Buckle fracture
exp date isn't null, but text field is
November 2023: This guidance is currently under review as it has gone beyond the standard review date. It reflects best practice at the time of authorship / last review and remains safe for use. If there are any concerns regarding the content then please consult with senior clinical staff to confirm.
Definition:
Incomplete compression fracture at the metaphysis of the distal radius, ulna or both in which one cortex is disrupted, and the other remains intact.1
Buckle fractures are common injuries sustained by children >2 years old2, typically following a fall on the outstretched hand.
As the developing bone is relatively soft, the trabeculae is compressed, resulting in the appearance of a bulge. This is most frequently seen on the dorsal aspect of the distal radius but can appear on distal ulna or both distal ulna and radius. The bulge may be seen at both the ulnar and radial aspects of the bone.
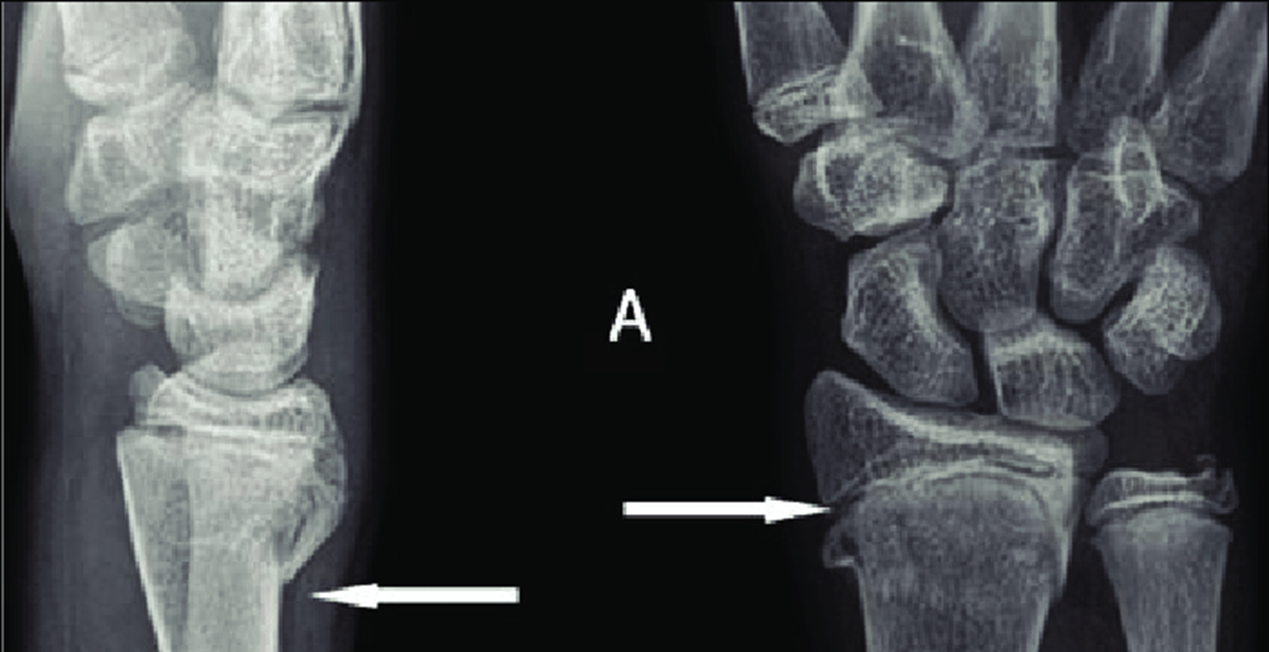
Example xray of distal radius buckle fracture:
Case courtesy of Dr Maulik S Patel, Radiopaedia.org. From the case rID: 10733
|
Pitfalls: Be careful not to misdiagnose Salter Harris II or Greenstick fractures as a simple Buckle fracture, as these can be unstable3 requiring immobilisation with cast, and orthopaedic follow up.
