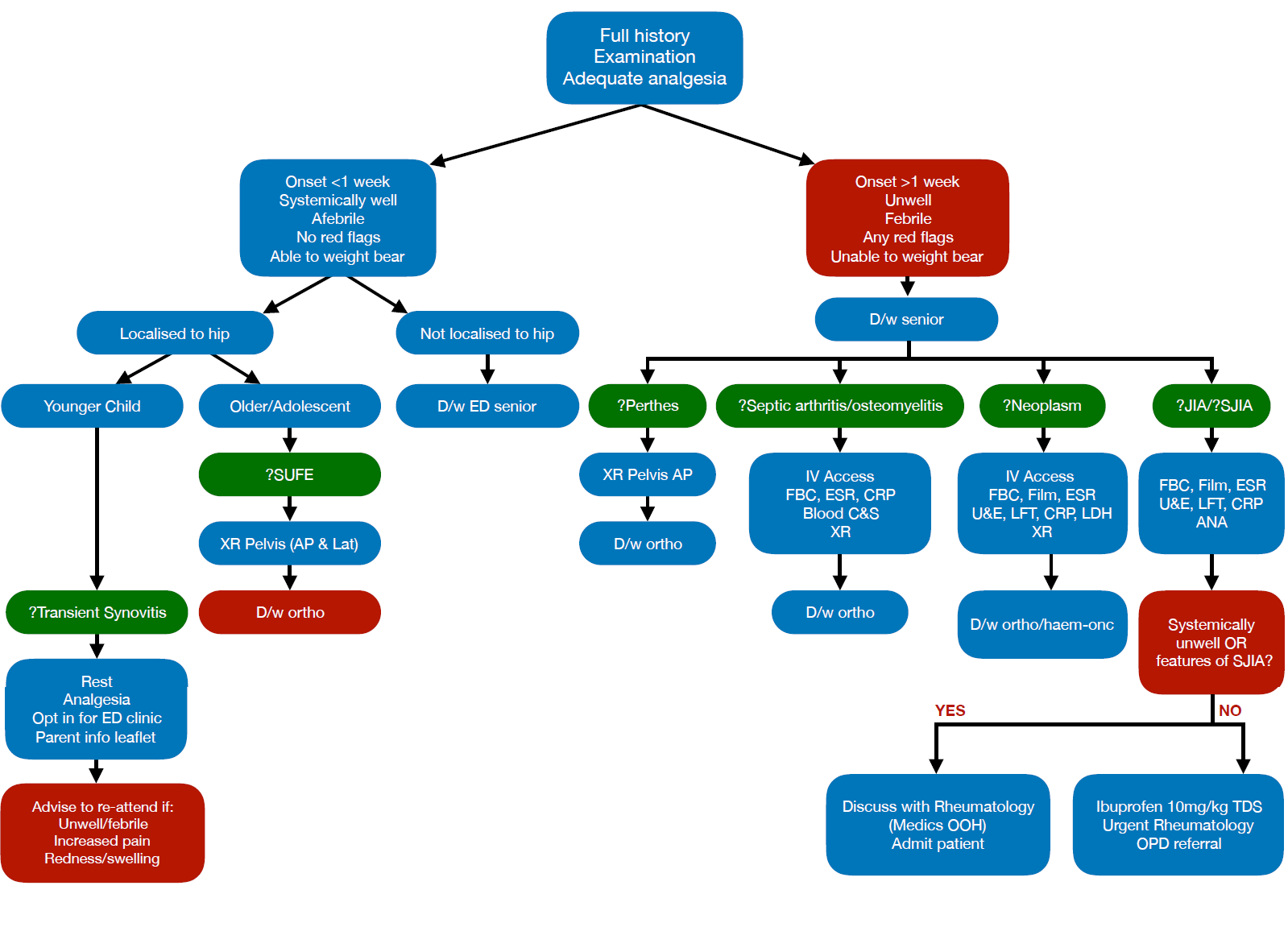
Atraumatic painful limb
Objectives
This guideline is designed to help the clinician with the initial assessment and management of the child presenting to the emergency department with an atraumatic painful limb/limp.
