Head injury guideline (Emergency Department)
Objectives
Clear guidance on the assessment and management of children that have sustained an acute head injury. This guideline is based on the NICE guideline Head Injury: assessment and early management ( CG176 -2019) with some adaptations for local use.
For the purpose of this guideline “acute” is defined as within the last 24 hours.
Scope
This guideline is to be used in children under 16 years who have suffered an acute head injury.
Audience
Emergency Department medical and nursing staff
Head injuries are common in children in all of ages. NICE Head Injury: assessment and early management (CG176) defines a head injury as any trauma to the head other than superficial injuries to the face. Emergency Departments see a large number of patients with minor or mild head injuries and need to identify the very small number who will go on to have serious acute intracranial complications.
Patients presenting to ED with impaired consciousness (GCS <15) should be assessed immediately by a trained member of staff.
Any patient <1 yr presenting with a head injury should not be triaged to the Minor Injuries stream /Triage category 0.
Patients representing to ED after being discharged with a head injury should be Triage category 3 or above and be seen by the most senior doctor available.
Patients transferred from other hospital EDs should be Triage category 3 or above and be seen by the most senior doctor available.
All patients presenting with a head injury should have a full set of observations and PEWS score at some point in their ED journey.
History
It is important to gain as much information as possible regarding the nature of the incident which should include:
- Time of the incident
- Details of the mechanism of injury *
- Witnessed loss of consciousness and duration
- Discrete episodes of vomiting
- Assess any amnesia (antegrade or retrograde) and duration. Assessment is not possible in preverbal children and unlikely to be possible before the age of 5 years
- Headache
- Seizures since the injury
- Altered behaviour since the injury
- Ingestion of alcohol or drugs
- Other injuries
- Clinical course prior to consultation – improving/stable/deterioration
*Examples of Dangerous Mechanism of Injury include:
- High speed road traffic accident as a pedestrian or vehicle occupant
- Bicycle collision (high speed)
- Fall from height greater than 3 metres
- Accident involving motorised recreational vehicle (e.g. quad bike)
- High speed injury from a projectile or other object (e.g. golf club)
Clinical Examination
For any head injury patient in resus, brought by ambulance or Triage category 1 or 2, perform an immediate primary survey and ensure that the child’s airway, cervical spine, breathing and circulation are secure. As part of the primary survey perform an AVPU score and assess the pupils.
The AVPU scale is used for the rapid assessment of neurological status during the primary survey.
AVPU Scale and pupils
|
AVPU Scale |
||
|---|---|---|
|
A |
Alert |
|
|
V |
Responds to Voice |
|
|
P |
Responds to Pain |
|
|
U |
Unresponsive |
|
Any patient with a head injury requires a formal GCS [see below] documented with pupils examined.
Examine the head
- for any scalp bruising, laceration, swelling or tenderness. Measure the diameter of any haematoma in <1yrs.
- any signs of basal skull fracture- bruising around the eyes (panda eyes) or behind the ears (Battle’s sign), CSF leak from the nose (rhinorrhoea) or from the ears (otorrhoea)
