Hyperglycemia is very common in preterm infants. The prevalence is 40-80% in Very low birth weight (VLBW) infants (1). This guideline provides a consensus recommendation on management of hyperglycemia in preterm infants.
Hyperglycemia in the neonate

Objectives
This guideline is relevant to all staff working in neonatal units in the West of Scotland. Staff should also refer to relevant pharmacy monographs. When prescribing intravenous fluids or TPN staff should refer to the relevant guidelines
Hyperglycemia is more prevalent in preterm infants than term infants. The incidence of hyperglycemia is inversely related to birth weight and gestation. Hyperglycemia in preterm infants is linked to relatively high glucose intake, impaired insulin production by beta cells of pancreas, insulin resistance, immaturity of glucose transport system and small mass of insulin responsive tissues(2). Other important causes of hyperglycemia include sepsis, stress, pain, medications (inotropes and steroids) and neonatal diabetes.

Despite the high prevalence of hyperglycemia in preterm infants, significant glycosuria (3) (defined as ≥3+ on dipstick or >56mmol/L of glucose in urine) is relatively uncommon. Glucose filtered through kidneys is nearly reabsorbed completely by the proximal tubules. Tubular reabsorption becomes progressively incomplete as the blood glucose level rises. Tubular absorption is not as effective in preterm infants when compared to term infants. Despite these factors glucose does not spill significantly into the urine until the BG level is > 12 -13 mmol/L(2) . Preterm kidneys handle excretion of water and solutes separately. Nephrons reduce the free water excretion in response to significant glucose spillage to maintain serum osmolality within normal limits (3). The normal serum osmolarity ranges from 275 to 292 mmol/kg. The maximum concentrating capacity of urine in preterm infants is 600mmol/kg(4).
The level of BG leading to complications has not yet been defined. The most feared complication includes osmotic diuresis eventually leading to dehydration, weight loss, electrolyte imbalance and increased serum osmolarity eventually leading to osmolar changes in the brain. But osmolar changes are seldom seen with blood glucose level less than 20 mmol/L (5, 6). Each 1mmol/L increase in BG raises the osmolality by 1mmol/L. Hyperglycemia has been associated with neonatal mortality and morbidities although a direct causation has not yet been proved. In has been associated with morbidities including Retinopathy of prematurity (ROP), Intraventricular hemorrhage (IVH) (7-9) and prolonged hospital stay. The most studied association is that of ROP and hyperglycemia, although a recent meta-analysis did not show any relation between ROP and level of blood glucose after adjusting for variables (aOR: 1.08[0.97-1.20]) (10).
Limit the maximum glucose infusion rate to 12 mg/kg/min. A preterm infant requires at least 6mg/kg/min of glucose infusion. An addition of 2-3mg/kg/min helps in promoting protein anabolism. The maximum glucose oxidative capacity is 12 mg/kg/min beyond which glucose is converted to fat with increased carbon dioxide production and higher oxygen consumption(5). We recommend that the glucose infusion rate be limited to a maximum of 12mg/kg/min for preterm infants.
Provide an adequate supply of amino acids. Amino acids should be added early to the nutrition regime in VLBW infants and the goal should be to provide around 3.0-3.5 g/kg/day of amino acids. The minimum amino acids required for a positive protein balance is 1.5g/kg/day(11). Parenteral amino acid improves insulin release, helps with glucose homeostasis and prevents protein breakdown even with minimum glucose infusion rate of 4.2 mg/kg/min (12). Enteral nutrition should be introduced as soon as feasible as enteral feeds help in pancreatic release of insulin.
It should first be ensured that glucose infusion rates > 12 mg/kg/min is not being used, particularly where VLBW infants are requiring a high fluid intake to maintain hydration. It is also pragmatic to ensure that unnecessary infusions of glucose are not being used e.g. medications diluted in Glucose rather than Saline. If such simple measures do not control the hyperglycemia and blood glucose levels remain at or above the operational thresholds outlined above then further intervention is warranted.
Hyperglycemia may be treated either by the use of insulin infusions or a reduction in the glucose infusion rates. There is limited evidence about the long term benefits of these two approaches however there is some evidence that the use of insulin to treat established hyperglycemia helps to maintain nutritional intake and improve growth, including head growth, in the neonatal period (13). It should be noted that other studies using insulin routinely, to maintain tightly controlled normoglycaemia, resulted in a frequent incidence of hypoglycemia and this practice is not recommended in this guideline. Studies looking at insulin infusion for hyperglycemia are heterogeneous in various aspects, including the definition of hyperglycemia, timing of initiation of insulin infusion, and duration of insulin infusion (14-19). Consequently the treatment thresholds recommended in this document are consensus statements.
