PDA management in preterm infants: general
An unrestrictive PDA in a premature infants can cause: progressive cardiac failure, prolonged ventilator dependence and can contribute to chronic lung disease (1,2). Additionally, associations between feed intolerance, necrotising enterocolitis, hypotension (3) and cerebral perfusion (4) are established. There is considerable animal evidence that PDA adversely affects lung compliance (5,6).The earliest (1970s) clinical trials demonstrated a reduction in ventilator support and hospital stays following surgical ligation(7). With improvements in perinatal care the optimal management of the PDA has been more controversial(8) but whilst there is no place for universal prophylactic PDA closure, medically or surgically, PDA ligation still has a role for preterm infants who (with) have persistent moderate/large PDA, who develop cardiac failure and who are not responsive to medical therapy.
Despite 50 years of clinical trials there is no clear picture or national/ international guidance on the management of PDA. After the earliest clinical trials, most randomised controlled trials (RCTs) either focussed on refinement of treatment or prophylactic treatment to reduce periventricular haemorrhage and improve developmental outcomes. Recent Cochrane reviews (9,10) of the more recent “treatment versus no treatment “demonstrate reductions in hospital stays but no other differences in outcome mortality of short term outcomes. Apparent negative results of trials have resulted in a therapeutic nihilism and a drift away from treatment. However the Cochrane authors acknowledge the heterogeneity of gestational age (GA) of infants included, potential selection bias and the need for appropriately targeted and powered trials. Despite this, PDA management (primarily medical but also surgical in selected populations) remains a standard in many institutions with the best neonatal outcomes. Evidence to support this approach comes from quality improvement studies strongly suggesting that moving away from treating PDA results in increasing rates of BPD and more vasopressor treatment of hypotension in the first 2 weeks of life(11,12). Sub analysis of the prophylaxis studies report reduced rates of PVL and better later developmental outcomes with prophylactic indomethacin (13) and MRI brain studies demonstrate lower brain volumes in infants with prolonged PDA exposure (14). Most recently critical appraisal of recent RCTs highlights some of the challenges with subjecting PDA management to RCTs. Problems include wide variation in the selected study population, marked variation in shunt size, shunt exposure, problems with patient selection bias, treatment contamination of the control arms and relatively poor efficacy of medical interventions. Analysis of the most recent RCTs demonstrated only a 20% difference in PDA exposure between the treatment arms in some RCTs (15). In these circumstances analysis of the most recent medical RCTs (with negative findings) demonstrate a strong relationship between the duration of PDA exposure, ventilation and the development of severe grades of BPD (16,17,18,19)
PDA Ligation in preterm infants:
Evidence and outcomes
The situation for surgical ligation of the PDA is more complex. Since the USA National collaborative trial there have been no randomized clinical trials comparing surgical ligation to medical or no PDA treatment (20).
In addition to potential direct surgical complications (pneumothorax, Post Ligation Impaired LV contractility (PLIC), vocal cord (nerve) palsy) there are concerns that very early handling the preterm lung may also have unexpected adverse effects and increase the risk of BPD (21) so that that whilst prophylactic PDA ligation decreases NEC rates (22) it may increase BPD(23). However whilst follow up studies have demonstrated higher incidences of BPD and neurosensory impairment (24) a more recent report shows where appropriate risk adjustment is undertaken for case mix babies requiring PDA ligation the increased rates of adverse outcomes do not persist (25).
What is known is that surgical ligation, in contrast to medical therapy, definitively closes the PDA. It has been demonstrated to improve lung compliance (5), may reduce the incidence of NEC (22), is associated in the past and present era with success in getting patients off ventilators (26,27) and, after potential transient decline, improves cerebral perfusion (28).
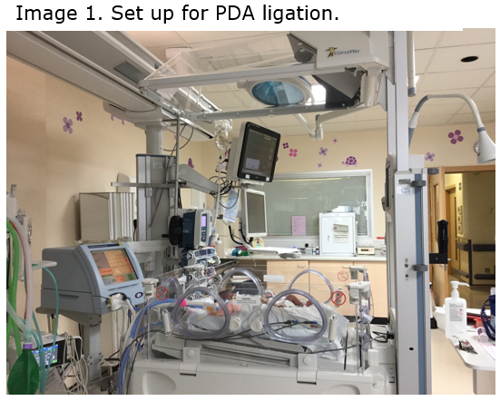
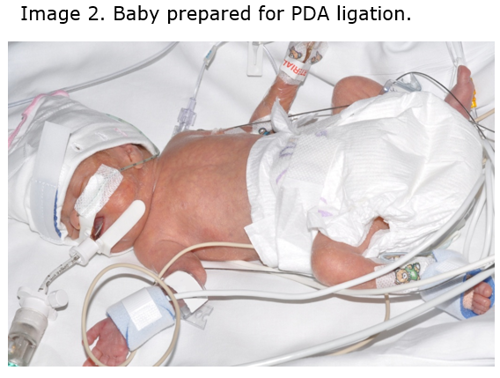
The approach around the world varies widely. Brooks et al, in 2005, reported an increase in mortality in infants < 28 weeks with PDA not responsive to medical management after losing a PDA ligation service (29). A very recent series from South Korea (median GA 26 weeks) reported that, in infants not responsive to indomethacin, if ligation was deferred from the first week of life until after 10 days of life outcomes were poorer. Earlier ligation was associated with reduced ventilator requirement and NEC (30). The overall mortality rate for this population was impressively low at 1-2 %. In contrast University of California in San Francisco reported that in infants not responsive to indomethacin for moderate to large PDA, deferral of PDA ligation from week 1 until 2-3 weeks of age, was well tolerated (31). Personal communication from Iowa (McNamara) reports excellent outcomes for infants < 27 weeks with a 41% ligation rate at 2-3 weeks using a haemodynamically significant grading system. In all series PDA ligation was undertaken in the NICU.
