last review and remains safe for use. If there are any concerns regarding the content then please consult with senior clinical staff to confirm.
Croup is an acute respiratory illness causing inflammation and narrowing of the subglottic region of the larynx. It is most often caused by a viral infection.
Where appropriate (if severity allows) a minimally invasive HANDS OFF APPROACH allows best initial assessment– as children can look very different if allowed to settle for a few minutes
Key points:
- If possible allow child to sit on carers lap – DO NOT FORCE TO LIE DOWN
- Do not examine throat
-
If hypoxic try to give O2 by facemask
The following clinical signs (in varying combination) are found in croup:
- Stridor
- Barking cough
- Hoarseness
- Respiratory distress +/- Fever +/- Coryza
- Respiratory rate
- Heart rate
- O2 saturations
- Respiratory distress
- Exhaustion
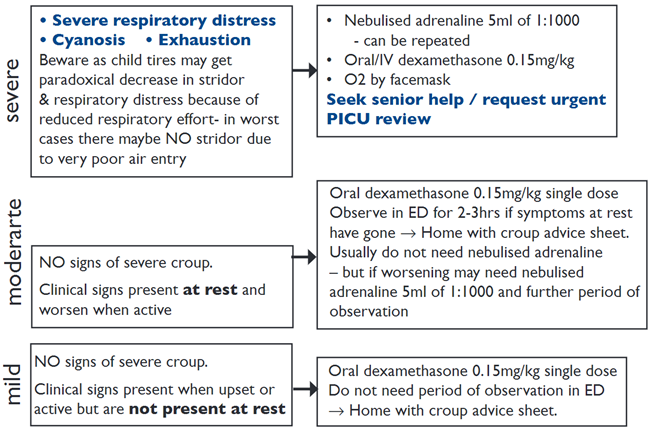
- If prednisolone already given by GP and child has mild croup in ED may not need second dose, but if child has signs of moderate croup consider giving second dose prednisolone 1mg/kg
- If for any reason dexamethasone not available – use prednisolone 1mg/kg once daily for 2 days
- Acute foreign body aspiration
- Acute anaphylaxis
- Bacterial upper airway infections e.g. epiglottitis, bacterial tracheitis.
| Croup | Tracheitis |
Epiglottitis |
|
| Cause | Viral |
Staphyloccocus aureus |
Haemophilus influenzae B |
|
Age |
6m - 3yr | Any age | 2 - 6 yr |
|
Onset |
Gradual | Gradual | Sudden |
|
Pyrexia |
Mild | >38oC | >38oC |
|
Abnormal sounds |
Barking cough, stridor | Barking cough, stridor | Muffled, gutteral cough |
|
Swallowing |
Normal | Difficult | Very difficult with drooling |
|
Posture |
Recumbent | Sitting | Tripod position |
|
Facies |
Normal | Anxious | Anxious, distressed, toxaemic |
Morton, N.S. Large airway obstruction in children: causes, assessment and management. Update Anaesth. 2004;18:1.
Last reviewed: 24 February 2017
Next review: 31 October 2024
Author(s): Steve Foster
Approved By: Clinical Effectiveness
Reviewer Name(s): ED Department