Where treatment with insulin is initiated, blood glucose levels must be monitored regularly to avoid hypoglycemia. Insulin should be reduced / withdrawn once glucose levels fall below these thresholds rather than waiting for normoglycaemia to be achieved. Some infants are refractory to insulin therapy, due to immaturity of glucose transportation, and may require a reduction in glucose infusion rates if hyperglycemia persists.
Glucose infusion rate reduction can be done either by reducing the total volume of fluid or by reducing the concentration of glucose. However, when using multi-component TPN infusions, reductions in fluid infusion rates may also reduce calorie and protein intake. In addition, the ELBW babies at greatest risk of hyperglycemia frequently need high fluid infusion rates to maintain adequate hydration. Therefore to reduce glucose infusion rates in babies with persistent hyperglycemia it may be necessary to order TPN solutions with a lower concentration of Glucose (e.g. 7.5%).
5.1 blood glucose measurement: Blood glucose should ideally be measured using a blood gas analyzer or laboratory values where a gas analyzer is not available. Other point of care glucose analyzers are less accurate than the above methods but are sufficient for monitoring hyperglycemia once the initial diagnosis is made.
5.2 Diagnose and treat underlying disorders including iatrogenic excess glucose delivery, sepsis, stress, medications and neonatal diabetes.
5.3 Management
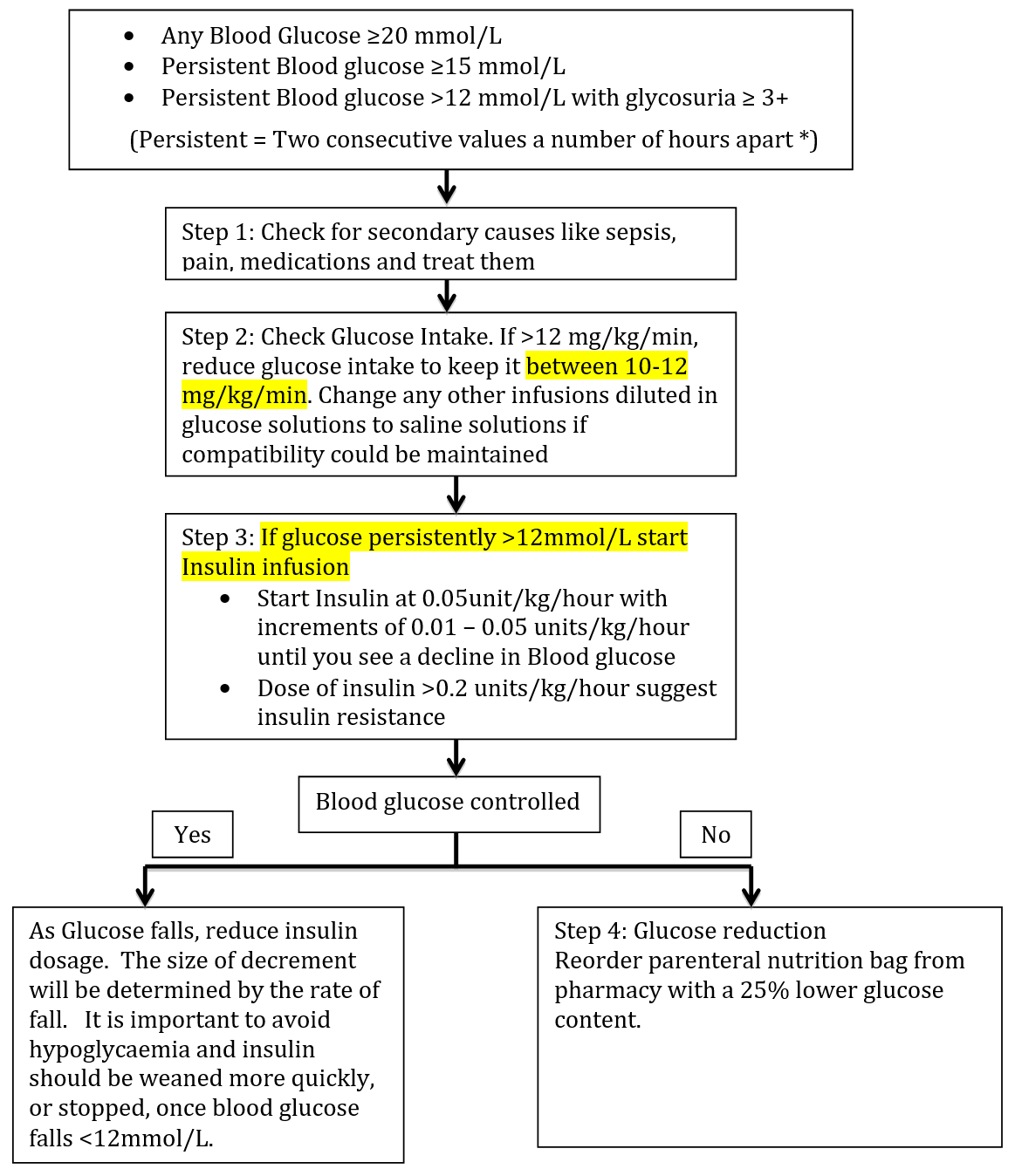
Consider interventions for any baby whose blood glucose levels exceed the following operational thresholds.