Conversely the UK data (26, 27) demonstrate a much later approach to PDA ligation. It is used almost exclusively for preterm infants with prolonged ventilator dependence with at a median age of around 5 weeks. The 30 day mortality rate was 4.8% and 3% respectively in the two epochs reported. Both studies report a median time to post ligation extubation of 5 days.
Adverse outcomes, PLICS and Post ligation Cardiac-Respiratory syndrome (PLICRS)
From Scottish data independent risk factors for death by 1 year were FiO2 >40% prior to surgery and lack of prior treatment with cyclo-oxygenase inhibitors (COI). Early post-operative deaths are associated with higher preoperative FiO2 > 60%. Significant complications such as perioperative pneumothorax (2.4%) and vocal cord palsy (4.8%) (26) are infrequent. Internationally reports of Post LIgation Cardiac Syndrome (PLICS) vary from to 30% to 8%. The syndrome is off sever lleft ventricular faiure and poor cardiac output with hypotensin and failing circulation. However the incidence of classic PLIC appears to be falling whilst but post Post LIgation Cardiac-Respiratory Syndrome is probably more common than previously appreciated. This can present with relative hypertension and deteriorating respiratory function 12-48 post operatively with a relative white out on chest X ray. This is also found following catheter closure of the PDA in very preterm infants. The mechanism is almost certainly due to increased systemic vascular resistance and poor diastolic function resulting in pulmonary oedema. For management see Figure 1.

Separate consideration should be given to the more mature infant, > 28 weeks, who are rarely reported in PDA ligation series. Most infants do not require management of the DA. However occasionally an atypical large and persistent DA is present resulting in heart failure often requiring extended periods of invasive or non-invasive respiratory support, failure to thrive and delay in developmental attainment such as sucking feeds. Experience suggests these infants derive considerable clinical benefit from PDA ligation.
PDA ligation referral guidance: a structured approach with robust clinical and echocardiographic assessment
For the reasons described above there are no UK or international guidelines on PDA ligation.
Consideration for ligation depends on robust clinical and echocardiographic assessment (Appendix 1 & 2) based on evolving international standards and timely referral.
Indications for referral
Potential clinical indications for consideration of referral for PDA ligation are listed below. They should be considered in conjunction with a full echocardiographic PDA assessment (Appendix 1) and considered against a clinical and echocardiographic triage score (Appendix 2). Only infants with clinical criteria and a moderate or large PDA, who are unsuited to or who haven’t responded to PGHS2 inhibitors, should proceed to ligation.
- Persistent systemic hypotension resistant to medical management
- Significant pulmonary haemorrhage
- NEC
- Renal failure or impairment
- Failure to extubate
- Cardiac failure not controlled medically (Hiflow/CPAP dependency, failure to thrive)
Echocardiographic assessment of the PDA (Appendix 1)
Echocardiographic assessment of the PDA can be challenging because of the 3D structure of the PDA and variability of shunt depending on clinical support and clinical condition. In addition reporting may also be subject to individual bias and understanding of the correlation of PDA diameter to the patient’s gestation and weight. Therefore it is important to have a robust system of assessment with standardised reports which grade the significance of the PDA.
It is not possible to measure the shunt directly but surrogates can be used looking at PDA diameter and flow patterns, measures of pulmonary blood flow (including LVO or LVO/RVO ratios) and measures of systemic flow. Using these measures PDA can be graded into small, moderate or large shunts (35). Moderate and large shunts can be considered for ligation if the above clinical criteria are met. It is important to recognise that the presence of an atrial shunt in the presence of a PDA can double the anticipated pulmonary blood flow. Atria communication >1mm in association with PDA.1.5mm are associated with increased measures of haemodynamic significance and worse clinical outcomes (37).
Clinical triage scoring system (Appendix 2)
A triage system to determine time to surgical ligation was devised in Toronto (36). Patients must have a moderate or large PDA but triage is based on the illness severity. In Toronto category 1 patients were ligated within 24 hours, category 2 within 3 days and category 3 within 7 days. In Glasgow most cases have been historically category 3 but as we move to look after smaller infants, who may not tolerate medical closure we will need to reconsider this strategy.
Referral process
Patients should be referred to both the on call Neonatal Consultant at RHC and the on call Consultant Cardiologist. Where the need for PDA ligation is clear, arrangements will be made to admit to NICU as soon as possible (consider against the triage system). Where the need for ligation is uncertain and the referring unit has capability the baby could be presented at JCC remotely. TEAMS consult could also be considered or it may occasionally be possible for a cardiology review to be undertaken at the referring hospital.
Key Points
- Prolonged PDA exposure is associated with adverse outcomes such as reduced brain MRI volume, heart failure and BPD.
- Preterm PDA ligation is reserved for infants who have not responded to or who are unsuited to medical treatment (COI or PGHS2 inhibitors)
- Higher rates of adverse neurodevelopmental outcomes have been linked to PDA ligation but do not persist after risk adjustment.
- Extubation success post PDA ligation continues to be demonstrated in UK series
- International centres reporting good outcomes tend to ligate earlier then UK case series but ideally > 21-30 days of life.
- Post PDA ligation mortality is associated with increasing FiO2 at ligation: < 40% is favourable.
- Standardised approaches to echocardiographic and illness assessment are essential
- Referrals should be (triaged) based on a clinical triage (score) severity score (Appendix 3) where possible.
- Input by neonatal clinicians is important at JCC
- Ligation should be undertaken in centres with the ability to support post-operative cardiac and respiratory instability.