Peripherally inserted central catheters (PICC Lines) - Neonatology guideline
Audience
This guideline is applicable to all neonatal staff caring for babies requiring Peripherally Inserted Central Catheters (PICC Lines). It is imperative that all practitioners inserting these lines should be aware of correct insertion techniques and that all staff involved in the care of these lines are aware of the hazards associated with their insertion and subsequent use.
It is mandatory that any practitioner wishing to learn to insert PICC lines have read this document before attempting to insert a PICC line for the first time.
- PICC lines should largely be reserved for use with TPN or other 24h infusions.
- Bolus drugs and those given by intermittent infusion should be given via a peripheral cannula whenever possible.
- Full aseptic technique should be used for insertion of PICC lines.
- An aseptic non-touch technique should be used for site care and for accessing the system. (Pratt et al)
- An appropriate antiseptic solution should be applied (see antisepsis guideline) and allowed to dry before and after accessing the PICC line. (Pratt)
- The maximum infusion pressures vary for each line. Infusion pressures should not exceed 300mmHg.
- Where possible the larger line (Nutriline) or Premicath with stylet should be used as these are easier to identify on X-ray. Premicaths should be avoided where expected flow rates exceed 10-12 ml/hour.
- Unless urgent access is required when the parents are unavailable, the parents should be informed about the procedure prior to placing a PICC line. They should be informed about the reasons for insertion and given information about the potential hazards (see below), noting that the PICC line is necessary for optimal clinical care. Formal consent is not required.
- Examine the infant to identify a suitable vein (See Fig.1)
- Measure the maximum insertion distance
- Upper limbs/ head & neck: Measure from the likely entry point to the supra-sternal notch
- Lower limbs: Measure from the entry site to the umbilicus
- If perfusion is poor it may be necessary to correct this prior to line insertion.
- It is appropriate to correct any significant coagulopathy before commencing the procedure however there is no requirement to routinely check FBC and coagulation profile if there is no evidence of a bleeding tendency.
- Consider platelet transfusion before the line is placed, particularly if the Platelet count is <50 or there is evidence of excess bleeding from venepuncture sites
- If the infant is known, or strongly suspected to be septic, it may be wise to delay the placement of a PICC line until the sepsis is under control. PICC lines may easily become colonised with micro-organisms which may then prove difficult to eradicate whilst the line remains in situ.
* Where possible veins suitable for PICC lines (e.g. saphenous vein) should not be used for peripheral cannulation and venesection in the first few days to leave them available for this purpose.
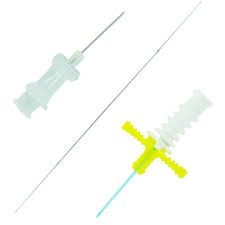
The available neonatal PICC lines are listed below with the manufacturer’s product characteristics quoted.
|
|
Nutriline |
Nutriline Twin-Flo |
Premicath |
Premicath |
|
Ref No. |
1352.152 |
1252.235 |
1261.22 |
1261.208 |
|
Catheter Gauge |
24 G |
24 G |
28 G |
28 G |
|
Catheter Length |
15cm |
30cm |
20cm |
20cm |
|
Introducer Needle Gauge |
20 G Microflash |
20G |
20G |
20G |
|
Catheter Priming Volume |
0.18 ml |
0.2 ml |
0.07 ml |
0.07 ml |
|
Max Flow rate |
240 ml/h |
87 ml/h |
30 ml/h * |
30 ml/h * |
*NB - Premicaths were designed for babies <1kg, who require the smallest catheters.
