BUR – back up rate
ITime – inspiratory time
PEEP – peak end-expiratory pressure
PIP – peak inspiratory pressure
PIPmax – maximum set peak inspiratory pressure
TTV – targeted tidal volume
VG – volume guarantee
VTe– tidal volume
VTV – volume targeted ventilation
Volume Targeted Ventilation: indication and use in the Neonatal Unit

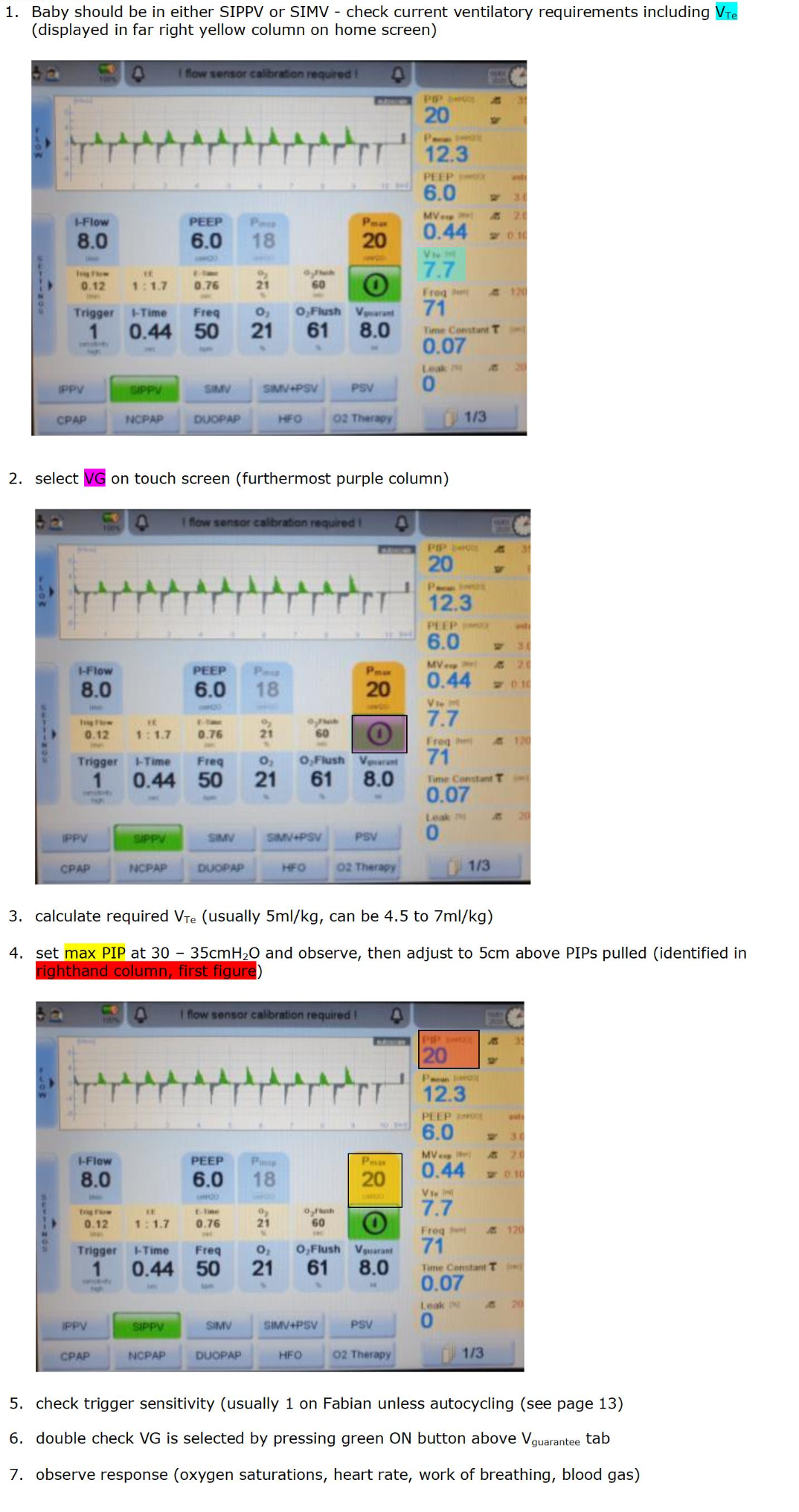
Flowchart (Fabian)
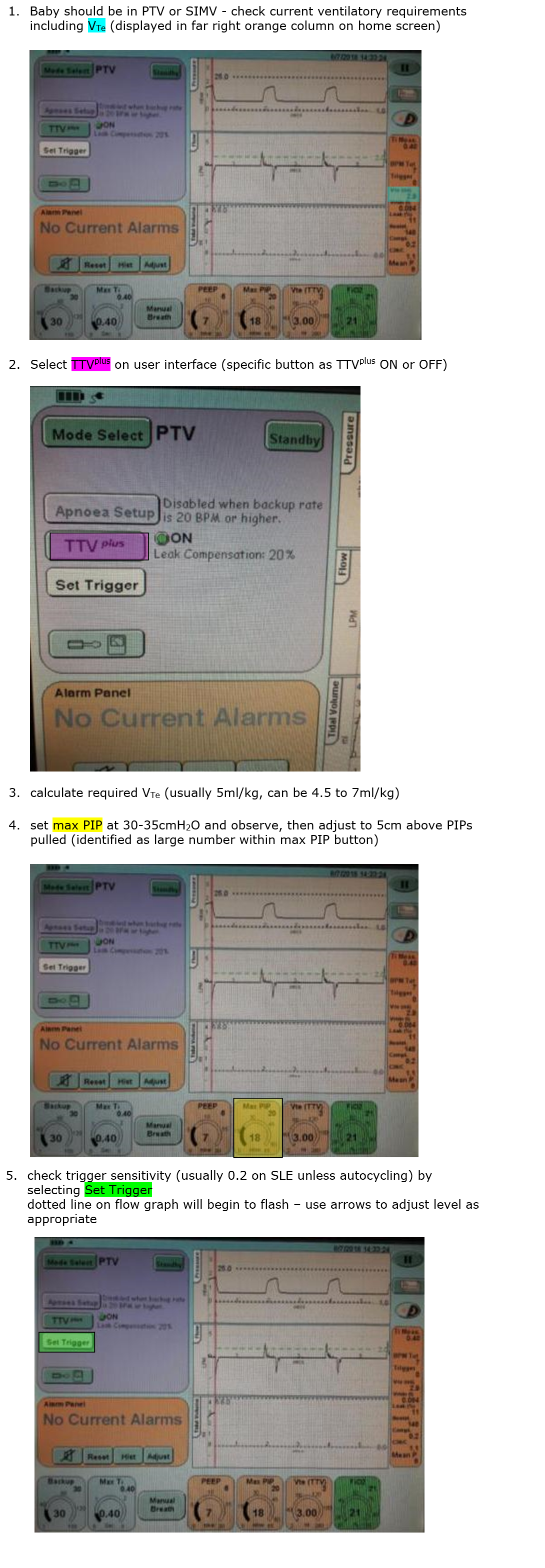
Flowchart for SLE 6000
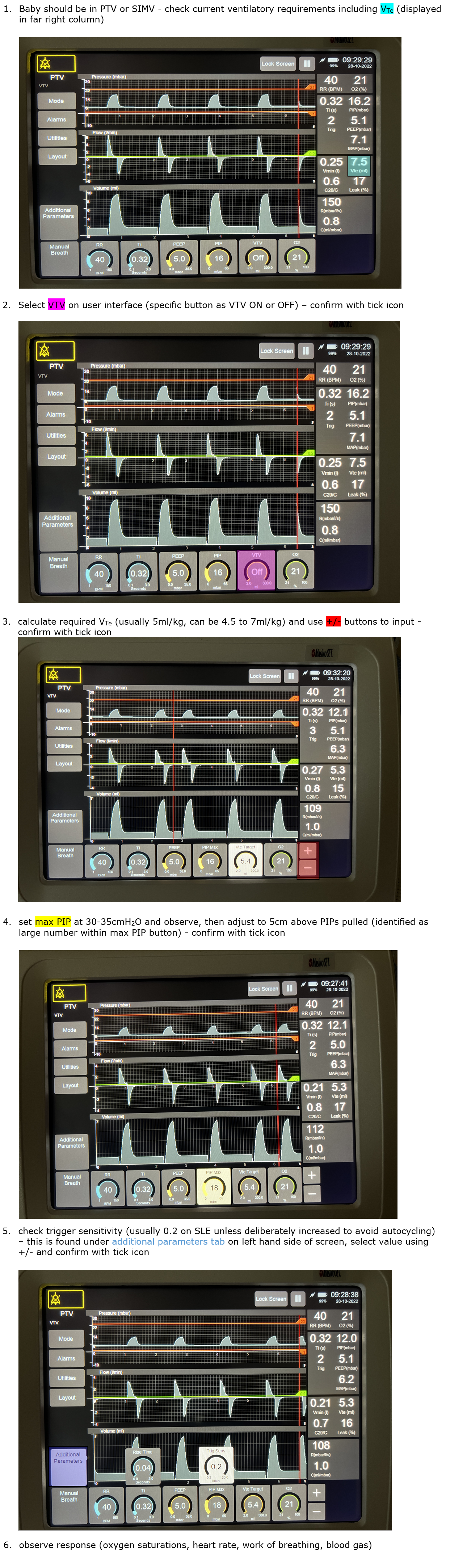
! Please note – all changes require confirmation with selection of tick icon !