Look in the ears as blood behind the tympanic membrane (haemotympanum) is another sign of basal skull fracture
Look in the mouth for dental trauma, soft tissue injuries
Assess for any? facial fractures
Perform a neurological examination,
- including cranial nerve function
- Motor function – examine limbs for lateralising weakness and presence of reflexes
|
Paediatric Glasgow Coma Scale Modification for young children/infants underlined |
|
|
|---|---|---|
|
Feature |
Scale Responses |
Score |
|
Eye Opening |
Spontaneous To voice To pain None |
4 3 2 1 |
|
Verbal Response |
Orientated/ Smiles, fixes, follows, words to usual ability Confused / Cries but consolable Inappropriate words/ Persistently irritable, moaning Incomprehensible words/ Agitated and inconsolable None / None |
5 4 3 2 1 |
|
Motor Response |
Obeys commands / Normal Movement Localise to pain Withdraw to pain Flexion to pain Extension to pain None |
6 5 4 3 2 1 |
|
Total |
|
|
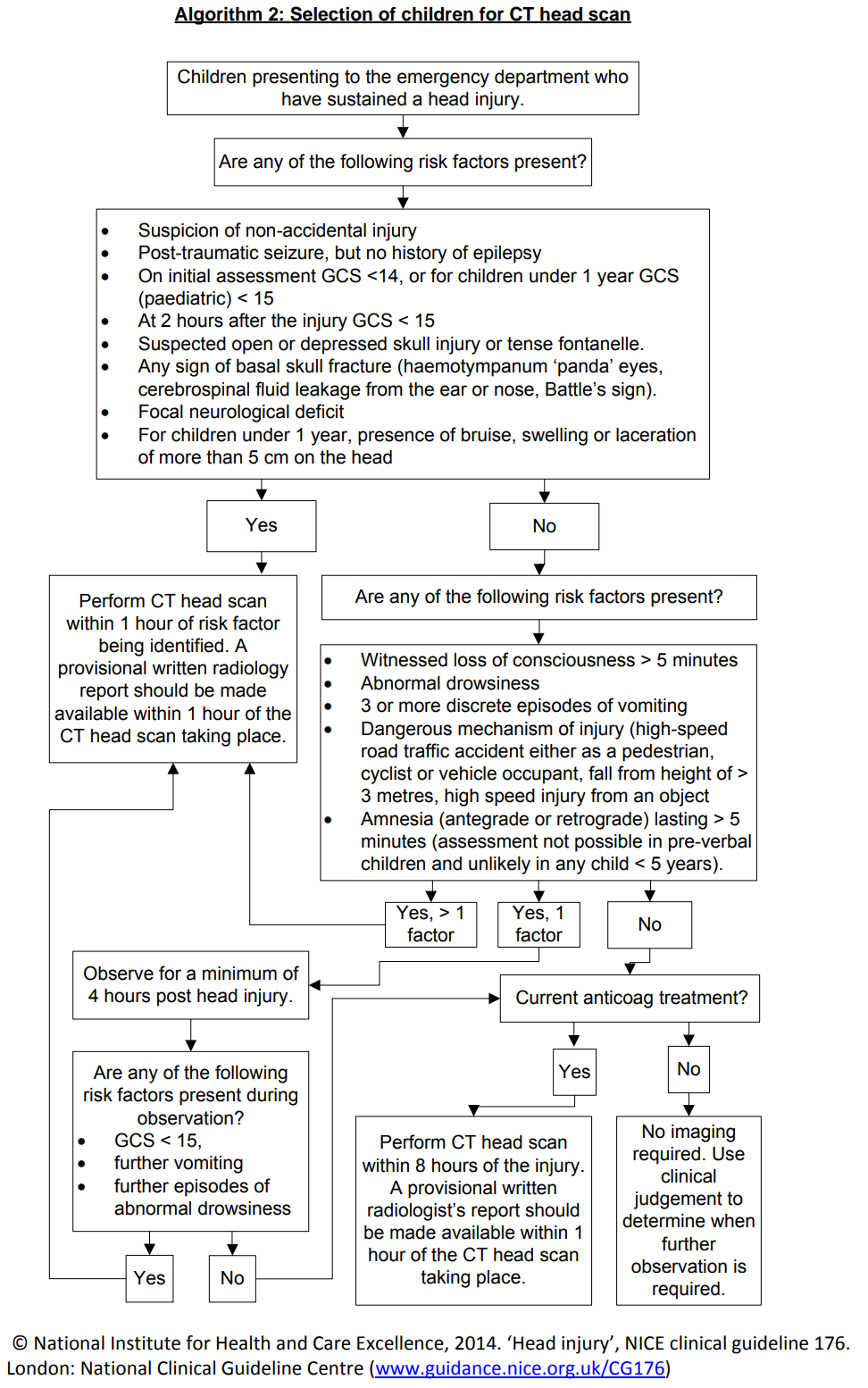
Category 1
For children who have sustained a head injury and have ANY of the following risk factors, perform a CT head scan within 1 hour:
- On initial ED assessment GCS less than 14, or children <1year GCS less than 15
- At 2 hours after the injury, GCS less than 15
- Suspected open or depressed skull fracture or tense fontanelle
- Any sign of basal skull fracture
- For children <1year, presence of bruise, swelling or laceration of more than 5cm on the head
- Post-traumatic seizure, but no history of epilepsy
- Focal neurological deficit
- Suspicion of non-accidental injury – irrespective of scan result safeguarding procedures must be followed: Child Protection pathways where concern for neglect or abuse - RHC ED
Category 2
For children who have sustained a head injury and have MORE THAN ONE of the following risk factors (and none of those in Category 1), perform a CT head scan within 1 hour of the risk factor being identified:
- Loss of consciousness lasting more than 5 minutes (witnessed)
- Abnormal drowsiness
- Three or more discrete episodes of vomiting
- Dangerous mechanism of injury*
- Amnesia (antegrade or retrograde) lasting more than 5 minutes.
|
*Examples of Dangerous Mechanism of Injury include:
|
Category 3
Children who have sustained a head injury and have ONLY 1 of the risk factors in Category 2 (and none of those in Category 1) should be observed for a minimum of 4 hours after the head injury. If during observation any of the risk factors below are identified perform a CT head scan within 1 hour.
- GCS less than 15
- Further vomiting
- A further episode of abnormal drowsiness
Category 4
Children who have sustained a head injury but have none of the risk factors above do not require imaging.
Severe Head Injury
These will be patients with significant risk factors described in Category 1 or Category 2 and may have a reduced GCS and will usually be managed in resus.
Consider the need for a Trauma Call if not already triggered.
Perform a primary survey and ensure the child’s airway, cervical spine, breathing and circulation are secure.
Prevent secondary brain injury by maintaining adequate ventilation and oxygenation.
Control any seizures.
Always consider the need for appropriate analgesia .
In conjunction with ED Consultant /PICU/ Neurosurgery consider measures to decrease intracranial pressure:
- Nurse 300 head up after correction of any shock
- Maintain adequate BP
- Aim to ventilate to a normal pCO2
- Consider IV 3% NaCl 3ml/kg as a bolus or IV Mannitol over 20minutes
Arrange an immediate CT head scan to be performed within 1 hour.