|
|
Ref No |
Size |
|
Vygon Microflash |
7370.19 |
20 G |
 |
N.B. – Microflash cannulae may be available in some PICC sets but are available separately on the above code should an additional or alternative introducer cannula be required. |
|
|
Vygon Microsite |
1147.02 |
24 G |
|
|
The Vygon Microsite uses a Seldinger technique to insert any of the above PICC lines starting with a 24G needle or 24G IV cannula. Note that the PICC line is not included in this set |
|
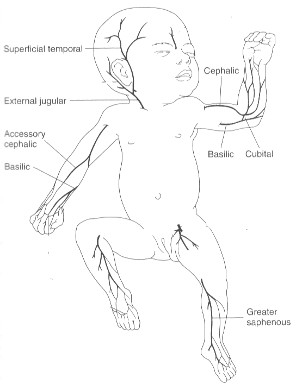 |
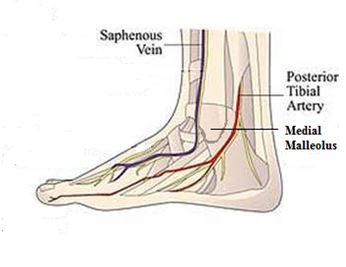
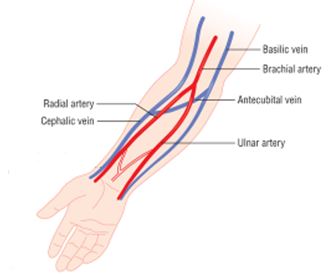
Common sites of PICC line insertion There are multiple potential sites for PICC line insertion. The most commonly used are the antecubital and basilic veins in the upper limbs and the long saphenous veins in the lower limbs. Axillary and scalp veins may also be used. The operator should take time to identify the most suitable point for venous cannulation A number of suitable veins lie in close proximity to arteries risking inadvertent cannulation of an artery. See later section – Specific risks of malposition |
Documentation is essential when placing, manipulating or removing any invasive line.
The operator should record in the notes the following information:
- Details of discussion with parents regarding PICC line insertion
- Name & designation of the operator & anyone assisting/ supervising
- The measured optimum insertion distance
- The no. of lumens, type and size of catheter inserted e.g. Premicath with stylet 28G
- The batch number
- Site of insertion
- Antisepsis used
- The length of catheter inserted (do not exceed the optimum insertion distance)
- If less than this distance document why
- The ability to aspirate blood and flush the line
- The position of the line on X-ray and whether this is satisfactory
- The name of the clinician approving the line for use following the review of the x-ray
- Details of any subsequent manipulation or re-imaging of the line.
PICC line placement should be performed, or directly supervised, by an operator experienced in their insertion- Full aseptic precautions must be observed. A gown and sterile gloves must be worn and a surgical (hernia) towel used
- Use the drapes to cover the infant from head to toe
- The line should be flushed with 0.9% sodium chloride for injection prior to placement and the clamp closed. This will help prevent occlusion whilst awaiting an X-ray. Use a 10ml syringe
- Sterilise the skin around the insertion site according to standard sterile technique. Allow the sterilising solution to dry completely before commencing insertion. Contact with antiseptic solutions may weaken the lines and cause premature failure. If there is any residual antiseptic solution pooling around the limb this should be cleaned off with a saline soaked swab before the procedure.
- Insert the introducer until flashback is noted or free-flowing blood is obtained
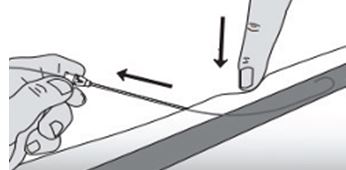
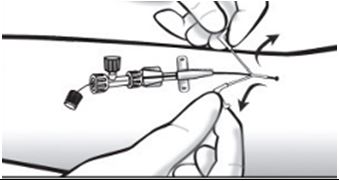
- Insert the long line and use non-toothed forceps to gently advance the line
- Do not insert the line further than the optimum insertion distance measured before the procedure
- If the line will not advance to the measured distance, the tip may have entered the start of an adjoining vessel. Attempts can be made to bypass this by withdrawing the line and then attempting further advancement. Do not leave the tip sitting against such an obstruction.
- Once successfully inserted, remove the introducer and apply gentle pressure to the insertion site until all oozing of blood around the PICC line has stopped
- Secure the line in place with a steristrip close to the entry site then cover the line with a Tegaderm dressing (or similar semi-permeable clear dressing) ensuring that all of the polyurethane part of the catheter is covered. This will involve looping the redundant portion around the entry site
NB Ensure the junction between the polyurethane part of the catheter and the wider bore section is covered by the dressing as this is a site which is prone to snapping if not supported.
Images by Dr Asma Yasmeen – Speciality Doctor Princess Royal Maternity

- The position of the line should be determined before TPN or drugs are infused through it. A 10% glucose infusion may be commenced prior to confirmation of line position if hypoglycaemia is a significant risk
- For upper limb PICC lines the x-ray should be taken with the limb in a neutral position.