In neonates, volume targeted ventilation is synchronised, volume targeted, pressure limited, time cycled ventilation where a set total volume of air is delivered to the infant using variable amounts of pressure depending on the flow volume measured at the end of the ETT during expiration.
This allows for changes in compliance and has been shown amongst preterm infants to have a reduced incidence in ventilator days, air leaks, CLD at 36 weeks corrected gestational age (CGA) combined with death and severe intraventricular haemorrhage (IVH) & periventricular leucomalacia (PVL) when compared with pressure-limited ventilation1.
The lungs of very preterm infants are exquisitely sensitive to injury for several reasons. These include surfactant deficiency, structural immaturity and a cartilaginous chest wall. Research in preterm lambs has shown that large distending lung volume and overdistension, rather than high ventilation pressures, can inhibit subsequent responses to surfactant treatment 2,3.
In Volume Guarantee (VG) or Targeted Tidal Volume (TTV), (the volume targeted ventilation modes on all modern ventilators), the operator sets a target expired volume (VTe). The ventilator measures the expired volume for each inflation and adjusts the peak inspiratory pressure (PIP) for subsequent breaths aiming to deliver the approximate required volume. Differences in one PIP to the next are minimised to a range of +/- 3cm H20 to avoid overdistension. Each inflation volume is limited to 130% of the previous expiratory volume and compensates for a degree of leak.
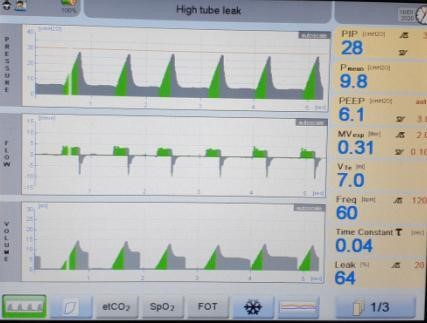
Figure 1: pulmonary graphics on VTV
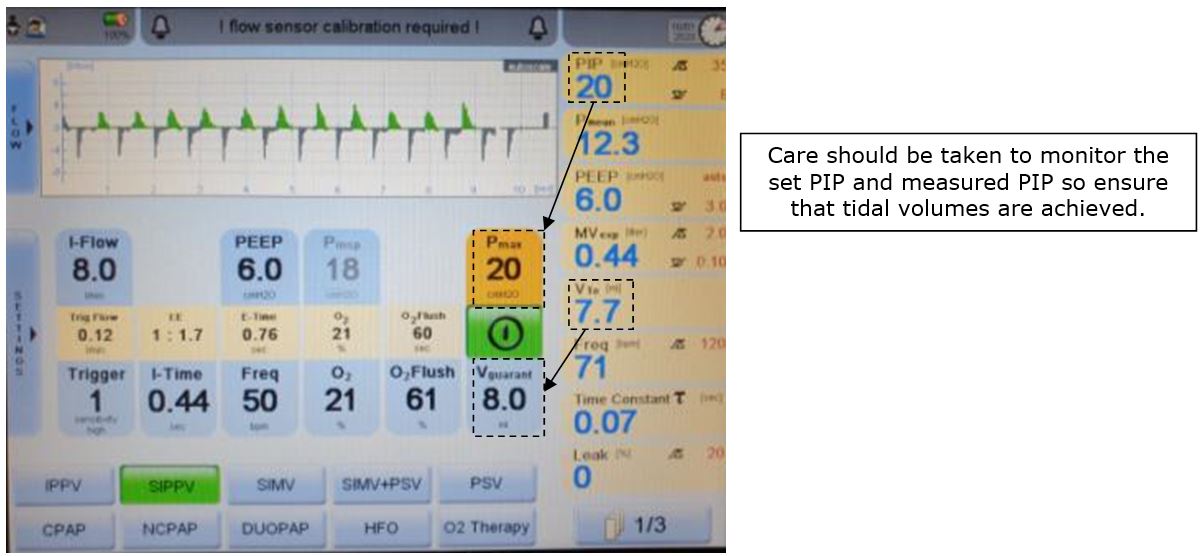
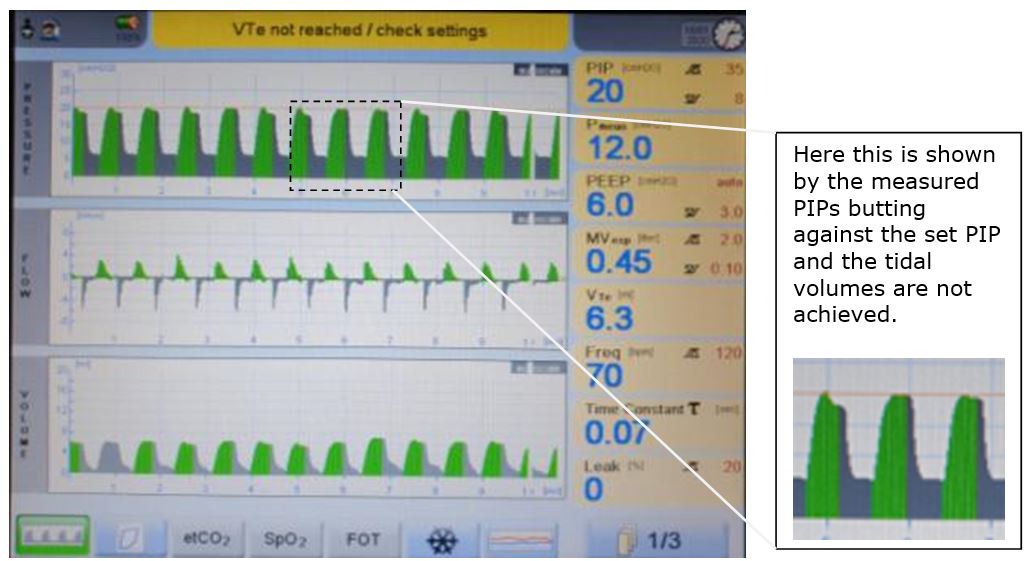
Figure 2: maximum PIP not set high enough
Ventilator Mode
Volume targeted ventilation is most suited to triggered ventilation modes, usually SIPPV though it can be used in SIMV.
