4.1 Considerations
The decision to electively remove any chest drain(s) is a clinical one.
It should be ascertained that the chest drain is no longer required. That is, the original need for chest drain insertion has been resolved, such as evidence of adequate lung re- expansion or minimal serous fluid loss.
Written documentation by medical staff or ANP for drain removal specifying drain/drains to be removed for the correct patient.
If an x-ray is available pre drain removal this should be checked by Medical Personnel. If multiple drains in-situ, then medical personnel should ensure the correct drain for removal is identified and labelled before nursing staff remove drain.
The nurse should check the child’s vital signs, particularly their respiratory status. These should be stable before considering removal of chest drains and monitored closely throughout.
The patient’s blood results should be checked, in particular haematology and coagulation status should be available, before chest drain removal, as a low platelet count would result in excessive bleeding.
Other clinical evidence of bleeding in the child, such as oozing at invasive line or wound sites, should be noted as this may indicate clotting problems and should be highlighted to medical staff prior to ensure informed decision on removal is made.
If the child is receiving any anticoagulant or thrombolytic therapy, then they are at greater risk of bleeding if the chest drain(s) is removed. Protocols for pausing therapy briefly for procedures such as chest drain removal, should be adhered to. See anticoagulation guidance.
4.2 Indications
- Absence of air leak (pneumothorax)
- Drain losses are diminished to little or nothing
- Respiratory stable
- Chest x-ray confirming re-expansion of the lung
4.3 Pre-Procedure & patient considerations
- Patient should be fasted pre procedure as per medical personnel instructions - see local guidance (are specific)
*Fasting Guidance for Procedures on PICU Patients in PICU or Theatre
- Explain procedure to child and family
- Provide appropriate analgesia and sedation for the patient. Oral midazolam liquid can be prescribed by medical staff to be give pre procedure, please refer to BNFC under conscious procedure section for guidance and doses. If patient has NCA/PCA Morphine in situ background should be paused and boluses used for pain management, consult with Pain Team and/or Medical Staff. If no NCA/PCA then give appropriate prescribed analgesia.
- If pacing wires and drain to be removed, remove pacing wires first (see anticoagulation guidance)
- If patient is receiving anticoagulant medication refer to local guidance if applicable (link)
- Ensure there are enough staff to assist and carry out procedure, (Minimum of 2 competent nurses).
4.4 Equipment
- Clean trolley
- Gloves – sterile & non-sterile
- Disposable apron
- Disposable visor mask/goggles
- Sterile Dressing pack: inc. drape, gallipot, gauze.
- Chest drain site & wound site cleaning solution: 0.9% sodium chloride (Prontosan may also be used)
- Stitch cutter
- Steri strips
- Occlusive dressing for chest drain wound site: E.g. Duoderm®
- Chest drain clamps (minimum x2 per drain))
- Clinical waste bags (x2) & large sharps bin
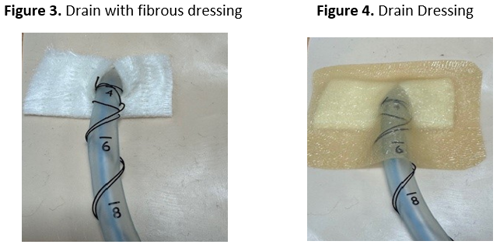
*Dressing for mediastinal wound site and chest drain site if removing mediastinal drains post-cardiac surgery (Duoderm® & UrogoClean)
4.5 Procedure - Chest drain removal
- Assemble equipment and take to bedside once analgesia/sedation has taken effective
- Identify staff to help and identify specific roles - see appendix 5.5 for roles
- Ensure patient is in optimal position lying in bed 30 degree head tilt and drains are easily accessible.
- Perform hand hygiene
- Open dressing pack and other equipment to clean trolley
- Don appropriate PPE for procedure
- If drain is connected to suction, then stop suction and clamp drain
- Clamp chest drain(s) being removed (Figure 13) and all other drains connected to, or sharing the same chest drainage unit. If only one drain is removed and other on the same connection/drainage unit are still in situ, the drainage tubing to the removed drain must remain clamped following removal.
- Removal all dressing from the area and examine site. Identify drain anchor sutures (if any/cardiac patients) and the purse string and expose the ends, unwind in preparation for assistant to tie.
- Remove disposable gloves, preform hand hygiene and don sterile gloves
- Clean around the catheter insertion site with appropriate skin cleaning solution
- Together with assistant, identify anchor suture and purse string
- Ensure the assistant and patient are ready
- Prepare purse string for tying once drain has been removed
- Cut anchor suture and ensure drain mobile and ready for removal
- Remove drain:
- nurse using one hand to ‘brace’ either side of the chest drain site, should start to remove chest drain smoothly and briskly with other hand.
- If the child is old enough to understand (and not on mechanical ventilation) they may be asked at this stage to take a breath and hold it as the drain is removed (a few practice breaths may be tried first). Once the drain is out they should be encouraged to breathe normally.
- If the child is receiving inhalational anaesthetic for chest drain removal, please communicate with doctor administering anaesthetic when chest drain about to be removed.
Note: If at any point the drain does not come out easily or if there is an excess of tissue/omentum, then stop procedure, apply occlusive dressing and inform medical staff immediately.
- As drain is removed the assistant should tie the wound suture firmly and securely to close drain site, ensuring the suture is not pulled too tight
- As soon as drain is removed and wound site closed, pressure should be applied with a Prontosan swab over the site briefly, then remove and quickly inspect the site. If closure of site does not look complete, then steri-strips should be applied.
- If removing two drains (E.g. mediastinal) then repeat the above procedure (remember to keep clamps on until all drains to come out have been removed).
- Once drain(s) removed, the site(s) should then be checked, cleaned again, steristrips applied (if required) and covered with a suitable occlusive dressing (E.g. Duoderml® +/- Urgoclean).
- In certain circumstances children with more than one drain on the same drainage system may require removal of only one of these drains.
-
- In these cases follow above procedure, keep chest drain clamps on all drains, change connectors (if applicable) and do not remove clamps until remaining drains are connected back to the underwater seal unit.
- Once underwater seal established on remaining drains, remove clamps and recommence suction (if required).
- Ensure child comfortable and positioned upright after procedure.
- Note and document child’s vital signs, colour, air entries, oxygen saturation, respiratory rate and effort post drain removal.
- Arrange for chest x-ray post drain removal if requested by medical staff** Observe patient closely following removal for signs of pneumothorax/deterioration and alert medical staff immediately.
- Remove chest drain clamps and keep for re-sterilisation. Dispose of removed chest drains, drainage system, dressing pack and aprons and gloves into clinical waste bags (orange) x2, then place in large clinical waste bin.
**Follow Removal flow chart for specific roles see appendix 5.5
4.6 Further Information and precautions
Sometimes omentum may come out with the chest drain being removed. If this does happen, pause procedures, clean site and apply dressing and inform medical staff immediately.
Occasionally the chest drain wound site may not have a wound closing suture (E.g. drain inserted as emergency by transport team prior to admission). In this instance, when removing drain ensure application of sufficient steristrips, occlusive dressing and document.
Post drain removal x-ray will only be considered on Consultant’s request. Follow POCUS (Point of Care Ultrasonography) in the first instance if the patient is showing clinical signs of pneumothorax.
Dressing post drain removal must be closely monitored and changed every 48hours until dry and skin healthy and healing. If signs of infection or oozing present the dressing may require to be changed more frequently, and a swab taken of the area. If stay sutures in place these should be remove on day 5 post drain removal.