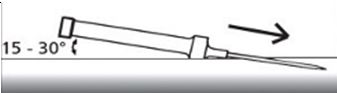 |
Insert the cannula into the chosen vein. A 24ga yellow cannula may be used if preferred |
 |
Insert the guidewire through the needle or cannula. Either end may be used. A mark on the wire indicates when the wire starts to enter the vein |
 |
Withdraw the needle / cannula ensuring that the wire remains in place |
 |
Insert the Microsite cannula over the wire. Use a little rotation of the cannula to ease the tip through the skin. Ensure the outer part of the cannula is well into the vein |
 |
Remove the inner part of the cannula and the guidewire |
 |
Pass the PICC line (Nutriline) through the Microsite catheter to the measured length |
 |
Withdraw the Microsite catheter until the tip is outside the skin and then split the catheter off the PICC line. Secure the PICC line |
The optimal position for the distal tip of a PICC line is in the SVC or IVC but clearly outside the cardiac silhouette.
- For a PICC line inserted in an upper limb or scalp vein the tip should be within the SVC but above T4
- For a PICC line inserted in a lower limb the tip should be within the IVC but below T9 and lie to the right side of the spinal column. (this will require care to ensure the baby is not rotated at the time the X-ray is taken)
It is not always possible to advance a PICC line to the predetermined position and it may be necessary to use a PICC line which lies within a large vein more peripheral than the optimal position however the operator must be aware of the increased risk of malposition under these circumstances. The use of a PICC line where the tip lies outwith the SVC/IVC must be sanctioned by a consultant and, where available, following radiological advice. It may be necessary to do additional imaging +/- the use of contrast media to provide further reassurance about the position of the line.
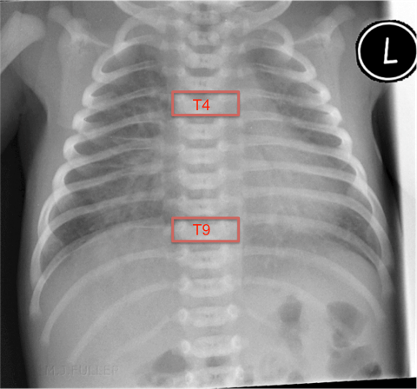
Fig.2 Neonatal CXR with maximal insertion landmarks
The following is a list of ‘red flags’ which raise the possibility of malposition
- The PICC line ‘sticks’ during insertion and cannot be advanced to the length anticipated
- The tip of the PICC line cannot be clearly identified on the x-ray
- The route the PICC line takes is not smooth, with kinks or sharp deviations
- The tip of the PICC line lies at the level of the hip or shoulder joints
- The PICC line inserted in the left leg fails to cross the midline to lie to the right of the spine
- The PICC line does not flush or sample. B. even 27G catheters allow a little blood to be withdrawn into the catheter even if full sampling is not possible.
- Therapeutic infusions fail to have the desired effect g. hypoglycaemia despite glucose infusion
- The tip of a PICC line may be visualised more easily if a larger PICC line (24G) is used. These lines are the preferred choice if a suitable vein is available. Using a 24G PICC line also allows the use of multi-lumen lines and higher flow rates.
If a 27G PICC line is required, visualisation is easier if a styletted PICC line is used and therefore these are the preferred line to be used in ELBW patients with small veins.
The tip of a non-styletted 27G PICC line may not be accurately identified in up to 50% cases (Reece et al). If a line of this type is inserted, the x-ray should be taken using contrast media to aid visualisation.
For any PICC line where the tip is not clearly identified, the x-ray should be retaken using contrast media.
- When using contrast only 0.2ml of Omnipaque (240mg/ml) is required. Prior to using the contrast, flush the line with 0.9% Sodium Chloride for injection to ensure patency. The X-ray should be taken a few seconds after the Omnipaque has been injected. (This should allow contrast in the vein to disperse but ensure that pooled, extravasated contrast, in a non-vascular space, does not have time to disperse). The line should then be flushed with 0.9% sodium chloride for injection again and the gate clamp closed until the X-ray has been reviewed.