Background
The limping child and the child with a painful joint / limb are common presentations to the emergency department and in can be challenging to differentiate between those with potentially serious pathology and those with benign conditions.
Quick links to more information about specific diagnoses (green boxes in algorithm):
| Transient Synovitis | SUFE | Perthes | Septic Arthritis / Osteomyelitis | Neoplasm | JIA / SJIA |
Below is a list of possible differential diagnoses for a child presenting with limp / atraumatic limb pain. This list is by no means exhaustive. Some common / important diagnoses are highlighted and will be discussed in more detail.
Red flags – consider serious pathology if any present.
|
Systemic JIA (SJIA) |
Daily or twice daily spiking fever Macular rash which appears when febrile and subsequently fades. Pallor Lymphadenopathy Hepatosplenomegaly Stiff or swollen joints |
|
JIA |
Swollen and (or) restricted joint(s) Stiffness. Often worse in morning Duration approaching or exceeding 6 weeks |
|
Septic arthritis / Osteomyelitis |
Fever Systemic upset Acute severe pain / unable to weight bear Erythema or hot joint Pseudoparalysis Joint/bony tenderness |
|
Neoplasm |
Pallor Weight loss Lethargy Nocturnal pain Back pain Behaviour changes Night sweats Bruising Hepatosplenomegaly Lymphadenopathy. |
Differential diagnosis summary
|
Orthopaedic |
|
|
Infection |
|
|
Haematology / Oncology |
|
|
Rheumatological |
|
|
Other |
|
All children should have a full history and examination, full set of observations and weight. Give adequate analgesia early.
Full History:
- Consider the age of the child as this will affect your differential.
- SOCRATES for full history of pain (site, onset, character, radiation, associated symptoms, timing, exacerbating/relieving factors, severity, does it wake patient during the night)
- Be aware of referred pain - limping may due to pain referred from somewhere else (groin, abdomen, spine) and hip pain may be referred to the knee or thigh.
- Preceding illness
- History of trauma (interpret with caution as this can be coincidental or may exacerbate a chronic problem).
- Systemic symptoms - fever (duration and pattern), rash, weight loss, night sweats, bruising / bleeding, joint swelling/stiffness.
- Past medical history
- Family history – arthritis / psoriasis / IBD / other autoimmune disease
- Development - milestones - age patient started walking if applicable
- Consider NAI - (previous ED attendances, social work involvement, notifications of concern)
Examination:
General:
- Presence of fever
- Pallor
- Lymphadenopathy
- Rash (HSP / SJIA / leukaemia)
- Bruising
Musculoskeletal
- Observe child - ?pseudoparalysis of affected limb (completely stopped using limb) / refusal to weight bear
- If pain reported in a particular joint - always perform a full musculoskeletal examination.
- Gait – walking / running (or crawling if appropriate). Running often accentuates pathological features.
- Joints – inspection / palpation / movement. Look for swelling / erythema / heat / restricted movement. Comparison between affected limb and opposite side. Particular attention to hip rotation as mild restriction of movement may be seen here when other movements are normal.
- Examine all joints if swelling identified in one.
- Spine - any deformity or tenderness?
- Leg length - assess for discrepancy.
- Muscle weakness / wasting
- Neurological examination of affected limb (bilateral)
Abdomen
- Masses / organomegaly
- Boys - testicular examination
ENT examination - ?URTI / pharyngitis / acute otitis media
1.Transient Synovitis (Irritable Hip)
This is a common problem in the pre-school age group but can also affect older children. It usually affects the hip and is more common in boys than in girls. It is preceded by a viral illness in approximately 50% of cases. Transient synovitis will self resolve within 7-14 days. Children are otherwise well and afebrile.
|
|
History |
Examination |
|
Transient Synovitis |
|
|
Investigation:
If no red flags are present no imaging or other investigations are indicated at this point.
