A correctly fitting rigid collar only provides between 40-80% restriction of neck movement when used on its own (Gavin et al 2003, Tescher et al 2007, Holla et al 2016). Those children with a suspected spinal injury and in a medically-induced coma, may need application of a collar (where clinically instructed), with the collar allowed to be loosened only when the child is on neuromuscular blockade (see RHC PICU: Traumatic Brain Injury guideline 2012).
If the instruction is to apply a cervical collar, then the cervical collar must fit correctly. If it is too small, the head may become flexed on the spine, if too large, the neck may be able to move in any direction and therefore the cervical spine is not immobilised [EPLS 2012].
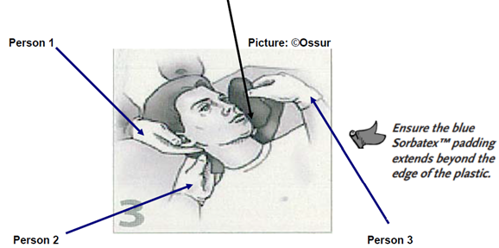
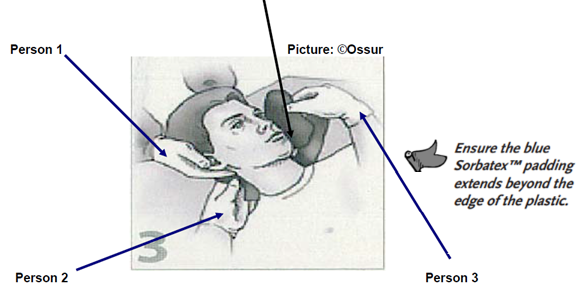
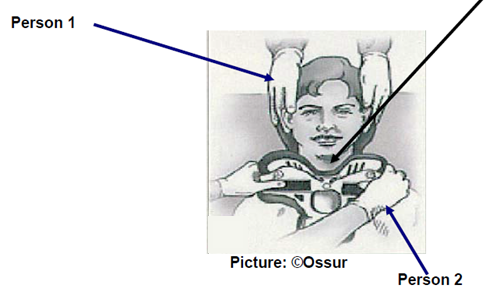
Three health care professionals are normally required to apply a two-piece cervical collar. (see following pages).
*The following is for an unconscious or calm/cooperative non-combative child
The Procedure*
The child should be told what is happening even if he/she appears to be unconscious. When using the Miami-Jr/Miami-J collar, follow the: Size it up, Scoop it up and Snug it up procedure (©Ossur)