There has been a historical reluctance to use iodine containing contrast media in the preterm population due to concerns about potential impact on thyroid function. Recent data from the I2S2 study have provided reassurance around this. - The X-ray should include the anticipated course of the PICC line starting at the hip/shoulder joint on that side. This will assure the operator that the line route does not show any deviations at the important venous junctions. It will also ensure there are no loops that could unwind and cause the tip to migrate.
- The line tip should be visualized in a large central vein outside the cardiac silhouette.
- If the catheter is in an inappropriate position the line must be withdrawn and a further X-ray should be taken to ensure the line is now correctly sited.
- Ultrasonography can be utilised to identify line tip position (Madar/ Jain) though this should only be performed by appropriately trained personnel
- If the line takes an unusual or tortuous route advice must be sought from a senior paediatrician or radiologist before the line is used.
- If the line cannot be advanced to the pre-measured length or the tip lies at the level of the hip or shoulder joints, the tip may be in a small tributary vein. These lines should be withdrawn slightly to ensure the tip is in a main vein.
- The position of the line should be reviewed on any subsequent X-ray to ensure migration has not occurred.
- Record a “sticky note” on PACS including position of the line tip and any amendments to the line position.
“Short” long line
Not infrequently, a PICC line cannot be advanced as far as planned during preparation for the procedure. In many cases these lines are within a large vein but short of the IVC/SVC. In a few cases the tip of the line may be embedded in the wall of the vessel or it may have entered a small tributary vessel. Such tributary vessels are commonest around the large joints such as the hip or shoulder. PICC lines in these locations are prone to thrombosis and extravasation and may cause local injury if this occurs.
It is sometimes necessary to use a PICC line which cannot be advanced into the SVC/IVC, but which sits instead in a large vein short of the preferred location. This is usually the case where no other suitable vessels are identified to place an alternative line. Extra care must be taken to ensure that the tip is within a large vein.
- Ensure there are no other “red flags” from the list above
- Ensure that the line samples blood
- If not sampling or sampling with difficulty, withdraw the line a short distance and try again
- Consider the use of contrast medium
Lines in these positions should be replaced or removed as soon as practicable.

PICC line which has failed to advance beyond the hip joint
Inadvertent insertion into the lumbar vein
This complication is rare and predominantly affects PICC lines inserted into the left leg. Possible warning signs that the line has entered the lumbar vein may include some of the following:
- Failure to advance the line as far as anticipated
- The PICC line does not cross the midline to lie to the right of the spine on x-ray
- The PICC line that has an unexpected kink or deviation to its path on x-ray.
- A lateral X-ray may demonstrate deviation of the line posteriorly
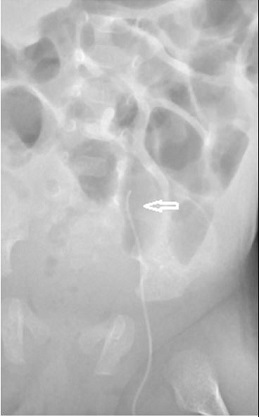
See illustrative x-rays below.
If there are any concerns that this complication has occurred, a lateral x-ray may show the line deviating posteriorly. If possible, seek advice from radiology about further imaging.
Such lines must not be used and the catheter should be removed. These lumbar veins are small, and extravasation of the infusate into the spinal canal may readily occur. This may result in permanent neurological injury and seizures.