|
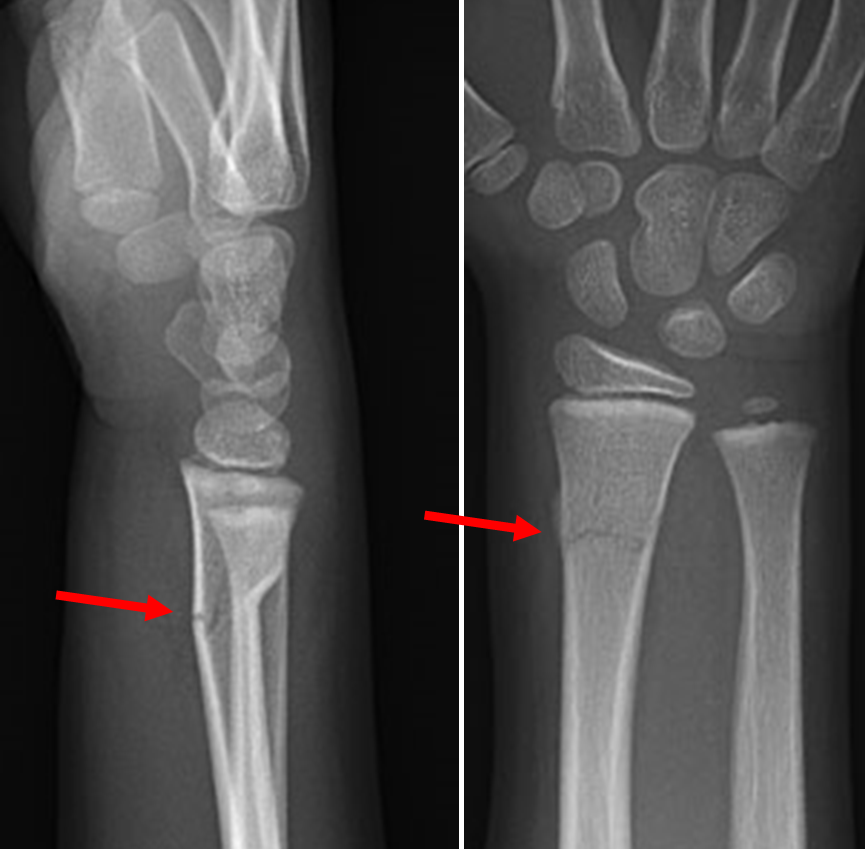
Example xray of Salter Harris type 2 fracture of distal radius:
Imaging Findings of the Distal Radio-Ulnar Joint in Trauma - Scientific Figure on ResearchGate.
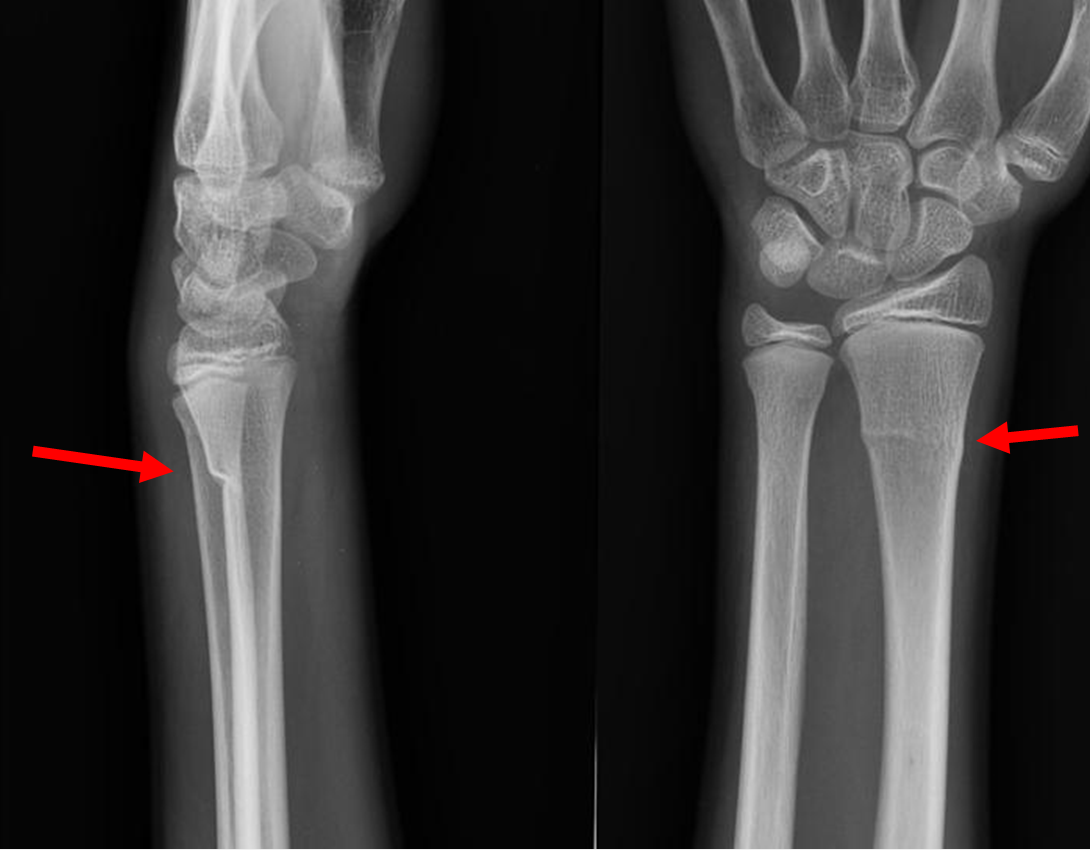
Example xray of greenstick fracture of distal radius:
(demonstrating extension of fracture line to volar cortex with angulation of the volar cortex)
Images from:
Royal Children's Hospital Melbourne - Complete fracture with buckle distal-radius lateral & Royal Children's Hospital Melbourne - Complete fracture with buckle distal-radius AP
Management:
Buckle fractures have excellent cosmetic and functional prognosis. A rigid cast is not recommended4, instead a removable splint should be applied. This has been shown to be at least as effective as a cast in terms of facilitating healing, but can promote earlier functional recovery.
Splint can be used if there is a buckle seen on both radius and ulna.
These patients can be discharged with a parent information leaflet and no planned follow up.5,6,7,8,9
Advice to Parents:
The splint should be worn for 3 weeks, but can be removed for bathing, showering and for sleep.
The child should receive regular simple analgesia for the first few days following injury. They will usually be fine to attend school after the first day.
If the child remains in significant distress despite the splint and regular analgesia, they should return to ED for review.
