COVID-19 Theatre Processes RHC Glasgow
Objectives
RHC Glasgow Theatres & Anaesthetics: Guideline for Theatre Processes During COVID-19 Pandemic
This guideline details processes for RHC theatres related to COVID-19
Scope
Some of this guidance differs from measures in ED or other hospital areas due to the different patient processes & patient flow through theatre. Much of the information will NOT apply outside of theatres.
Audience
All theatre personnel & staff preparing patients for theatre

RHC guideline for COVID-19 patient pathway in ED and ward admissions is available here.
Case definition
Case definition is acute onset of any of the following symptoms:
- Fever >37.8
- Persistent cough (with or without sputum),
- Loss of sense of smell / taste
In addition, the RHC ED & in-patient pathway includes the following symptoms:
- hoarseness
- nasal discharge or congestion
- shortness of breath
- sore throat
- wheezing
Be aware that COVID-19 may present with other symptoms. If in doubt discuss with another consultant. Fever alone may be attributable to the surgical condition and should be considered in that context.
For COVID-19, the following procedures are reported to be aerosol generating and are associated with increased risk of respiratory transmission:
- tracheal intubation, extubation and related procedures
- manual ventilation
- tracheotomy or tracheostomy procedures (insertion or removal)
- bronchoscopy
- dental procedures (using high speed devices such as ultrasonic scalers or high-speed drills)
- non-invasive ventilation (NIV); Bi-level Positive Airway Pressure Ventilation (BiPAP) and Continuous Positive Airway Pressure Ventilation (CPAP)
- high flow nasal oxygen (HFNO)
- high frequency oscillatory ventilation (HFOV)
- induction of sputum using nebulised saline
- respiratory tract suctioning
- upper ENT airway procedures that involve respiratory suctioning
- upper gastro-intestinal endoscopy where there is open suctioning of the upper respiratory tract beyond the orophayrnx
- high speed cutting in surgery/post mortem procedures if this involves the respiratory tract or paranasal sinuses
The available evidence relating to Respiratory Tract Suctioning is associated with ventilation. In line with a precautionary approach, open suctioning of the respiratory tract regardless of association with ventilation has been incorporated into the current (COVID-19) AGP list. It is the consensus view of the UK IPC cell that only open suctioning beyond the oro-pharynx is currently considered an AGP i.e. oral/pharyngeal suctioning is not an AGP.
Certain other procedures/equipment may generate an aerosol from material other than patient secretions but are not considered to represent a significant infectious risk. Procedures in this category include: administration of pressurised humidified oxygen; administration of medication via nebulisation.
Use of PPE must be discussed as part of the theatre brief and theatre staff should make their own risk assessment regarding PPE use.
Air changes / pause times in RHC Glasgow:
|
Area |
Air changes/ hour (data from estates) |
Time (minutes) for 99% airborne contaminant removal |
|
Laminar flow theatres1 |
25 |
11 |
|
Standard theatre |
25 |
11 |
|
Anaesthetic rooms |
15 |
18 |
|
MRI / CT |
15 |
18 |
|
Theatre recovery |
6 |
46 |
|
Theatre reception |
6 |
46 |
|
Staff Rest areas |
2.5 |
138 |
|
PICU clinical area |
10 |
26 |
|
ED Resus |
6-8 |
46 |
Ventilation in both laminar flow and conventionally ventilated theatres should remain in full operation during surgical procedures where patients/individuals have suspected/confirmed COVID-19. Air passing from operating theatres to adjacent areas will be highly diluted and is not considered to be a risk.
Reference: https://publichealthscotland.scot/media/3361/1_covid-19-operating-theatres-faqs.pdf
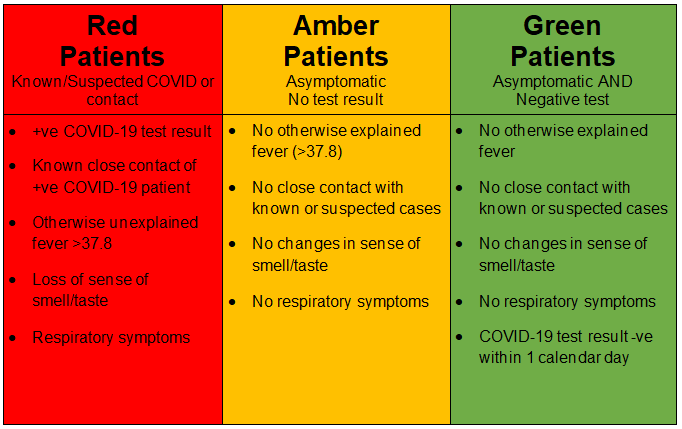
All patients referred for surgery should be checked against the case definition for COVID-19.