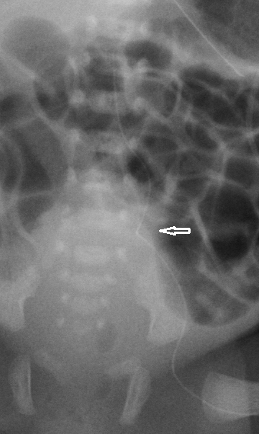 |
These two x-rays show PICC lines that have entered the left lumbar vein. In both cases the line has not crossed the midline and lie to the left of the spine. Both X-rays show a kink in the route (arrow) although it is important to note that these kinks were not apparent on the initial x-rays and this feature cannot be relied upon |
 |
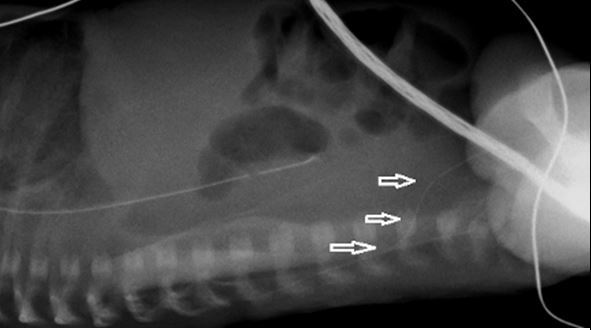 |
This lateral x-ray shows a PICC line in the left lumbar vein taking a posteriorly deviated route (arrows). The correct route would show the line continuing to lie anterior to the spine. | |
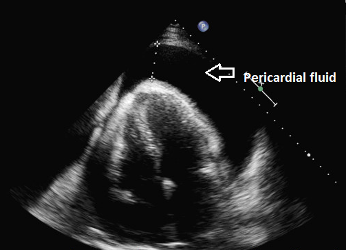
Cardiac tamponade
This complication may occur if the tip of the PICC line lies within the heart. To avoid this complication the tip of all PICC lines must be seen clearly outside of the cardiac silhouette. See advice on imaging above. Cases have been recorded where the tip appears to have migrated after the initial X-ray. To guard against this, the tip of the line should be noted on any subsequent x-ray taken for other reasons. The following symptoms and signs may alert the clinician that tamponade has occurred
- Tachycardia
- Bradycardia
- Hypotension
- Desaturation
- Quiet heart sounds
- Sudden collapse
- Enlarged cardiac shadow on x-ray
Cardiac tamponade can be easily diagnosed using an ultrasound scanner as there will be a large collection of fluid around the heart. See appendix for the procedure for aspiration of a cardiac tamponade.
 |
 |
Inadvertent placement in an artery
There are a number of locations where an artery lies in close proximity to a vein which may be selected for PICC line insertion. All operators must be aware of the local anatomy.
 |
 |
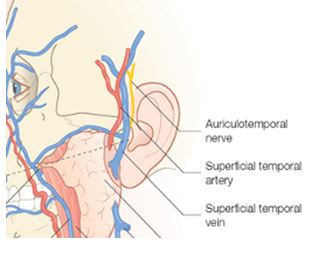 |
|
The ankle |
The elbow |
The scalp |
Possible warning signs suggesting inadvertent cannulation of an artery include some of the following:
- Pulsation of blood in either the introducer or the PICC line
- Arterialised blood from the needle or line (this can be determined from the colour or by testing a sample in the blood gas analyser)
- Blanching of the skin around the insertion site when the needle is flushed during insertion
- Blanching of the limb distal to the site of insertion
If there are suspicions that an artery may have been cannulated, the line must not be used until correct placement has been confirmed. Opinion should be sought from the attending consultant. If the limb becomes ischaemic the line should be removed immediately.
Perforation of the microbore catheter tubing
The polyurethane tubing of a PICC line is very thin and the lines can burst if too much pressure is applied. To avoid this complication the following precautions should be taken:
- Avoid high pressures when flushing a PICC line - use a 10ml syringe
- When flushing do not use excessive force to overcome resistance within the tubing.
- Do not increase pressure limits on infusion pumps or syringe drivers to overcome resistance.
Damage to the PICC line due to gate clamps
The gate clamp on the PICC line's extension tubing may cause a fracture of this tubing if used too close to the catheter hub, if left closed for extended periods or if repeatedly used on the same portion of the tubing.
Removal of a PICC line and the risk of the line snapping
- Care should be used to remove the occlusive dressing, particularly in ELBW babies with fragile skin
- Remove the PICC by applying gentle traction to the line close to the point of entry.
- If the line is being removed because there are concerns about sepsis then it may prove useful to send the line tip to microbiology for culture. If the line is being removed as it is no longer required then this is not necessary
- Gentle pressure on the site may be required to stop bleeding.
- The entry site may be left open to the air
A PICC line may become adherent to the tissues around the insertion site especially if it has been in situ for a prolonged period. If significant resistance is felt when removal is attempted then the operator should cease and seek senior advice as the line could snap leaving a portion within the vein, which may be very difficult to remove.
