This section gives guidance on the management of jaundice noted in the first two weeks of life. Separate guidance on management of infants over 2 weeks old is contained in the prolonged jaundice section further into this document.
Testing guidance
Hospital
Key points:
- Healthcare professionals should use every opportunity to assess infants for the development of visible jaundice.
- Higher risk babies should receive an additional inspection.
- If jaundice is visible then a bilirubin level must be measured using a transcutaneous bilirubinometer or serum testing.
- A serum bilirubin must be obtained in babies less than 35 weeks gestation or less than 24 hours old with visible jaundice
- Visual estimation of the severity of jaundice is no longer acceptable.
Detailed guidance
In all babies:
- examine the baby for jaundice at every opportunity especially in the first 72 hours. When looking for jaundice (visual inspection):
- check the naked baby in bright and preferably natural light
- examination of the sclerae, gums and blanched skin is useful across all skin tones.
- The presence or absence of jaundice should be recorded in the notes whenever a baby is examined by a healthcare professional.
High risk infants:
At delivery the midwife looking after the mother should check whether there are factors associated with an increased likelihood of developing significant hyperbilirubinaemia soon after birth:
High risk criteria:
- Gestational age under 38 weeks.
- A previous sibling with neonatal jaundice requiring phototherapy
- This should be recorded clearly on Maternity Badger whenever this
information comes to light during pregnancy.
- This should be recorded clearly on Maternity Badger whenever this
- Mother’s intention to breastfeed exclusively.
Arrangements should be made for identification of infants in these categories, and particular attention made to assessing for jaundice. If visible jaundice is noted by any member of staff prior to this additional check taking place then immediate action should be taken rather than awaiting this additional check.
Urgent additional care for babies with visible jaundice in the first 24 hours:
Measure and record the serum bilirubin level urgently (within 2 hours of detection) in all babies with suspected or obvious jaundice in the first 24 hours of life.
Continue to measure the serum bilirubin level every 6 hours for all babies with suspected or obvious jaundice in the first 24 hours of life until the level is below the treatment threshold and stable and/ falling (this decision should be made by a middle grade or consultant).
How to measure the bilirubin level
A bilirubin level should be measure in all jaundiced babies. When measuring the bilirubin level:
- use a transcutaneous bilirubinometer in babies with a gestational age of 35 weeks or more and postnatal age of more than 24 hours.
- if a transcutaneous bilirubinometer is not available, measure the serum bilirubin
- if a transcutaneous bilirubinometer measurement indicates a bilirubin level greater than 250 micromol/litre a serum bilirubin should be obtained.
- if the transcutaneous bilirubin is within 25micromols/l of the treatment line a serum bilirubin should be obtained (use treatment threshold graph).
- always use serum bilirubin measurement to determine the bilirubin level in babies with jaundice in the first 24 hours of life.