Elective patients and their household will be screened for symptoms and contacts, AND have a COVID test done within 1 calendar day of admission.
Emergency patients will have a COVID test taken as soon as possible after a decision is made for surgery.
Selected patients are screened regularly (eg PICU). In these groups of patients, the most recent result can be used to determine pathway.
The decision to proceed with an asymptomatic patient using the amber pathway while awaiting a COVID test result should be made jointly by surgeon, anaesthetist and theatre practitioner. This should take into account urgency of surgery, theatre availability and likely timing of COVID test result.
Where all attempts at obtaining a pre-op COVID swab have failed (e.g. autistic patient), a decision may be made to proceed using the amber pathway. Consent should be obtained for taking a swab for POC test following induction of anaesthesia. If negative, the patient can then be moved to a green pathway.
Point-of-Care PCR testing is available in theatre (and ED) and can be used to facilitate the green pathway particularly for emergency patients. This should be requested via the Coordinator for Theatres on 84383 Monday-Friday 8-6, and via 84852 out of hours and at weekends.
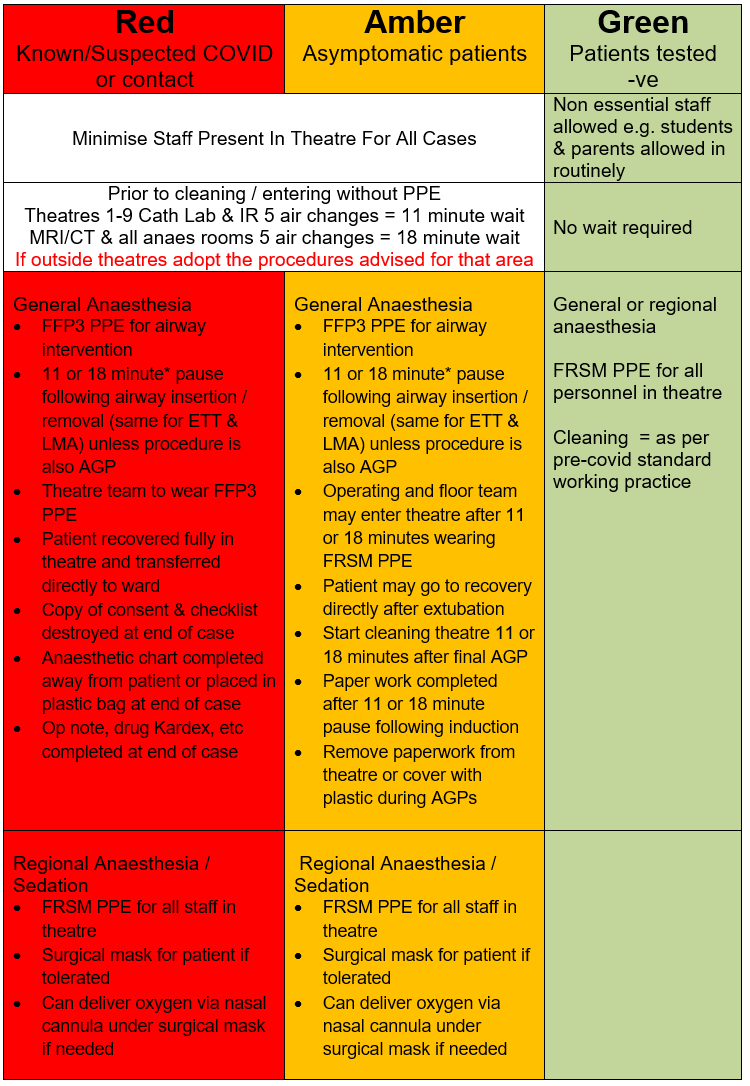
In the case of patients who have COVID-19, careful MDT discussion is required to decide which patients should and should not be coming for surgery, i.e. only those requiring emergency or urgent surgery. Ideally surgery should be delayed until patient has recovered from COVID-19 illness.
Theatres must be informed in advance if patient being booked for theatre has COVID-19 infection – phone theatre booking extension 84852.
Patient will be transferred from ward (via reception but not stopping) to designated theatre
Patient will be anaesthetised and fully recovered in theatre.
Anaesthetic room will not be used.
Following recovery in theatre, patient will be transferred directly to ward.
The theatre coordinator will limit corridor traffic during treatment of known or suspected patients.
Patient placement
Commonly this will mean patient is scheduled at the end of a list as per longstanding policies for other infectious cases. Consider using another theatre if available or out-of-hours
Prior to surgery
Designate a senior nurse controller for the area to ensure the following:
- Adequate and appropriate staffing including for substitution depending on length and complexity of case:
consider - additional anaesthetists, anaesthetic assistants, surgeons, theatre practitioners - PPE understood and trained. Locations for donning and doffing agreed.