Seek senior advice if unsure.
Management:
- Give letter for ED clinic opt-in letter.
- Give transient synovitis patient / parent information leaflet
- Advise regular analgesia and rest
- Strict worsening advice to re-attend if febrile / systemically unwell or worsening pain.
2.Septic Arthritis/Osteomyelitis
Septic arthritis and osteomyelitis can present in any bone/joint but most commonly affect the lower limbs. Onset can be acute (septic arthritis) or subacute (osteomyelitis). The child is usually unwell with fever and malaise +/- evidence of joint inflammation. With osteomylitis the presenting features can be subtle, consider discussion with orthopaedic registrar if obvious bony tenderness. Erythema and joint warmth are often not obvious. Pain is usually severe and children will often hold the affected limb in a flexed position or completely stop using the limb (pseudoparalysis). Presentation can be subtle in young children. Spinal tenderness can indicate discitis. Have a high index of suspicion in immunocompromised children. Early involvement of paediatric orthopaedics team is crucial as joint destruction can occur within 24 hours. Be aware that x-ray changes are a late sign so do not be reassured by normal x-rays.
|
|
History |
Examination |
|
Septic Arthritis / Osteomyelitis |
|
|
Investigation:
- IV access
- Blood cultures
- CRP
- ESR
- FBC
- Imaging of affected joint/bone
Management
- Discuss with senior
- Urgent referral to orthopaedic team
- Do not start antibiotics prior to discussion with orthopaedic team and taking blood cultures as joint aspiration may be indicated.
- Analgesia
- Elevate and immobilise limb
Case courtesy of A.Prof Frank Gaillard, Radiopaedia.org. From the case rID: 7980
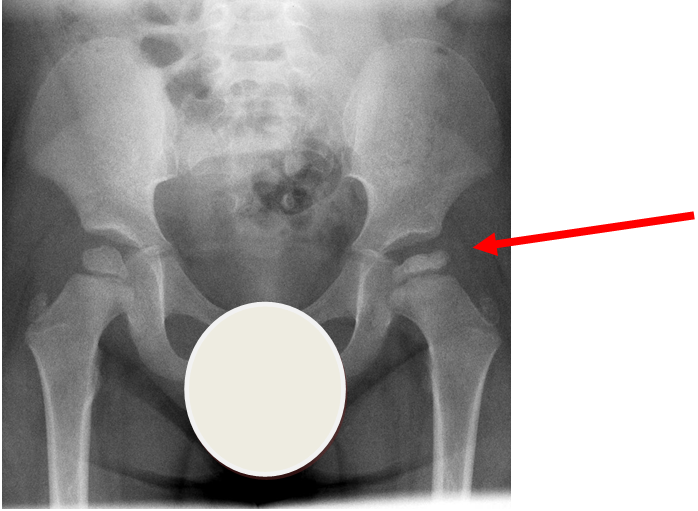
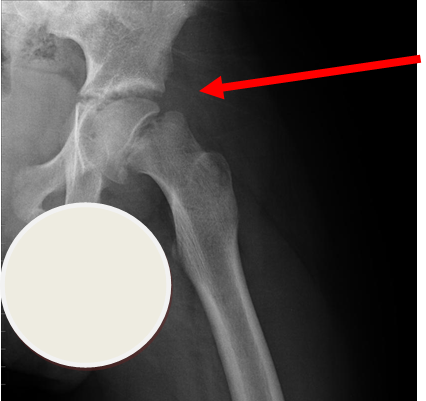
Perthes disease or avascular necrosis of the capital femoral epiphysis is more common in boys than girls (approximately 4:1). Onset is usually over weeks and typically between the ages of 3-9 years old. 15% are bilateral. X-ray of the pelvis shows flattening of the femoral head with joint space widening. X-ray changes may be absent in early disease.
