1. Diagnosis relies on samples taken from the system(s) involved (see table).
2. Most tests use PCR technology, these take an average 3-5 hours to complete from arrival in the lab. Most of the tests are multiplexed. This means that a sample may be tested for more viruses than you requested
|
Respiratory Screen by PCR (2 parts)
RS1 – influenza A/B, RSV
RS2 - parainfluenza 1-4, coronaviruses, rhinovirus, human metapneumovirus, adenovirus, mycoplasma
In addition, CMV is tested on the respiratory secretions of all babies <21 days of age & Chlamydia is tested on all negative samples in babies (<2month age).
(NB- if Pertussis PCR testing is required this must be requested separately)
|
| Blood – CMV, EBV, adenovirus, HSV |
| CSF – HSV1/2, VZV, enterovirus. |
| Skin swab – HSV/VZV. |
| Stool samples – norovirus, rotavirus, sapovirus, astrovirus, adenovirus |
| Eyes – HSV, VZV, Adenovirus, Chlamydia trachomatis |
3. In situations which have infection control implications (e.g. outbreak or VZ contact), please contact the lab and infection control to coordinate testing.



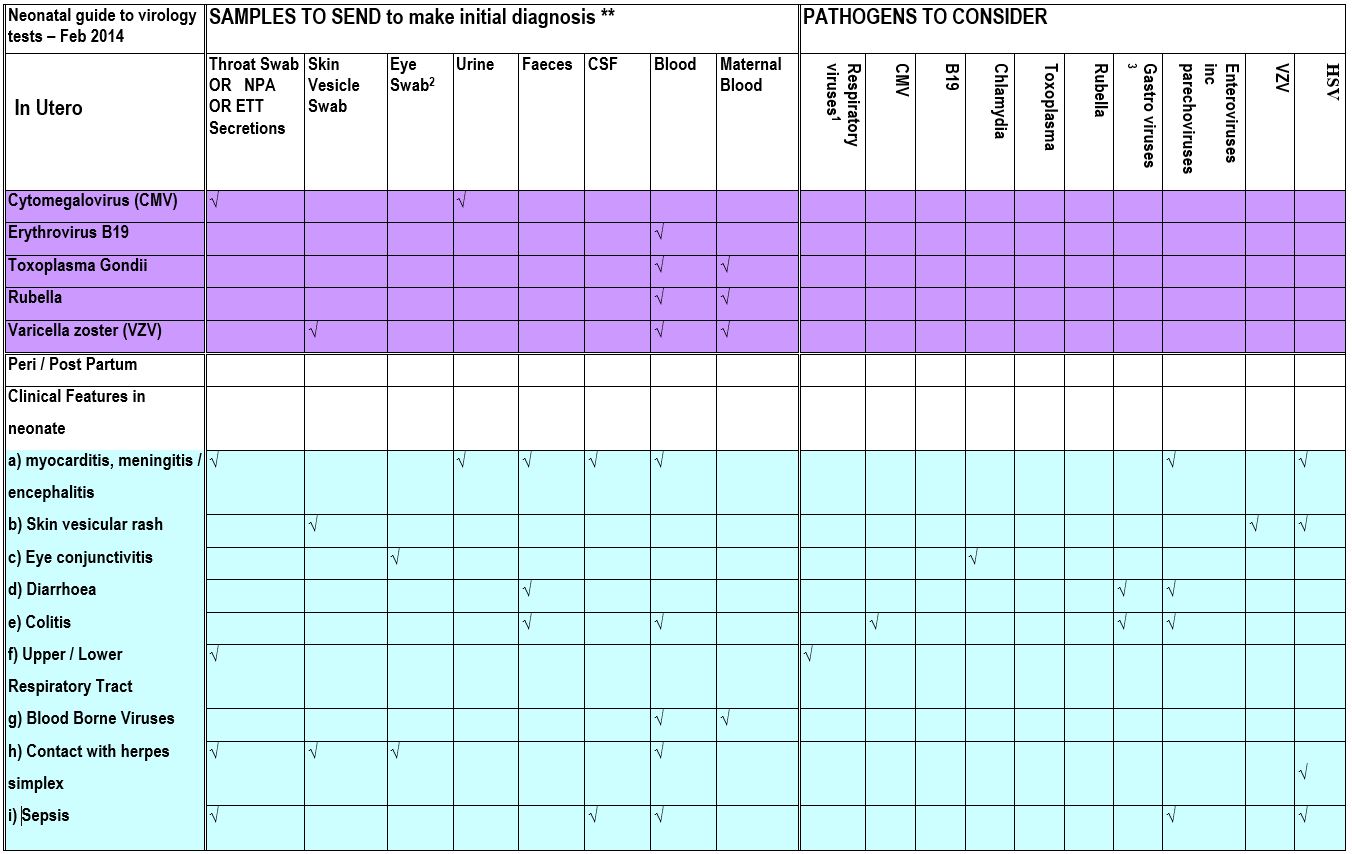 ** Samples are from the neonate unless otherwise specified
** Samples are from the neonate unless otherwise specified