Where a previous sibling is affected by one of these disorders, or the parental carrier status is known to put this infant at increased risk the baby may need to be managed differently. This varies according to the condition, as described below:
Phenylketonuria
Risk - Siblings of a child known to have PKU will have a 1 in 4 risk, reducing to approximately 1 in 200 if one parent is a carrier and 1 in 100 if one parent is affected. It will be 1 in 2 where there is an affected parent and a carrier parent. The risk is 100% if both parents are affected.
Early testing (ie at 48 hours) may allow the parents of an affected sibling to know if their new child is affected or not a few days before the normal screening result becomes available. It may not however be as reliable as the day 5-8 test, and as there is no risk of neonatal disease, early testing should reserved for cases where there is significant parental anxiety expressed, and following counselling regarding the risk of a false negative result. For those families at lower risk or where there are mild (non-classical) elevations of then early testing is not recommended.
Screening process
At 48 hours (optional)
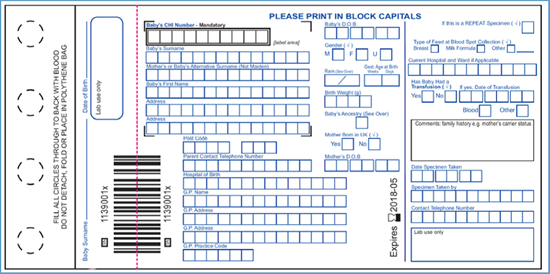
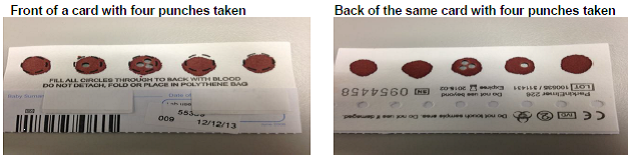
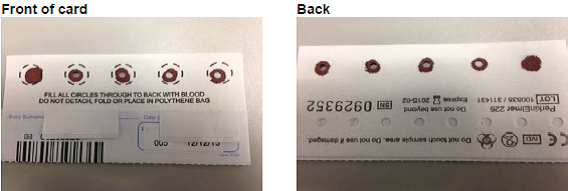
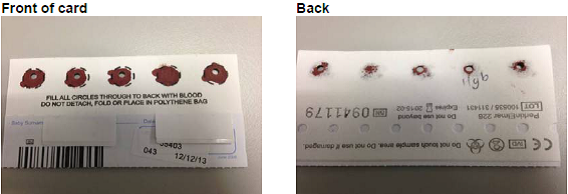
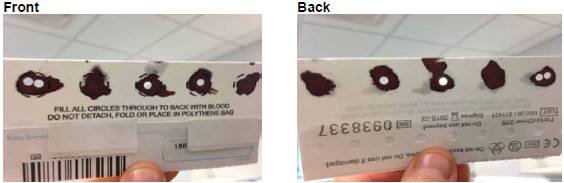
Send 2 drops of blood on a newborn screening card for phenylalanine and tyrosine measurement to:
Department of Biochemistry, Queen Elizabeth University Hospital, 1345 Govan Rd, Govan, Glasgow G51 4TF
Write on newborn blood spot card ‘Family history of PKU'
Day 5 – 8:
Routine newborn screen (5 drops on a newborn screening card), write on newborn blood spot card ‘Family history of PKU’.
Management
The baby should be breast fed or formula fed as normal. He is not at risk of becoming ill in the neonatal period
For further advice the attending metabolic consultant should be contacted via Yorkhill Switchboard during daytime hours.
Other inherited disorders of amino acid metabolism
For siblings of a child with one of the other inherited disorders of amino acid metabolism the risk is similarly 1 in 4. The case should be discussed antenatally with the metabolic team on an individual basis, and a plan of management clearly documented in the maternal notes.
Congenital Hypothyroidism
This is rarely an inherited disorder so no specific measures need be taken unless specified antenatally. This should be specified on the paediatric section of the yellow alert sheet of the maternal notes.