The child is systemically well with no other joint involvement and no evidence of joint inflammation.
|
|
History |
Examination |
|
Perthes disease |
● Onset over weeks ● Mild hip/groin pain ● Referred pain to knee/thigh ● Systemically well |
● Limp ● Limitation of hip rotation ● Systemically well ● Afebrile ● Nil evidence of inflammation ● No other joint involvement |
Investigation
- X-ray - AP pelvis
Management
- Analgesia
- Discuss with orthopaedic team
4.Slipped Upper Femoral Epiphysis (SUFE)
Subtle left sided SUFE.
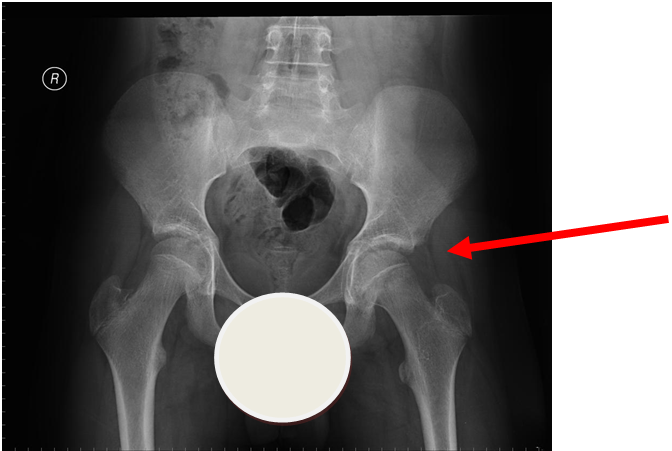
Case courtesy of Dr Gagandeep Singh, Radiopaedia.org. From the case rID: 7688
More obvious left sided SUFE (AP)
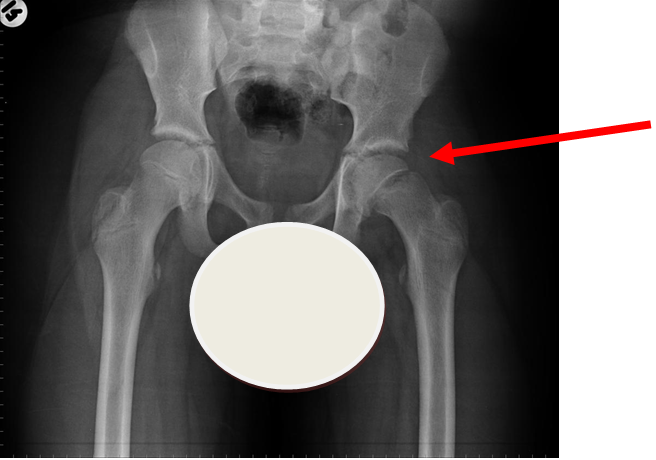
Case courtesy of Dr Gagandeep Singh, Radiopaedia.org. From the case rID: 7228
Lateral view of same patient as above
Case courtesy of Dr Gagandeep Singh, Radiopaedia.org. From the case rID: 7228
Usually occurs in late childhood / adolescence and is more common in boys than girls (2:1). It also presents more commonly in children whose weight is above the 90th centile. Bilateral in 25% of cases. Onset can be acute or subacute (ie children may present with >1day h/o pain or limp). Children may walk with an antalgic gait out-toeing, with shortening of the affected limb. If the slip is acute, the child may be unable to walk. Diagnosis is made radiologically and frog-lateral views are required as it may be missed on AP views. Urgent orthopaedic opinion is required. Unstable slips can lead to avascular necrosis of the femoral head.
|
|
History |
Examination |
|
SUFE |
|
|
Investigation
- X-ray - AP pelvis with frog lateral view (must be discussed with ortho 1st on call / ED consultant if child <8 years old)
Management
- Analgesia
- Discuss with orthopaedic team
Be aware that leukaemia or neoplasm may present with limp/limb pain.
|
|
History |
Examination |
|
Malignancy / leukaemia |
|
|
Investigation
- Early discussion with senior ED clinician if malignancy suspected
- X-ray of affected joint/limb
- Bloods - FBC and film, CRP, ESR, U&Es, LFTs, LDH. (MAS order set if SJIA suspected)
Management
- Involve orthopaedic or haematology / oncology team as appropriate.