Breakage of Premicath lines
These catheters are more prone to breakage (snapping or bursting) than wider bore catheters. This is due to a number of factors including their very thin walls. Antiseptic solutions may weaken the catheter material and should not come into direct contact with the catheters. Ensure antiseptic solutions used to clean the skin are allowed to dry thoroughly before starting the catheter insertion. The catheters may be prone to fracture at the junction of the thin polyurethane section and the wider microbore tubing. This junction should be secured under the dressing to support this vulnerable area.
Bacterial / Fungal colonisation and sepsis
If bacteraemia or fungaemia occur whilst a PICC line is in situ the lines may easily become colonised. This can also occur if inadequate aseptic precautions are observed during insertion or when accessing the line when changing infusion fluids.
Such colonisation is very difficult to eradicate whilst the line remains in situ.
Failure to remove PICC lines in the face of bacterial or fungal sepsis is associated with failure of antimicrobial treatment and increased morbidity and mortality particularly with fungal sepsis.
If a PICC line is in situ when a neonate becomes septic then withdrawal of the line would be appropriate in most cases. If the line is vital because of very difficult vascular access, and where it is clear that long term central venous access will be required (e.g. babies with “intestinal failure”) the situation should be discussed with the NICU consultant as it may be more appropriate to initially treat the infection and conserve the line. Where the decision is made to retain the line for such reasons, this should be clearly documented. It is prudent to remove the line at the point of discontinuation of antimicrobial therapy as there may be a significant risk of recurrent infection.
All central lines should be inserted using full aseptic precautions. Each lumen should be capped with a needle-free connector. See separate advice about aseptic precautions to be taken when accessing central lines.
All vascular access devices have associated hazards. Before the insertion of a PICC line, the following information should be discussed with the parents before insertion.
(unless urgent vascular access is required when the parents are unavailable)
Placing PICC lines is a skilled procedure. All Medical staff or ANNPs placing these lines are required to be trained under the supervision of senior colleagues. In addition, they are required to have read this guideline to ensure they are familiar with the technique and the possible hazards.
Why we use PICC lines
Peripheral vascular catheters (PVCs) are useful for short term access to a baby’s veins, for the administration of fluids and medications. PVCs have significant limitations. Small peripheral veins thrombose readily. This requires replacement of the PVC and it may take some time before the affected vein recannalises allowing it to be used again. If vascular access is required on an ongoing basis we frequently run out of peripheral veins to use for PVC access. When the vein thromboses there may be an extravasation of the IV fluids or medications and this may cause a significant extravasation injury. This risk is increased where the osmolality of the fluid is high e.g. TPN, glucose (>10% solution) or if an infused medication is particularly irritant e.g. Bicarbonate, Calcium Chloride, Ganciclovir. Refer to the WoS guideline on extravasation injury for a full list of fluids for which there is an increased risk of such injury.
We recommend the placement of a central vein catheter when we are likely to run out of peripheral veins for PVC placement or where we need to infuse TPN or other irritant fluid. A UVC may be placed after birth but there are national recommendations that we limit the use of these lines to between 7 and 10 days.
Misplacement or Displacement:
The PICC line tip should come to rest in the Superior or Inferior Vena Cava (large veins which bring blood back to the heart from the body).
Lines may insert too far: Although we measure the baby to estimate the correct length for insertion, the line may be found to have reached the heart. If so the line must be withdrawn to the desired location and re x-rayed.
Lines which do not reached the planned position: Occasionally the line does not pass smoothly to reach the desired location and this may occur for a number of reasons.
The commonest reason is that the veins are simply too small and the line may not be able to advance as far as we would like. If the tip reaches a large vein but does not pass as far as the vena cava, the line may still be able to be used but it will not last as long as a line placed in the vena cava.
Less commonly the tip of the line may have become lodged in the wall of the vein or entered a smaller blood vessel which connects to the larger veins. If this is recognised then the line may be partially withdrawn and re x-rayed. If the line is not pulled back the vein may eventually rupture, allowing the parenteral nutrition fluid or medications to leak into the surrounding tissues. If this is not recognised the leaking fluid may cause injury to the surrounding tissues which may have serious consequences depending on exactly where the fluid leaks.
Medical staff are aware of instances where such a misplacement has not been recognised and our guideline now includes more detail of the warning signs that misplacement has occurred.