- Roles understood
- Environment controlled
- Thorough Team Brief
- Patient transfer route
- All automatic doors in theatre switched off.
- Signage at entrances to theatre indicating RED theatre.
- Check if image intensifier is required and inform Radiology.
- Log staff undertaking case on Opera. Include COVID-19 status in free text.
- Control and log breaches of PPE on Datix – phone 84315 which will prompt for dataset.
Theatre Brief
Senior anaesthetic and surgical staff in order to expedite procedure. Consider sedation/regional / local anaesthetic to avoid AGPs.
Personal Protective Equipment
Use full airborne PPE whenever attending to the patient in theatre:
- Gloves (not required to be sterile unless performing aseptic or sterile practices)
- Long-sleeved, fluid resistant disposable surgical gown
- FFP3 mask – fit check after applying (cover filter and breath in, holding breath for 10 seconds. You should be aware of mask sucking on to your face with no air coming in round the seals while you hold your breath)
- Eye protection
All staff are required to train in the donning and doffing of PPE and will be fit tested for a FFP3 mask. Donning and doffing of PPE must be done in the correct order and in an unhurried manner.
Posters are displayed throughout theatres
All steps of donning are carried out before entering the COVID theatre.
The FFP3 mask must always be removed outside the patient’s room or after leaving theatre disposal room.
Pre-op Assessment
By anaesthetist, on ward.
Check paper and computer records first.
Low threshold for premedication.
PPE: FRSM, apron and gloves to enter patient room. Consider wearing a gown to provide some protection of theatre scrubs at this stage. Maintain distance of >2m from patient and parent. Avoid touching surfaces in room. Inform family of changes to normal theatre practice re parental presence in for induction and during recovery period.
Careful doffing of PPE to exit patient room.
Anaesthetic Preparation
BE PREPARED - EVEN MORE THAN USUAL!
Airway
Select age appropriate equipment/materials and place on trolley inside theatre.
Use cuffed endotracheal tube for intubation
LMA is acceptable if appropriate.
Consider using videolaryngoscopy – McGrath or C-mac depending on requirements.
HMEF filters at machine and patient ends of circuit (as is usual in RHC theatres).
Select additional equipment for airway management appropriate for that patient and place in plastic box on trolley shelf
IV access & Drugs
Prepare anaesthetic drugs in anaesthetic room, including vasoconstrictor and fluid boluses.
Err on side of preparing more than you think you will need.
Drugs in plastic tray
Single dose of NSAIDs is likely to be OK if no other contraindication.
Don’t forget local anaesthetic if appropriate.
Select range and ample supply of IV cannulae, syringes, needles, dressings.
Place all airway and IV equipment, and drugs inside theatre before patient arrives.
Place any emergency/additional drugs that may be required in a plastic box.
Other
Ideally, set up surgical instruments in advance and cover appropriately. This will reduce the time scrub staff need to wear PPE.
After a patient is in theatre, drugs and other items can only be passed in on a tray onto a trolley. Avoid all touch contact. A member of the team in FRSM/droplet PPE will be in the anaesthetic room until after induction and then in prep room throughout the case for this purpose.
Any single-use equipment and all drugs (including CDs) must be disposed of in theatre. They must not be returned to the anaesthetic room.
Transfer to Theatre
PPE to be worn by team undertaking transfer: apron, fluid-resistant surgical mask with visor, gloves.
Theatre team including anaesthetic assistant to do transfer
Complete theatre checklist in ward. Bring all relevant documentation to theatre
Route cleared to minimise exposure.
Shortest route used.
Two designated COVID lifts are available to transfer patients from the wards in RHC. Lifts only require cleaning if AGP has occurred while in lift.
Patient should wear a fluid-resistant surgical mask where appropriate/possible. A Hudson mask may also provide some protection of staff
Patient should be transferred directly to theatre.
Ideally parents should not accompany the child to theatre. However this may be required to facilitate safe anaesthesia in a selected few patients – e.g. MLB.
Minimise transfers. Transfer from trolley to table, anaesthetise on table. Trolley will remain in theatre. For adult-sized patients it may be safer to anaesthetise on the trolley then transfer after pause time following on from induction.
Induction & Intubation
Intubation is an aerosol generating procedure (AGP), so full respiratory PPE as above must be used. Minimise the number of staff in the theatres at intubation while recognising that additional members cannot be added at short notice.
- Induction in theatre
- If parent present (and this should only be in selected cases), they should wear FRSM, theatre gown, shoe covers. They should be prepared to leave during induction, before AGP starts. A member of staff should be designated to accompany them out.
- Patient should wear a surgical face mask if appropriate/possible before start of anaesthetic induction.