The ventilator adjusts PIP for triggered and untriggered breaths separately and it is often noted that the PIP required for the same tidal volume for triggered breaths is much lower than that of untriggered breaths.
The set up of VTV is in addition to the standard set up of triggered ventilation and some good practice is discussed below.
Setting Target VT
Research quotes a range of tidal volumes in the preterm neonate from 3.5 to 8ml/kg4, 5. In practice, the optimum starting volume is probably 6ml/kg on the Fabian ventilator, particularly for infants under 1000g.
PIP Limit
The maximum set peak inspiratory pressure (Pmax) is not the same as the delivered PIP. The delivered PIP varies from breath to breath to achieve the set VT.
The maximum PIP should be set to allow the ventilator to adjust pressures appropriately to achieve the target volume but not to allow excessively high pressures when the ventilator cannot accurately determine the TV. Usually this would be around 5-10 above the current PIP and this does require user input.
Any higher and there may be little warning of changes in lung compliance.
Any lower and the tidal volume may not be achieved, leading to subsequent hypoventilation and atelectasis. In this instance the ventilator will alarm ‘low VTe’ as it will not be able to achieve the desired VTe with the PIP allowed.
There is no set numerical value required for the Pmax. Approximate values are provided in the set up flowcharts but these must be reviewed during this process and individualised to each baby.
Trigger Sensitivity
For preterm infants and to allow for maximum synchrony between baby and ventilator, the flow sensor trigger threshold should be set at its greatest sensitivity (1 on Fabian, 0.2 on SLE5000/6000)
Breaths can be inappropriately triggered by rain out (condensation in the circuit). This should be avoided by pointing the flow sensor plug upwards, the use of heated AND humidfied gases and intermittently clearing the ventilator tubing of any condensation.