Lines which move after insertion: PICC line tips have been demonstrated to ‘migrate’ after insertion, i.e. the tip of the line is seen to have moved further into the baby on a later x-ray. All medical staff are reminded to check the line position on each x-ray taken whilst the line is in position. (We do not take regular x-rays specifically to look at the line as we must also limit the amount of radiation to which the babies are exposed.)
Damage to lines
Perforation: This may occur when fluid passes through the line under too high a pressure. We limit the pressure on the pumps and we advise medical staff flushing lines not to use small syringes as these exert the greatest pressure. Although perforation of the line does not usually cause injury directly, it does mean that the line will need to be replaced
Infection of the lines:
Any device which passes through the skin may become colonised with bacteria or fungi if it remains in position for long enough. Medical and nursing staff are all trained in hand hygiene and aseptic technique both during insertion and during later care of the line.
If the line does become colonised and the baby develops an infection it is usual practice to consider removing the line as this will speed the recovery from infection.
In some cases the line may be the only access we have to the baby’s veins and under these circumstances the medical staff may decide to leave the line in place and treat the infection through the line. The line can be removed when other vascular access is possible, or at the end of treatment.
N.B. NICE have recently recommended that there is no evidence to support the use of antimicrobial impregnated central catheters and that these catheters are not recommended (Neonatal infection: antibiotics for prevention and treatment NG195 April 2021)
Cardiac tamponade is a rare complication of PICC line use in neonatal units. It is a medical emergency, with associated morbidity and mortality. Literature suggests an incidence of 0.76% to 3% in infants with PICC lines. Retrospective data from the UK estimate an incidence of 0.2%, with a mortality of 0.7 per 1000 neonates. Initial resuscitation should be methodical and follow recognised life support guidelines. Siting catheter tips outwith the cardiac border does not completely abolish the risk of pericardial effusion, or cardiac tamponade.12
Pericardiocentesis should only be performed by skilled operators, under ultrasound guidance, unless a delay in treatment would be life threatening. If it is not possible to await ultrasound-guided drainage, emergency pericardiocentesis should be attempted by the most experienced neonatal practitioner available.
In subacute cases, where infusate pericardial effusion is suspected, there may be a role for aspirating the PICC line in-situ. This should be discussed with the Consultant on-call.
Clinical Signs:
- Tachycardia
- Bradycardia
- Hypotension
- Desaturation
- Quiet heart sounds
- Sudden collapse
Investigations:
- Chest X-ray: Widened mediastinum +/- fluid level
- ECHO (if available/ time permits)
Equipment:
- Sterile gloves & gown
- Sterile drapes
- Dressing pack
- 22/24G Cannula
- 10ml syringe x 2
- 3-way tap
- Suitable cleaning Solution - See antisepsis guidelines