- Any Blood Glucose measurement of ≥20mmol/L
- Persistent Blood Glucose values of ≥15 mmol/L
- Persistent Blood Glucose values of > 12 mmol/L with glycosuria ≥ 3+ on urinary dipstick testing
* NB – Blood glucose may be transiently raised following a stressful event such as reintubation or line insertion. When making a decision to initiate treatment the clinician should consider whether the hyperglycaemia may have been caused by such an intervention. If so, it is reasonable to repeat the measurement before initiating treatment. The interval between the initial sample and the repeat will be determined by the level of blood glucose and the rate of rise.
If the baby has refractory hyperglycemia above these levels, consider monitoring serum sodium, urine glucose, urine osmolality if available and daily weights to look for evidence of osmotic diuresis.
Step 1: Check for secondary causes of hyperglycemia and treat them.
Step 2: Calculate the glucose infusion rate: (Glucose % × ml/kg/day of glucose solution) divided by 144. If the infusion rate is > 12 mg/kg/min (this equates to > 180ml/kg/day of standard TPN solution) adjust the glucose intake to keep the glucose infusion rate <12 mg/kg/minute. Consider changing infusions diluted in glucose to saline dilution if compatibility permits.
Step 3: Insulin Infusion
a) Type of Insulin: Actrapid
b) Please refer to the local pharmacy policy for preparation of insulin infusion. 2 insulin infusion rates are given with increments of either 0.05 U/kg/hour, or if finer control is required, 0.01 U/kg/hour.
c) Before starting infusion prime the line and leave for 10 minutes as insulin adheres to plastic. For this reason, if blood glucose fails to show a decline after the first check, check again in 2-4 hours before increasing the insulin infusion rate.
d) Administration: Start insulin infusion at 0.05U/kg/hour and titrate upwards by 0.01-0.05U/kg/hour every 2-3 hours until blood glucose begin to decline.
e) Monitoring: Check blood glucose after 1 hour with every insulin dose change and then assess blood glucose 2-3 hourly while on insulin. Monitor potassium levels every 12-24 hours.
f) Discontinuation: When a baby is on Insulin it is very important to avoid hypoglycemia. Hence frequent monitoring is required. As blood glucose starts to fall, reduce the insulin dose. The size of decrement will be determined by the rate of fall. It is important to avoid hypoglycaemia and insulin should be weaned more quickly, or stopped, once blood glucose falls <12mmol/L.
Step 4: Glucose Reduction
This may be required for infants with persistent hyperglycemia and a poor response to insulin. It can be accomplished either by reducing the total volume of glucose containing solution or by reducing the glucose concentration.
For infants on pre-prepared TPN infusions the glucose infusion rate cannot be reduced without adversely impacting the infant’s requirements for hydration and nutrition. For these infants, a new bag of TPN with a glucose concentration of 7.5%, should be ordered from pharmacy at the first opportunity. No alterations should be made to TPN at ward level.
For infants on a concentrated TPN solution, some reduction to glucose intake may be achieved by adjusting the additional fluid being provided to meet the infant’s fluid requirements. Subsequent bags of TPN may be ordered with a 25% reduction in glucose content.