Inspiratory Time
An adequate inspiratory time (Ti) is needed for sufficient delivery of the PIP selected. If it is too short, a high enough PIP will not be achieved for long enough to deliver the set volume. For most preterm infants this will be between 0.32 and 0.36 seconds.
Ventilator Rate
The set rate is a back up rate (BUR) whereby the ventilator delivers untriggered inflations, only if the baby’s own respiratory rate falls below this, recorded over a set time.
Generally this should sit low enough to encourage spontaneous respiration as these will require less ventilatory support. A back up rate of 40 to 45 breaths per minute is sufficient but may need increased in infants with poor respiratory drive.
Flow Rate
This is automatically set on SLE and Fabian ventilators but in the use of Drager models, should be 8 litres/minute.
PEEP
To maintain functional residual capacity, an adequate peak end expiratory pressure (PEEP) is essential. It improves oxygenation and prevents atelectasis. The optimum PEEP for intubated preterm infants is at generally 5 to 6cm H20. But higher settings may be required in certain infants e.g CLD, pulmonary haemorrhage.
When optimally applied to preterm infants, this ventilator mode lends itself to automatic weaning. As the baby’s lung compliance improves, the PIP reduces on a breath to breath basis rather than on steps guided by blood gases or oxygen requirement. Equally, if lung compliance is worsening, the ventilator will respond with higher PIPs to maintain the set VT.
In infants who are spontaneously breathing, and well synchronised on a patient triggered mode, the main adjustable variables will be the VT and oxygen concentration. Such infants will be setting their own rate.
Using the usual parameters of need for supplemental oxygen and CO2 clearance on blood gases the set VT can be adjusted to deliver more or less ventilation. This is usually done in 0.5ml/kg increments.
In practice, in those infants with good lung compliance, delivered VT between 4 to 6 ml/kg can often be delivered with low PIPs and little variation in delivered PIP. Therefore the PIPs ‘pulled’ can be a better indicator of the ability of an infant to be weaned or extubated once their requirement is less than 5ml/kg. In such cases, if the patient is triggering well with stable oxygenation and good gases, it is time to extubate.
Below these levels, the ventilator can be effectively providing CPAP via an endotracheal tube with a small diameter, and a corresponding marked increase in airway resistance, which can worsen atelectasis and respiratory distress.
In some infants, extubation cannot be considered for other clinical reasons e.g. poor respiratory drive, airway abnormalities. Here, pressure-limited ventilation (at a low PIP) may be more appropriate to prevent derecruitment.
However, this ventilation mode responds intuitively to lung compliance and so will allow for easier, earlier extubation in the majority of babies.
Common Alarms
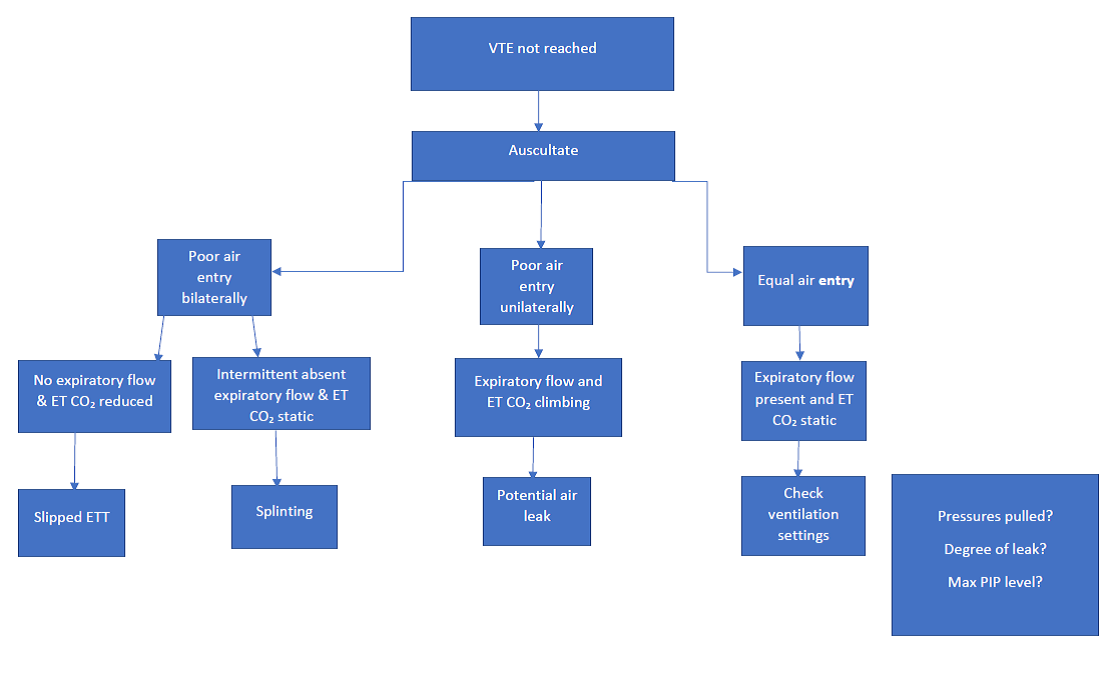
VT Not Reached
This can occur if:
- the Pmax hasn’t been set high enough (see figure 2).