- Person 1 Ensure manual in line cervical stabilization is maintained throughout. A jaw thrust could be adopted with the head held in the neutral position and the cervical spine immobilized, without extension of the head, i.e. the cervical spine is kept in-line with the rest of the spine. (See photos above).
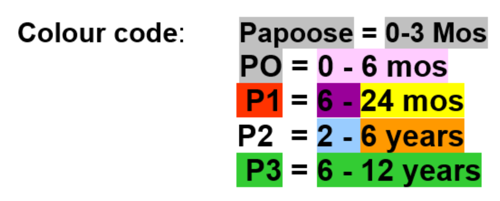
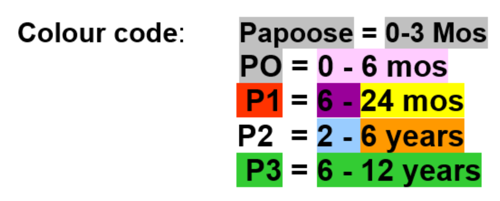
- Person 2 Size it up: Using the manufacturer’s method, select a correctly sized collar. Collars are colour coded according to size and are available in the PICU store cupboard (see below)
SIZING
Child UNDER 12 years old
Use Miami - Jr chart below
 (©Ossur)
(©Ossur)
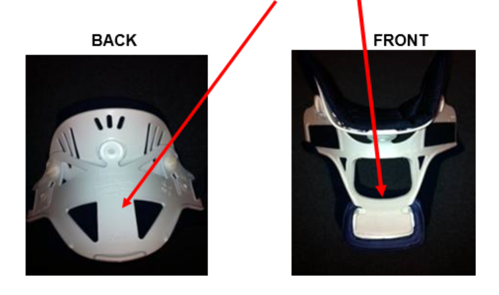
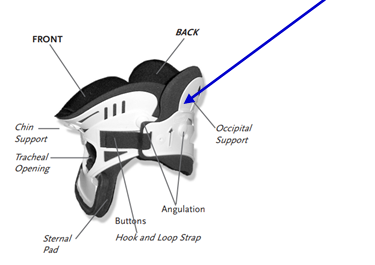
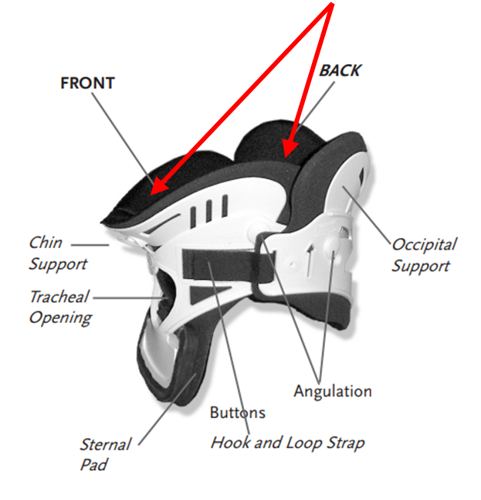
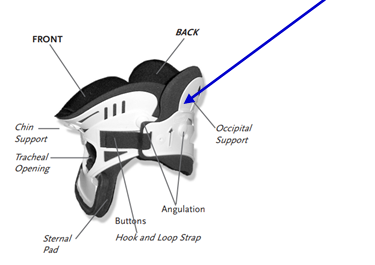
- Size it up: Once colour coded size collar chosen, fully unfold the collar and identify Back and Front pieces.
- Check child supine and head centrally aligned, and that child’s thorax is at appropriate height to accommodate the occipital prominence (this may require the use of a back pad such as Occian® AirWay pad™).
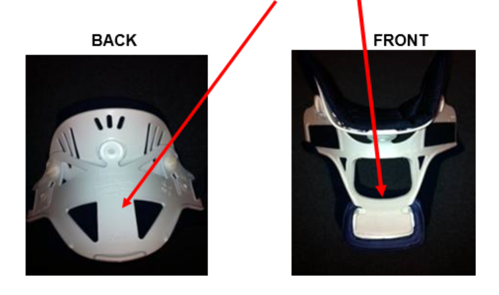
- Taking care not to cause movement or drag on the neck, slide the BACK of the collar behind the neck, push it down gently into the bed as you pass it through
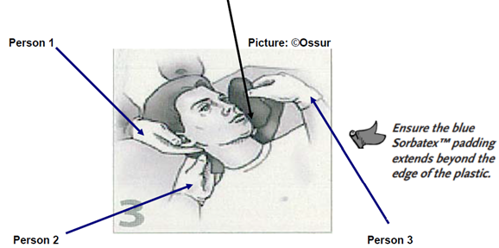
When using the Miami-Jr collar you will need a third person to assist with this (see above)
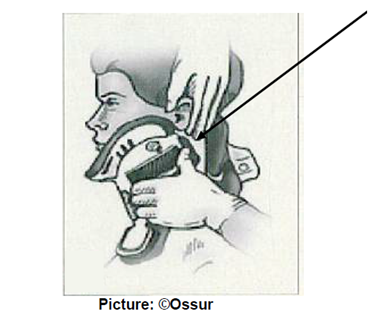
- Scoop it up: Once the Back piece of the collar is in situ and symmetrical, take the Front piece of the collar with both hands. Flare the sides of the Front of the collar and slide the collar UP the chest wall. Scoop the collar up under the child’s chin until the chin is seated in the centre of the chin piece (see picture below)

- Ensure the sides are oriented up towards the ears and off the trapezius. Note: Picture below rotated to show clearer positioning of collar. In PICU, child will be supine with manual in-line stabilisation.