- Consider 2 anaesthetists present at induction, one for airway, one for IV access & drugs, and one anaesthetic assistant. Consider anaesthetic assistant in full PPE in anaesthetic room to assist if required.
- Preoxygenate if possible.
- Don’t switch on bair hugger until after AGPs are completed.
- Consider IV induction vs gas induction - choice should aim to minimise coughing / distress. Premedication will help.
- LMA may be used if appropriate.
- Minimise bag-mask ventilation and tidal volume as this might generate aerosols
- Consider using Videolaryngoscopy (McGrath or C-Mac) to maximise anaesthetist distance from patient.
- Avoid ventilation until ETT cuff is inflated. Use cuff pressure monitor to inflate cuff. Do not get close to patient to listen for a leak. If an un-cuffed ETT is used, consider placing a throat pack to minimise effect of leak.
- Confirm ETT placement with ETCO2 trace and chest wall movement. There are single-use stethoscopes, but these are best avoided as difficult to use with PPE and risk of self-contamination.
- PPE must be continued after intubation.
Intraoperative Management
- Minimise traffic
- Computers are available in theatre for documenting care, viewing x-rays.
- Communication via phone in theatre should be kept to a strict minimum. Walkie-talkies are available for easier communication. Use phones on loud speaker to reduce self-contamination. Use runner to communicate with those outside theatre during case.
- Plan and avoid time critical manoeuvres with associated risk of PPE breach.
- Avoid ventilator disconnections.
- Consider using plastic sheets/drapes to enclose patient during AGPs if possible.
- If sterile procedure planned as part of anaesthetic (e.g. central line), doff gloves and gown into orange bin in scrub area, re-scrub and don sterile gown and gloves. Don’t change mask & googles/visor.
Extubation and Recovery
- Transfer patient to trolley before extubation
- Only keep minimum staff in theatre
- Attempt to minimise coughing to minimise generation of aerosols
- Use sugammadex if appropriate
- Extubate to facemask & circle or T-piece
- Consider using plastic sheets to minimise aerosol spread
- Full recovery of patient in the same theatre, minimum 11 minutes to allow aerosol dispersal
- Patients transferred back to the ward by theatre team via agreed routes after appropriate coordination with receiving ward
- PPE for transfer: FRSM, apron, gloves. Doff FFP3 PPE prior to transfer.
- There may be circumstances where due to lack of space in theatre, use of a recovery cubicle is required for part of the patient recovery period in order to expedite theatre cleaning and preparation.
Theatre Cleaning
- See Public Health document ““COVID-19 Guidance for infection prevention and control in healthcare settings”. Joint document issued by UK Public Health Agencies including HPS (Key document 3 – see above for link) for additional information including cleaning and disposal of waste.
- Wear droplet precaution PPE (surgical mask with eye protection, gown/apron and gloves) to clean.
- Phone Facilities 5555 to arrange terminal cleaning– ask for domestic supervisor for RHC.
This pathway should be used when a patient is asymptomatic, a COVID test result is NOT available, and surgery cannot be delayed.
Amber pathway infection control precautions are the same as for red pathway patients. However a separate pathway is required because these patients must be regarded as at risk of infection (as well as potentially infectious) and so must not be mixed with patients on the red pathway who have suspected or confirmed infection.
Point-of-care testing should reduce the need for the amber pathway.
Place patients at the end of a surgical list and where possible use a separate theatre.
The amber pathway may also be used for an elective patient where all attempts at obtaining a pre-op COVID swab have failed (e.g. autistic patient). In this case, obtain consent to take a swab for COVID POC test following induction of anaesthesia. If negative, the patient can then be moved to a green pathway during the episode of care.
Patients who are asymptomatic and have no household contacts, and who have a negative COVID test within 1 calander day before coming to theatre can be managed using droplet precaution PPE and standard pre-COVID theatre cleaning processes. Droplet precaution PPE is a FRSM, gown/apron and gloves. It can also include eye protection.
Change to reflect earlier section Selected patients are screened weekly. If a patient in this group has a negative result within one week of theatre and no COVID symptoms/contacts, they can be managed on the GREEN pathway.
Patients undergoing procedures involving sedation, regional anaesthesia or spontaneously breathing face-mask anaesthesia can be managed on the GREEN pathway regardless of COVID status or symptoms, provided the surgical procedure is also not an AGP. However, remember to consider the risk of conversion to general anaesthetic which would require an increase of PPE and a break in the procedure to facilitate airway management. At a minimum droplet precaution PPE must be worn.
Last reviewed: 16 August 2021
Next review: 16 August 2022
Author(s): Anne Goldie; Dannie Seddon; Ewan Wallace; Graham Bell; Teresa Jerome
Version: 15.1
Author Email(s): anne.goldie@ggc.scot.nhs.uk
Approved By: SOP approved by existing management structures / clinical director