In a well synchronised infant then you may need to increase the maximum PIP to allow the set VTe to be achieved (>30 - 35cm H2O). If PIPs above 30 - 35cm H2O are consistently being pulled, the infant may be requiring considerable ventilatory support and should be discussed with a consultant. - there is a problem with the baby or equipment.
Usual checks of the ETT and baby should apply with exclusion of tube blockage or displacement and air leak
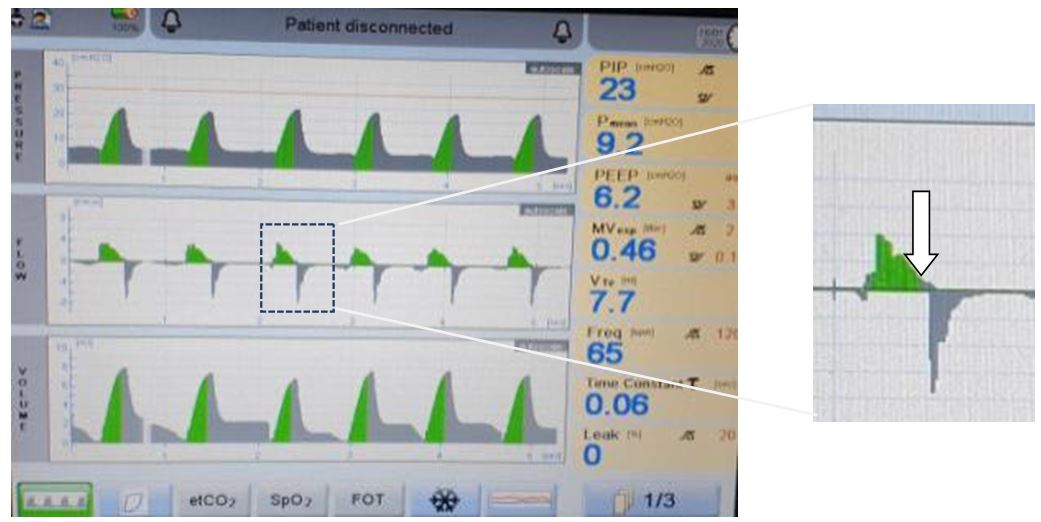
Figure 3: ETT displaced as seen on pulmonary graphics

- the baby is splinting.
This is active expiration against ventilator inspiration; it can also be thought of as diaphragmatic braking (see figure 3). It will appear as recurring drops in VTes despite increasing PIPs - the flow rate is too low.
This is solely a concern in the use of Drager ventilators as flow rate is automatically set on SLE and Fabian ventilators. the iTime is too short.
It can be assessed via the ventilator graphics.
On a pressure-time graph, an adequate Ti is demonstrated as a short plateau after the PIP is delivered then a return to baseline before expiration.
On a flow-time graph, if Ti is too short, the flow wave will end abruptly at the end of inflation before reaching the baseline and the tidal volume will have a sharp peak.