Procedure:
- Ensure senior support available or en route to attend
- Clean the skin around the xyphisternum and allow to dry
- Connect the cannula to one syringe

Fig. 4 IV Cannula & 10ml syringe
- Connect the 3-way tap and other syringe
- Insert the cannula below the xiphisternum at 30° to the skin, aiming towards the left shoulder
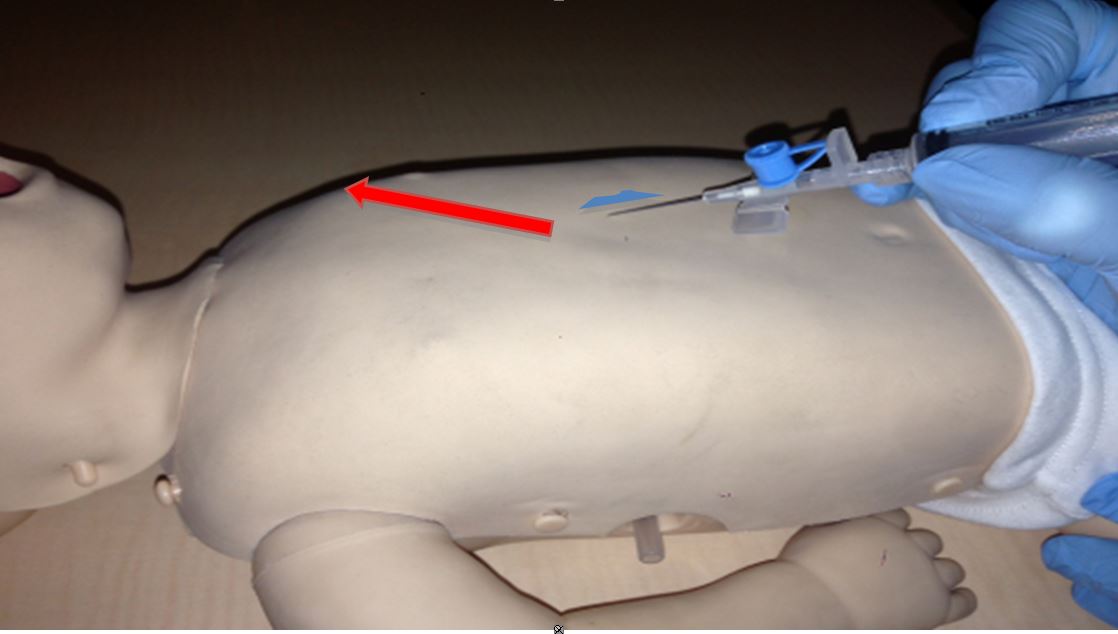
Fig.5 Approach for emergency pericardiocentesis
- Aspirate continuously as the needle is advanced until blood or infusate is aspirated
- Advance the plastic sheath of the cannula, ensure the needle does not advance further
- Connect the 3-way tap & use to aspirate the pericardial contents
- Send the aspirated fluid for microbiological and biochemical investigation
- Cover the injection site with an occlusive dressing e.g. Tegaderm
Pratt RJ, Pellowe C, Loveday HP et al. The epic Project: Developing National Evidence-based Guidelines for Preventing Healthcare associated Infections. Phase 1: Guidelines for Preventing Hospital-acquired Infections. Journal of Hospital Infection 2001;47(Supplement):S43-S44
Cartwright DW. Placement of neonatal central venous catheter tips: is the right atrium so dangerous? Arch Dis Child Fetal Neonatal Ed 2002;87:F155-F156
Department of Health. Review of four neonatal deaths due to cardiac tamponade associated with the presence of a central venous catheter. London: HMSO, 2001.
MHRA Device Alert - DA2001(04). The Use of Central Intravenous Access in Neonatal Parenteral Feeding
Nowlen TT, Rosenthal GL, Johnson GL et al. Pericardial Effusion and Tamponade in Infants With Central Catheters. Pediatrics 2002; 110:137–142.
Beardsall K, White DK, Pinto EM et al. Pericardial effusion and cardiac tamponade as complications of neonatal long lines: are they really a problem? Arch Dis Child Fetal Neonatal Ed 2003;88:F292–F295.
A Reece, T Ubhi, A R Craig and S J Newell. Positioning long lines: contrast versus plain radiography. Arch. Dis. Child. Fetal Neonatal Ed. 2001;84; F129-130.
Keeney SE, Richardson CJ. Extravascular extravasation of fluid as a complication of central venous lines in the neonate. J Perinatol 1995;15:284–8.
Racadio, J. M., Doellman, D. A., Johnson, N. D., Bean, J. A., & Jacobs, B. R. (2001). Pediatric peripherally inserted central catheters: Complication rates related to catheter tip location. Pediatrics, 107, E28.
Serrao, P. R., Jean-Louis, J., Godoy, J., & Prado, A. (1996). Inferi- or vena cava catheterization in the neonate by the percutaneous femoral vein method. Journal of Perinatology, 16 (2 Pt. 1), 129–132.
Jain A, McNamara PJ, Ng E, El-Khuffash A. The use of targeted neonatal echocardiography to confirm placement of peripherally inserted central catheters in neonates. Am J Perinatol. 2012 Feb;29(2):101-6. doi: 10.1055/s-0031-1295649.
Last reviewed: 07 July 2021
Next review: 01 July 2024
Author(s): Dr A Powls – Consultant Neonatologist PRM
Co-Author(s): Other Professionals consulted: Dr Allan Jackson – Consultant Neonatologist PRM; Dr Joyce O’Shea – Consultant neonatologist RHC; Dr Ruth Allen – Consultant Radiologist RHC; Dr Jon Staines – Consultant Paediatrician Ayrshire
Approved By: West of Scotland Neonatology Managed Clinical Network