- However, before the collar is fastened, the neck should be inspected for distended veins, tracheal deviation, wounds or subcutaneous emphysema. If possible, use a collar that allows the trachea to be seen and felt.
- Snug it up: Curl the ends of the collar so that they touch the neck. Fasten the Velcro strap and ensure symmetrical alignment and oriented as "Blue-to-Blue" to Front Velcro.

- Tighten Velcro straps alternately and check no gaps.
- NB: if the child can slip his/her chin inside the collar IT IS NOT SNUG ENOUGH.
Wrong fit:
- Reassess the correct fit of the collar. If the fit is correct secure the joining device.

Just right!
- If the fit is wrong, have Person 1 maintain manual cervical in-line stabilization, remove the collar, taking care not to cause neck movement. Select the correct size and recommence the procedure.
SIZING
Child OVER 12 years old
- Check Miami-J chart below to see which collar might be most appropriate

-
NOTE: Although the 250 XS is required by only 5% of the adult population, it is likely that many of our children over 12 in PICU will fit this collar. However, there should be at least one of each of collar sizes – 250 XS, 300 Small, 400 Medium, 500 Large - available in case required.
- Size it up: After checking chart above select collar required. Or use a quick size check:
- Use your fingers to measure the vertical chin-to-shoulder distance
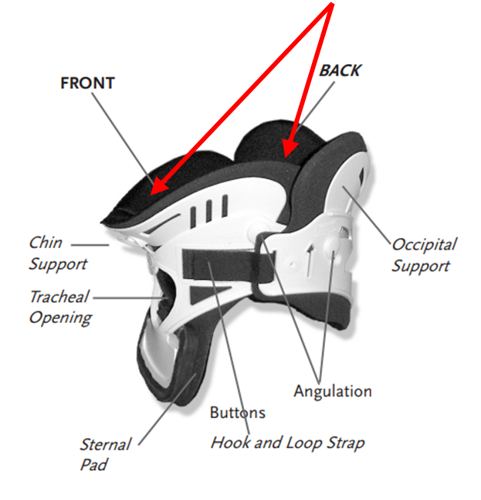
- On the collar, this measurement corresponds to the distance from top of hook & loop strap to bottom edge of collar plastic (see below)

- If deciding between two consecutive sizes, try the smaller size first.
- Use the largest size that fits comfortably and maintains correct immobilisation
NOTE: Miami-J collar Front & Backs sizes are interchangeable (i.e. fronts interchangeable with other fronts & back interchangeable with other backs). However, this is rarely necessary.
- Fully unfold the collar and identify Back and Front pieces
- Check child supine and head centrally aligned.
- Taking care not to cause movement or drag on the neck, slide the BACK of the collar behind the neck, push it down gently into the bed as you pass it through.
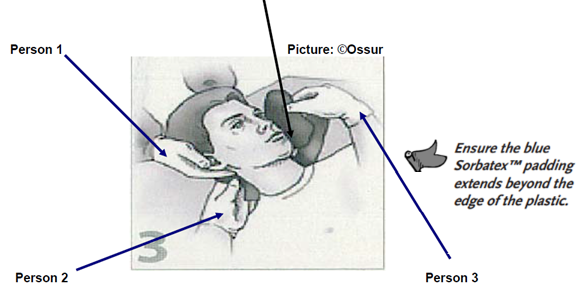
When using the Miami-J collar, you will need a third person to assist with this (see above)
- Scoop it up: Once the Back piece of the collar is in situ and symmetrical, take the Front piece of the collar with both hands. Flare the sides of the Front of the collar and slide the collar UP the chest wall. Scoop the collar up under the child’s chin until the chin is seated in the centre of the chin piece (see picture below)
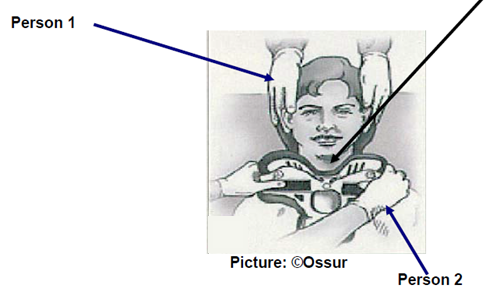
- Ensure the sides are oriented up towards the ears and off the trapezius. Note: Picture below rotated to show clearer positioning of collar. In PICU, child will be supine with manual in-line stabilisation
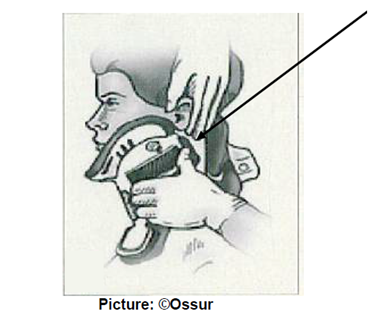
- Place Front of collar inside the Back. Apply hook & loop strap one side of collar then the other (see below)

