Antibiotic choice
- NICE recommends benzylpenicillin and gentamicin as initial antibiotic choice
- Prescribe gentamicin as a once only medication in the first instance.
- N.B. A decision should be made by 36h whether to discontinue antibiotics OR to prescribe regular gentamicin dosage.
- Consider cefotaxime if there is evidence of meningitis
Duration of antibiotics
For babies with a strong clinical suspicion of sepsis, or proven sepsis.
NB – If there is strong evidence, or proof, of Early Onset Sepsis (EOS) the paediatric team should inform their Obstetric colleagues. This may help guide maternal therapy if the mother is also unwell.
These babies will be managed initially on the neonatal unit and treated according to the antibiotic guideline. Antibiotics should be commenced within 1h of decision to treat
Babies with proven sepsis will generally require a minimum of 7d antibiotics. Longer courses may be required dependent on microbiological results, or in the presence of meningitis – see separate guidance for antibiotic therapy.
In cases of clinically suspected sepsis, if the blood cultures remain negative, the baby has clinically improved, and the CRP falls to below 10, antibiotic therapy may be discontinued earlier in the course of treatment
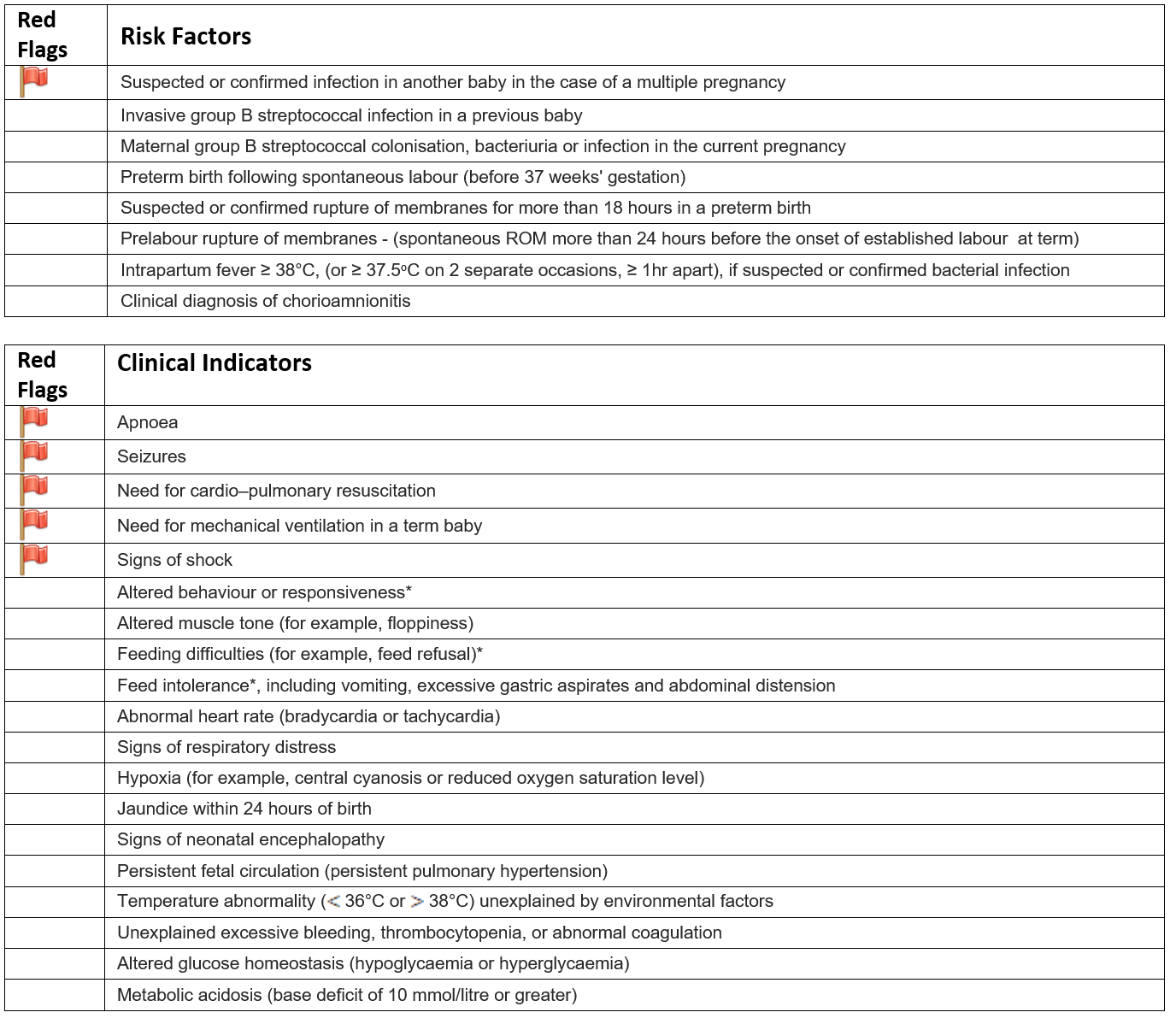
For babies with a ‘red flag’ OR two or more risk factors or clinical indicators BUT without a strong clinical suspicion of sepsis
NB – follow this guidance whether or not Intrapartum Prophylaxis has been given
These babies may be managed on the postnatal wards after their initial investigations.
Antibiotics should be prescribed as above. Repeat CRP should be taken 24h later to enable a decision to be made about the need for further treatment within 36h (NICE recommendation)
If both CRP tests (Baseline & 24h later) are <10 AND there are no clinical signs of infection then antibiotics may be discontinued.
If either CRP is >10 then Gentamicin should be prescribed on an ongoing basis commencing alongside the 3rd Benzylpenicillin dose. As above, the duration of treatment will be based on the results of blood cultures and/or the persistence of clinical signs.
N.B. - If continuing antibiotics for longer than 36 hours despite negative blood cultures, [due to persisting clinical signs] review the baby at least once every 24 hours. Consider at each review whether it is appropriate to stop antibiotic treatment, taking account of:
- The level of initial clinical suspicion of infection and
- The baby's clinical progress and current condition and
- The levels and trends of C-reactive protein concentration
The decision to continue antibiotics in this context should be clearly documented.
For babies with a single 'non-red flag' risk factor or clinical indicator and no clinical evidence of sepsis.
For these infants we would recommend the following:
- Withholding antibiotics and observing the baby for 12-24 hours.
Parents should be informed about the risk factor which has prompted this recommendation. The parents should be told that the clinical examination has not identified any current signs or symptoms of active infection and that we will continue to monitor these clinical signs throughout the first day of life. (Most babies who develop EOS will become unwell in the first 12-24h).
We recommend that all such infants are observed for this period irrespective of whether intrapartum prophylaxis was given or not.
A parental leaflet will be provided which will explain this recommendation and to provide information about the signs and symptoms of infection in a baby.
If the parents are uncomfortable with the decision not to perform any additional investigations, or treat with antibiotics, then this should be taken into account when planning the baby's care. At the discretion of the medical staff the baby could be managed in the same way as babies with multiple risk factors or clinical concerns as outlined above.