If after 3 weeks the wrist still seems very sore, swollen, or the child is not willing to use it, please contact the ED secretary on 0141 452 4603 where follow up arrangements will be made.
Once the splint is removed the children should avoid contact sports or high energy activities (such as rough and tumble play) for a further 3 weeks to avoid further injury
Parents should be provided with an information leaflet containing the above information.
- BMC Musculoskeletal Discord 2012 Jan 23;13(1):6
- Clin Orthop Rel Res 2005 Mar;(432):8
- RANDSBORG, P. and SIVERTSEN, E.A., 2008. Distal radius fractures in children: substantial difference in stability between buckle and greenstick fractures. Acta Orthopaedica, 80(5), pp. 585-589
- Fractures (non-complex) assessment and management (NG58). February 2017 (p7 1.3 Management in the emergency department: management of torus fractures).
- Howes, M. (2008). Splinting of buckle fractures of the distal radius in children. BestBets.
- J Bone Joint Surg Br 2001 Nov;83(8):1173
- Paediatrics 2006 Mar;117(3):691
- Paediatric Energency Carr 2016 Nov;32(11):773
- WILLIAMS, B.A. et al, 2018. Buckling down on torus fractures: has evolving evidence affected practice? Journal of Children’s Orthopaedics, 12(2), pp. 123-128
Last reviewed: 16 September 2019
Next review: 31 October 2024
Author(s): Dr Diane O’Carroll (Emergency Medicine Trainee – West of Scotland); Miss Alexandra Smith (Consultant Paediatric Orthopaedic Surgeon, RHCG)
Co-Author(s): Correspondence to Dr Steve Foster (Consultant in Paediatric Emergency Medicine, RHCG)