Cystic Fibrosis
Where both parents are carriers of Cystic Fibrosis this should be discussed antenatally and a plan made. The plan should be clearly documented in the paediatric section of the yellow alert sheet in the maternal notes.
In most circumstances cord blood is taken at birth and genetic testing for the parental CFTR mutations performed. For this to be successful, knowledge of the parental mutations is required, which should be dealt with antenatally if early neonatal testing is planned. If in doubt cord bloods can be taken, sent to the DNA lab in clinical genetics and stored pending discussion with the family and the attending consultant geneticist.
Medium Chain Acyl-CoA Dehydrogenase Deficiency (MCADD)
Where there is a previously affected child/and or parental carrier status suggests an increased risk to an infant, guidance has been issued by the NPSA on neonatal management pending results of testing (http://www.nrls.npsa.nhs.uk/resources/type/alerts/?entryid45=132858). This advises that the specialist paediatric inherited metabolic disorder services be contacted antenatally and a post birth plan made. As with other disorders it is vital that this is highlighted in the paediatric section of the yellow alert sheet in the maternal notes.
The following generic advice has been taken from the newborn screening handbook and updated by the Inherited Metabolic diseases team.
Testing
Additional testing should be offered to siblings of a child known to have MCADD (1 in 4 risk) - or where there is an extended family history which causes concern. The risk to the infant is approximately 1 in 200 if one parent is a carrier and 1 in 100 if one parent is affected. It will be 1 in 2 where there is an affected parent and a carrier parent. The risk is 100% if both parents are affected)
When to test and samples taken
24-48 hours:
- Diagnostic acylcarnitine profile (2 drops of blood on a newborn screening card), Write on newborn blood spot card ‘Family history of MCADD’
- Qualitative urinary organic acids (3 to 5 ml urine needed)
- MCADD mutation analysis (0.5 to 1.0 ml blood in an EDTA bottle).
These should be sent to the local biochemistry lab (after telephoning), along with the request form in appendix 4.
Day 5 – 8:
Routine newborn screen (5 drops on a newborn screening card)
Write on newborn blood spot card ‘Family history of MCADD’
Management
Prior to results
This baby is at risk of illness or death in the neonatal period. The aim of treatment is to prevent mobilisation of fatty acids by providing ample glucose - enterally or intravenously. It is essential to ensure that the baby maintains a good milk intake. A term baby should be fed every 4 hours and a preterm baby at least every 3 hours. Exclusively breast fed babies are particularly at risk in the first 72 hours when the supply of breast milk is poor; top up feeds of expressed breast or formula milk may be necessary in the first 48-72 hours until a good milk supply is established. If oral feeds are not tolerated, or if the baby is unwell in any way, urgent referral should be made to a paediatrician for review and consideration of nasogastric tube feeds or commencing intravenous glucose. It is not safe to base the management on monitoring of blood glucose as a baby may be seriously ill even if the blood glucose is normal. A baby should not be discharged until it is certain that he or she is feeding well.
Sickle Cell Disease (SCD)
Where both parents are Sickle Cell disease carriers, there is a 25% risk of the child being affected. This is of no clinical consequence in the neonatal period and so there is no clinical need for testing before the routine day 5 test. The latter should be carried out as normal, with a note on the test card regarding the family status to aid the screening laboratory.
In circumstances where there are particularly high levels of parental concern, consideration can be given to taking a blood spot for screening earlier (this must not be cord blood), but this is not encouraged. Testing should done only be after discussion with a consultant neonatologist, and it must be made clear that the routine day 5 test is still required to screen for other disorders. The card should be clearly marked as an early sample, and sent to the newborn blood spot screening lab, with the laboratory called in advance to discuss. Samples should not be sent to local haematology laboratories for analysis. A clear plan for feedback of results to the family must be made.
Positive results obtained through the routine (day 5) screening process will be dealt with by the screening laboratory with a direct referral to the haematology services in RHSC Yorkhill, or to genetic counselling services where carrier status is identified.