- Snug it up: Curl the ends of the collar so that they touch the neck. Fasten the Velcro strap and ensure symmetrical alignment and oriented as “Blue-to-Blue” to Front Velcro.
- Tighten alternately to achieve an equal length on both sides
- When the child’s collar is properly fit, there should be equal amounts of excess hook & loop overhanging the Front blue adhesive sections (see image below)

Final adjustments:
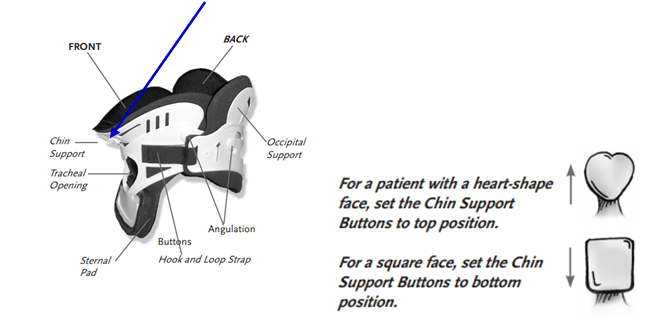
- This can be done using angulation buttons to ‘fine tune’ the fit of the collar.
- Position of buttons: 12 & 6 o’clock = unlocked……3 & 9 o’clock = locked (see below)
- These adjustments may help reduce pressure on critical points such as chin and occiput.

N.B. It is easier to adjust the Angulation buttons when Front of collar is off child
- Adjustments for chin support:
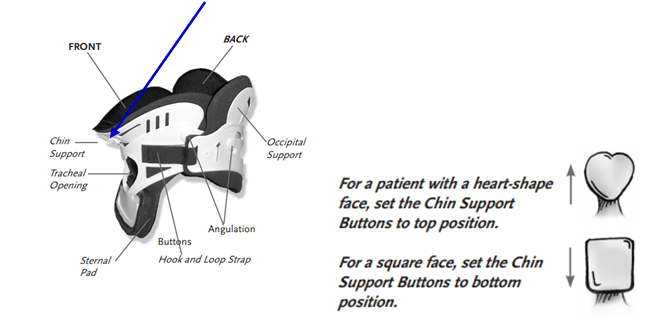
- Adjustments for occiput support:
- For supine patients keep Occipital support buttons set to TOP position (this directs top edge of collar shell to bed)
For BOTH Miami-Jr and Miami J check:
- Collar hook & loop straps are oriented ‘blue-on-blue’ with both tabs equal length
- Sides of Back overlap sides of Front
- Front of collar angled up toward ears
- Chin centred comfortably and does not extend over edge of Sorbatex™ pad OR fall back inside collar
- Plastic edge of collar should NEVER rest on child’s clavicles
- No plastic should touch child’s skin – Sorbatex™ pads should always extend beyond all plastic edges
- Tracheal opening & posterior vent should sit ‘midline’
- Collar is not too tight or fit too closely to neck. If needed, size up to next taller size.
*N.B. If you have problems with fitting your patient with any of these ‘off-the-shelf’ collars, or your patient requires ‘bespoke’ collar fitting or any other issues, you can contact Paediatric Orthotics for advice (Mon-Fri).
Orthotics department
Clinic 12 Therapies Hub
Royal Hospital for Children
0141 452 4651





 (©Ossur)
(©Ossur)