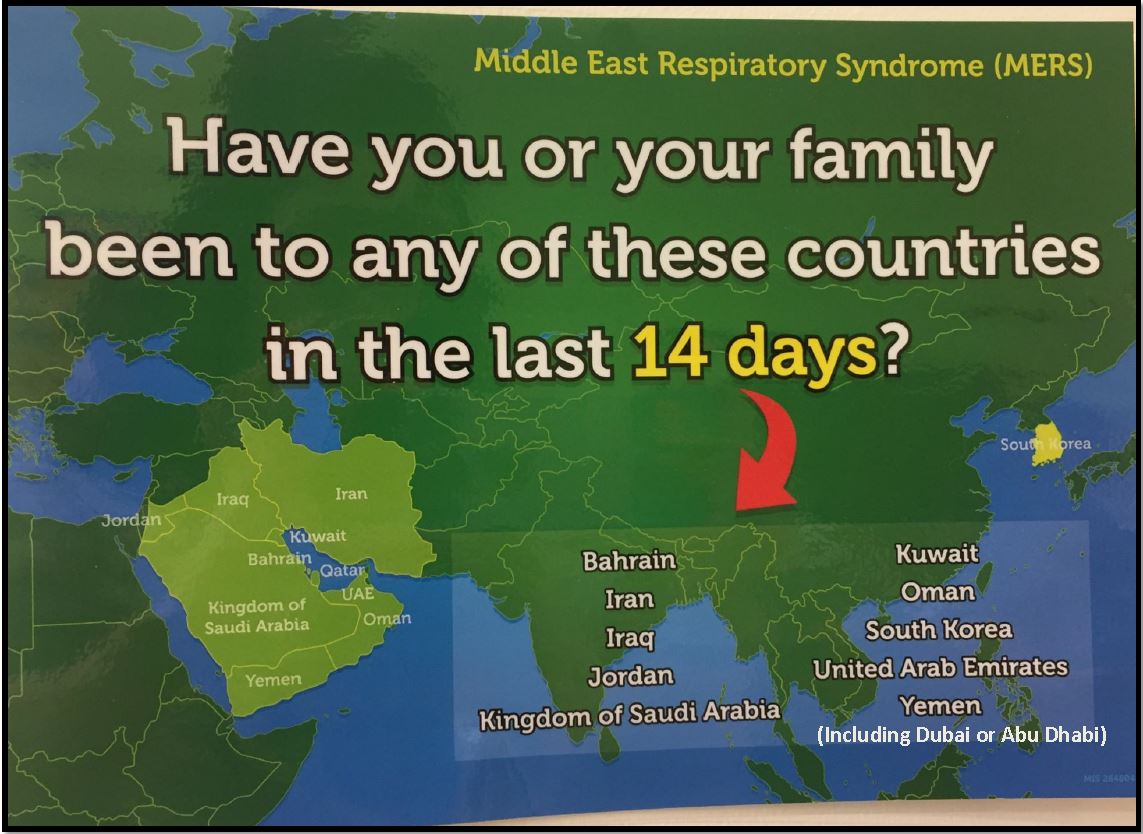
- Reception staff to ask patients if they have been to one of the “MERS POTENTIAL” countries in the last 14 days (see map below).
- MERS potential countries include:
- Bahrain
- Jordan
- Iraq
- Iran
- Kingdom of Saudi Arabia
- Kuwait
- Oman
- Qatar
- United Arab Emirates ((including Abu Dhabi & Dubai)
- Yemen
- South Korea
- If there is a positive travel history to any of the above countries in that time frame, reception staff to ask patient to wait in the breast feeding consultation room across from the reception desk for immediate assessment by the triage nurse.
- Positive travel history –THE PATIENT MUST have been in a “MERS potential” country in the last 14 days before symptom onset and have respiratory symptoms. (NOT patient relative and NOT just transiting through the airport)
- Reception staff to inform triage nurse and ED nurse coordinator immediately.
- Reception staff to take screen shot identifying list of patients in the ED waiting room and in triage queue.
- Breast feeding room to have a terminal clean after it is vacated.