- analgesia
See JIA guideline
Systemic JIA
If SJIA suspected discuss with oncall rheumatology team (in hours) or ED senior (out of hours) to determine whether child can go home with urgent rheumatology review the next working day or require admission.
Always consider NAI as a cause of limb pain / limp. Discuss with senior clinician if you suspect NAI and review clinical portal for other ED presentations or notifications of concern/shared referrals.
See Child Protection Guidelines (NOTE: Staffnet link - only accessible from pcs or devices connected to the GGC network).
- American College of Radiology (2013). ACR appropriateness criteria: Limping child age 0-5 years. Available at https://acsearch.acr.org/docs/69361/Narrative/ Accessed 19/6/18.
- Clinical Practice Guidelines: The limping or non-weight bearing child. The Royal Hospital for Children, Melbourne. December 2012.
- Foster H et al. Assessment of gait disorders in children. (2017) BMJ Best Practice . Retrieved from http://bestpractice.bmj.com
- Davis T, et al, 2017. Walking in circles: The limping child. Emergency Medicine Australasia, 29(4), pp. 380-382.
- Raam, R., et al, 2016. Limping Child? Think LIMPSS. Annals of Emergency Medicine, 67(2), pp. 297-300
- Singhal R et al. The use of CRP within a clinical prediction algorithm for the differentiation of septic arthritis and transient synovitis in children. Journal of Bone and Joint Surgery. British version. 2011 Nov;93(11):1556-61
- Ryan, D.D., 2016. Differentiating Transient Synovitis of the Hip from More Urgent Conditions. Pediatric annals, 45(6), pp. E209-13.
- Naranje, S., et al, 2015. A Systematic Approach to the Evaluation of a Limping Child. American Family Physician, 92(10), pp. 908-916.
- Plumb, J., et al, 2015. The role of ultrasound in the emergency department evaluation of the acutely painful pediatric hip. Pediatric emergency care, 31(1), pp. 54-58
- McCanny, P.J., et al, 2013. Implementation of an evidence based guideline reduces blood tests and length of stay for the limping child in a paediatric emergency department. Emergency Medicine Journal, 30(1), pp. 19-23.
- Caird M et al. 2006. Factors Distinguishing Septic Arthritis from Transient Synovitis of the Hip in Children. A prospective study. Journal of bone and Joint Surgery. American volume. 2006 Jun;88(6):1251-7.
- Kocher, Mandiga et al: Validation of a Clinical Prediction Rule for the Differentiation Between Septic Arthritis and Transient Synovitis of the Hip in Children. Journal of bone and joint surgery. American Volume (2004); 86-A (8): 1629-35
- Kocher MS, Zurakowski D, Kasser JR Differentiating between septic arthritis and transient synovitis of the hip in children: an evidence-based clinical prediction algorithm Journal of Bone and Joint Surgery. American Volume. 1999 Dec;81(12):1662-70.
Last reviewed: 16 September 2019
Next review: 31 October 2025
Author(s): Dr Catherine Fiddes (Paediatric Medicine trainee, RHCG)
Version: 1
Co-Author(s): Stakeholders consulted: Miss Alexandra Smith (Consultant in Paediatric Orthopaedics, RHCG), Dr Neil Martin (Consultant in Paediatric Rheumatology, RHCG). Correspondence author: Dr Steve Foster (Consultant in Paediatric Emergency Medicine, RHCG)
Approved By: Paediatric Emergency Department Guidelines Group