- Duration
- Speed of change
- Associated fever
- Pain
- Recent illnesses
- Risk factor exposure (TB, cats, HIV)
- Previous episodes
Neck lumps - RHCG Emergency Department

Objectives
This guideline is for RHCG Emergency department staff to support assessment, investigation and management of patients presenting with neck lumps.
Scope
Children with neck lumps.
Audience
Clinicians working in the Emergency Department.
Neck lumps are a common presenting complaint to the paediatric emergency department with a wide range of aetiologies. These can be broadly separated into congenital, inflammatory and neoplastic masses. Thorough history taking and detailed examination can aid in diagnosis and management. Inflammatory masses are by far most common, accounting for 75% of neck lumps and 80-90% are benign in origin.
Lump exam
- Size
- Consistency
- Texture
- Location
- Single versus multiple
- Uni- versus bi-lateral
- Tenderness
- Skin changes overlying the mass (description of nature of changes essential – including mobility to skin and surrounding tissue)
Systemic exam
- Hepatomegaly
- Splenomegaly
- Other lymphadenopathy (groin/armpit)
- Rash
- Well vs unwell child
- Stridor
- Dysphagia
- Drooling
- Torticollis
Reactive lymphadenopathy is very common secondary to upper respiratory tract infection. Identifying the focus of infection will guide management. Most commonly, this will be a viral infection and require symptomatic management only. Reassure parents and discuss the natural history of waxing and waning of lymphadenopathy as well as when to seek medical advice as below in addition to red flags:
- Persistent lymph node >6weeks AND >2cm
- Rapidly increasing size – as documented by healthcare provider (GP or previous ED attendance)
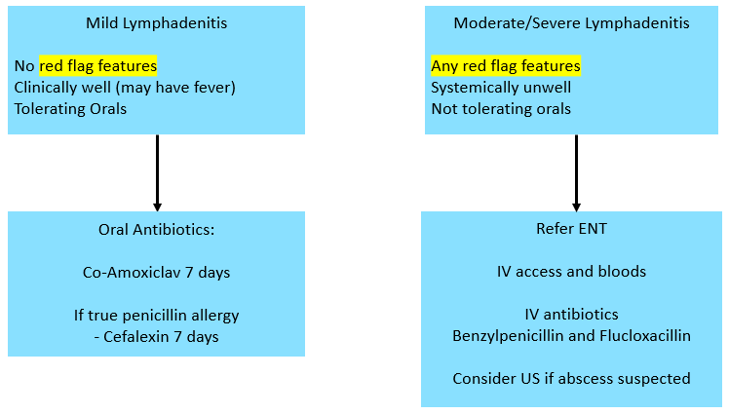
When lymphadenitis is diagnosed, treatment with antibiotics should be considered. When the child is clinically well, will tolerate orals and without any red flag features, treatment can be with oral antibiotics. Treatment of choice is 7-days of Co-Amoxiclav and Cefalexin in Penicillin allergic patients.
After successful treatment it is possible that the residual node might remain noticeable for 2-3 months.
In children with red flag features, features suggestive of an abscess or not tolerating oral intake, referral should be made to ENT to review in the emergency department for consideration of imaging, IV antibiotics and admission.
Congenital non-inflammatory masses generally do not require admission to hospital unless there are airway concerns. Sternocleidomastoid tumours should be referred to physiotherapy for treatment.
If a suspected congenital neck mass is identified in ED then patient should be discussed with ED senior decision maker and if ongoing concerns, then the case should be discussed with the on-call ENT team.
In children where there is a concern of a neoplastic neck lump, additional urgent investigations will be required including bloods, ultrasound and CXR if lymphoma is suspected to assess for evidence of mediastinal widening. Immediate referral to Oncology is appropriate if malignancy is highly suspected or confirmed and these children will be admitted.
Red flags
- Septic or unwell-looking child
- Difficulty swallowing
- Stridor or airway compromise
- Change in voice
- Rapidly progressing (significant increase in less than 4 days)
- Tethered node
- Red flag features
- Unable to tolerate oral antibiotics
- Suspicion of abscess
- Suspicion of malignancy
- Suspicion of congenital neck lump
- Supraclavicular nodes
Ultrasound is the imaging of choice for neck lumps. For those who require inpatient ENT assessment, ultrasound can be carried out the ascertain presence of abscess or suspicion of malignant changes in the lump. All imaging decisions should be made in combination with ENT and radiology teams.
Patients discharge from ED on oral antibiotics should be advised of specific red flag features warranting repeat ED attendance.
They should also be advised to attend their primary care team after the completion of the antibiotic course to ensure no abscess is forming. If concerns arise that an abscess is forming or the patient develops any red flag features then they should be directed to ED for review.
Further indications for referral to ENT for cervical lymphadenopathy from primary care can be found here - Primary Care referral guidelines: cervical lymphadenopathy - advice for referrers.