- always use serum bilirubin measurement to determine the bilirubin level in babies less than 35 weeks gestational age.
- always use serum bilirubin measurement for babies at or above the relevant treatment threshold for their postnatal age, and for all subsequent measurements.
Additional tests
In addition to a full clinical examination by a suitably trained healthcare professional, carry out all of the following tests in babies with significant (i.e. requiring treatment) hyperbilirubinaemia as part of an assessment for underlying disease (see threshold chart in appendix 1)
- serum bilirubin (for baseline level to assess response to treatment)
- Full blood count
- blood group (mother and baby)
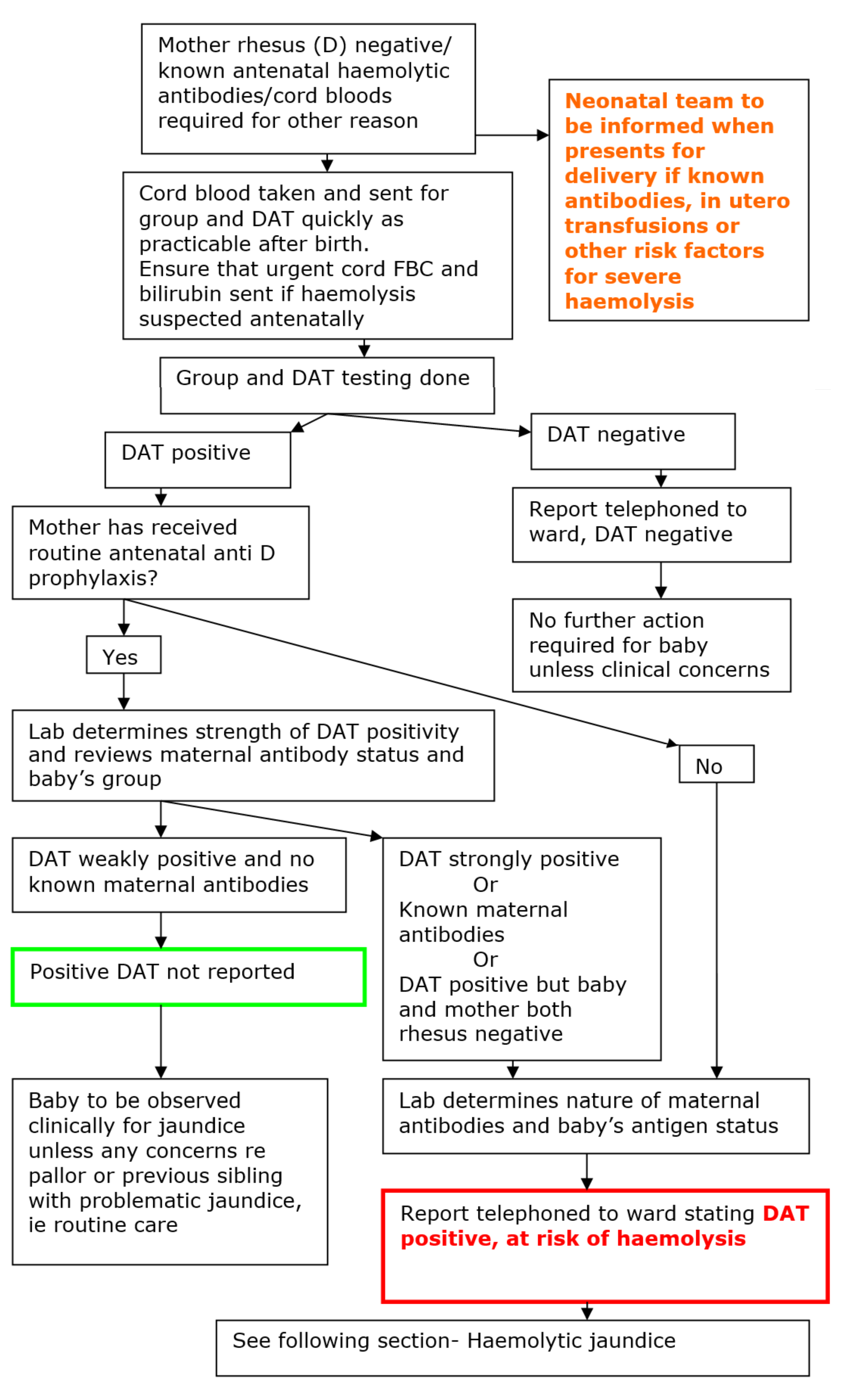
- DAT (Coombs’ test). Interpret the result taking account of the strength of reaction, and whether mother received prophylactic anti-D immunoglobulin during pregnancy.
When assessing the baby for underlying disease consider whether the following tests are clinically indicated:
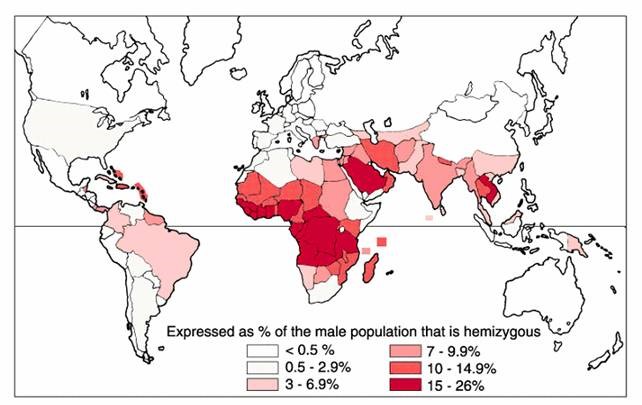
- blood glucose-6-phosphate dehydrogenase levels, taking account of ethnic origin
- microbiological cultures of blood, urine and/or cerebrospinal fluid (if infection is suspected).
Timing of repeat samples where the initial measurement is below the treatment threshold:
In 2016 NICE revised their guidance around the timing of repeat samples for infants of 38 weeks gestation or more to the following:
- Within 50micromols/l of the treatment line:
- No additional risk factors- recheck within 24 hours
- Additional risk factors- recheck within 18 hours
Testing frequency guidance is not given for more immature infants. Given their greater susceptibility to kernicterus it would be prudent to ensure that they are retested within 18 hours, less where there are additional risk factors.
Where the bilirubin level is more than 50 micromols/l below the treatment line routine retesting is not required, unless the rate of rise based on serial measurements is a concern, or the clinical situation changes.
Community testing guidance
Timely and accurate measurement of bilirubin levels in the community is a particular practical challenge. With early discharge now the norm it must be recognised that a significant proportion of the assessment of jaundice occurs outwith the hospital setting and away from easy access to measurement resources.
At present the following is recommended:
- Every opportunity should be used while infants are in hospital to accurately measure bilirubin if jaundice is visible.
- Where a bilirubin has been measured the result and subsequent plans for follow up should be made clear to the community midwifery team
- The inaccuracy of visual estimation of bilirubin levels should be borne in mind at all times and if in any doubt a level should be measured, either using transcutaneous bilirubinometry or blood testing.
- It is preferable that measurement takes place in the community rather than by referral to hospital (unless there are other concerns about the infant).
Community teams should seek to improve access to transcutaneous bilirubinometers and/or ensure that staff are able to take, and have processed, blood samples for serum bilirubin.
Remote and rural areas should develop robust guidance with their referral neonatal units to facilitate this process.