If too long, the pressure plateau will be held after inflation flow has ceased with no subsequent increase in VT.Figure 4: effect of inspiratory time
Too short
Too long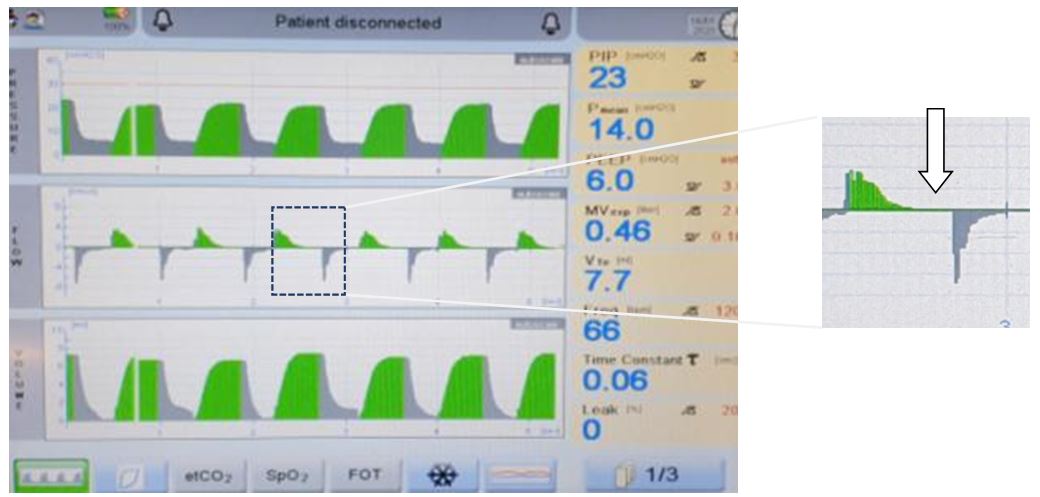
Figure 5: splinting as seen on pulmonary graphics

Leaks
Leaks around a neonatal endotracheal tube are common as they are usually uncuffed. This can affect the delivery of any type of ventilation. In VTV this is partially compensated by measuring the expired gas rather than the inspired gas as it is a more accurate measure of the actual tidal volume.
However with all ventilation modes, leak is overcome by delivery of higher flow and pressure to compensate for inspiratory flow that does not reach the lungs.
With VTV, the Fabian ventilator will tolerate up to 50% leak with appropriate PIPs delivered to this point. However beyond this range, there may be initial concerns that rising PIPs are due to worsening lung disease. Thereafter, with ongoing leak and falling measurements of expired VT, the PIP delivered may be insufficient to achieve the actual required volume with subsequent atelectasis and worsening ventilation.
It may be appropriate to replace with a larger diameter endotracheal tube.
Figure 6: leaks as seen on pulmonary graphics
In keeping with all modes of triggered ventilation, sometimes a baby does not do well on VTV. This may be caused by:
- An inappropriate iTime
Consider reducing this if long (>0.4 – 0.45 seconds). This should reduce interrupted expiration.
- A BUR too close to the baby’s spontaneous respiration rate
Reduce the rate to a minimum of 10 breaths per minute below the spontaneous rate.
- A baby in pain or distress
Consider analgesia or sedation - Autocycling
This is the inappropriate triggering of breaths due to causes other than the infant’s inspiratory effort. Causes include cardiac impulses, oscillation of secretions or humidity in the ventilator circuit or an inappropriate trigger sensitivity. This can be excluded by observing the baby’s spontaneous respiratory rate with a trial of a lower BUR. Solutions include adjusting the ventilator tubing, reducing rain out and adjusting trigger sensitivity as previously outlined.
Figure 7: asynchrony and interrupted expiration as seen on pulmonary graphics
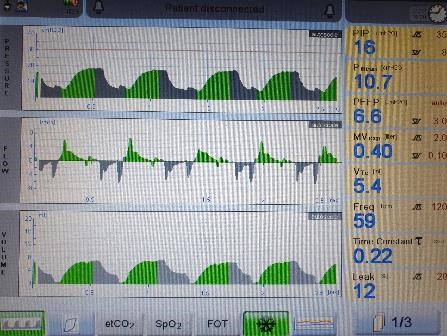
Figure 8: autocycling as seen on pulmonary graphics

Those ELBW babies most likely to benefit from VTV modes are those most likely to suffer common problems with endotracheal leak and splinting, therefore troubleshooting for these is of high importance.
Derecruitment
In some babies, despite the ventilator delivering the set VT with good synchrony with the patient, a rising oxygen requirement can be the first sign of lung derecruitment. A chest X-ray can be performed to check for small volume lung fields. A trial of pressure limited ventilation will help recruit partially collapsed lungs but an early return to volume targeted ventilation is then indicated to prevent barotrauma and hypocapnia as previously described.
Troubleshooting flowchart