Juvenile idiopathic arthritis (JIA), management in children
exp date isn't null, but text field is
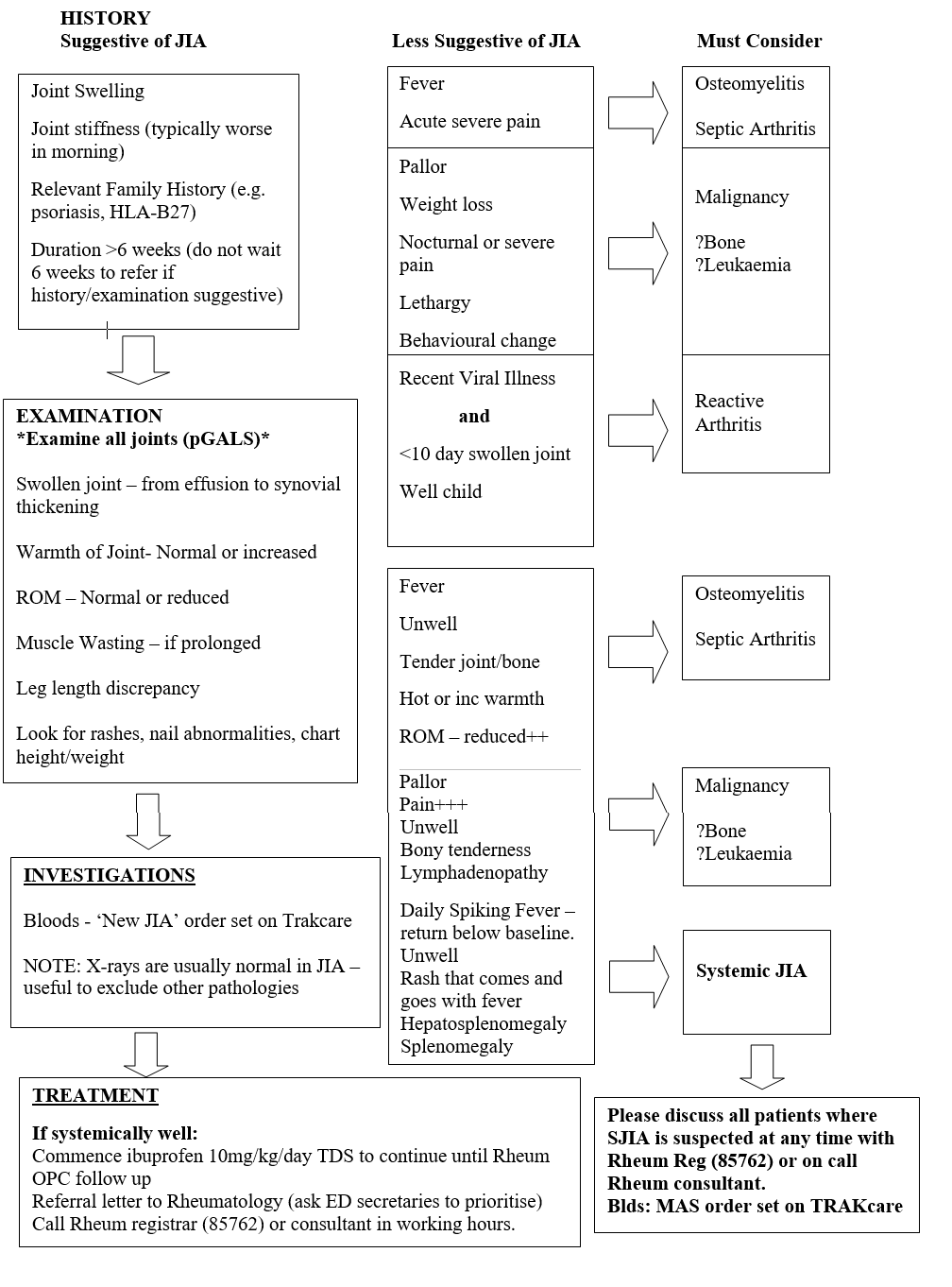
Juvenile Idiopathic Arthritis (JIA) is essentially a diagnosis of exclusion and therefore a high index of suspicion for other differential diagnoses is necessary. The chief differentials for a swollen joint will be infection (septic arthritis or osteomyelitis), malignancy (particularly leukaemia or bone tumours) and trauma.
Note:
- More than one swollen joint will always require rheumatology referral
- In an otherwise well chid with swollen joint(s) the most likely diagnosis is JIA
- Outcome of JIA is better if treated early ∴ have low threshold for referral to Rheumatology
- Beware of labelling all ‘limping’ or non-weight bearing as injury related - some falls are ‘red herrings’. Minor falls are common in children and may be co-incidental.
This is a serious medical condition that can be life-threatening – however it can be difficult to identify early in the course (as arthritis may not be present initially). It may present in many different ways and a high index of suspicion is needed. The disease is present equally in males and females with no preferential age of onset.
SJIA : Diagnosis
Requires presence of arthritis accompanied or preceded by daily-spiking fever plus one or more of the following:
- Evanescent non-fixed macular rash (pink rash that characteristically coincides with fever peaks)
- Hepatomegaly or splenomegaly
- Generalised lymphadenopathy
- Serositis
The arthritis is often symmetrical and polyarticular and can be absent at onset and develop during disease course.
Laboratory findings
Patients in whom a diagnosis of systemic onset JIA is being considered are at risk of Macrophage Activation Syndrome – Please do ‘MAS Set’ bloods on Trak and ensure Ferritin processed as urgent (will be significantly elevated). Please contact on-call Rheumatologist urgently. Lab findings can vary; inflammatory markers often raised, FBC can range from thrombocytosis and leucocytosis to pancytopenias. Please see separate MAS guideline for further information. Please note, normal/low ESR and normal/falling platelets are worrying signs.
Management
Discuss with on-call rheumatologist urgently and arrange admission.
Last reviewed: 01 September 2019
Next review: 31 October 2025
Author(s): Dr Fiona Russell (Consultant in Paediatric Emergency Medicine)
Co-Author(s): Updating authors: Dr Catriona Anderson (GRID trainee in Paediatric Rheumatology) & Dr Neil Martin (Consultant in Paediatric Rheumatology).
Approved By: Clinical Effectiveness
Reviewer Name(s): Paediatric Clinical Effectiveness & Risk Committee