Moderate Head Injury
These patients will have some of the significant risk factors described in Category 2 or Category 3 but will not have a reduced GCS and will usually be managed in Majors.
Always consider the need for appropriate analgesia.
These children require 30 minutely neurological observations (GCS, pupils and limb power, HR, RR, BP) documented on a PEWS chart whilst in ED.
Senior advice should always be sought regarding the need for a CT head scan.
If these patients do not fulfil the criteria for a CT head scan then they should be observed in ED for a minimum of 4 hours from the time of injury before they can be discharged (see Discharge from ED section below).
These patients should be able to tolerate oral fluids in ED and be steady on their feet before discharge.
There is no clear evidence for or against the use of Ondansetron. Whilst there is no definite increase in missed pathology, there is a slight increase in the re-attendance rate in head injury patients who have had Ondansetron.
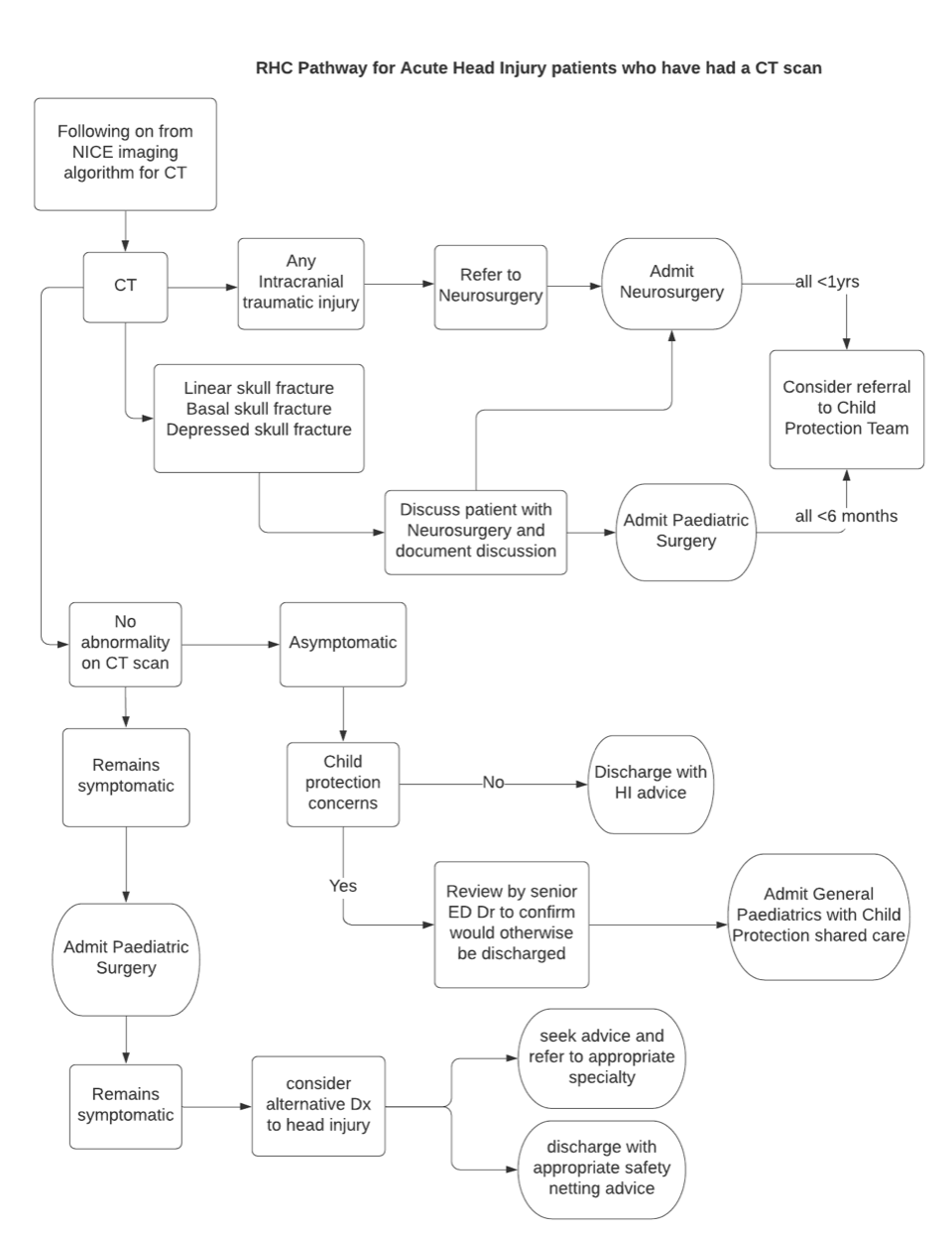
Patients who have had a CT head scan should continue to be monitored and discussed appropriately as per the Pathway for Acute Head Injury Patients who have had a CT scan (see section below)
Patients who had a dangerous mechanism of injury and other injuries in addition to their head Injury, should be referred to the Paediatric Surgical team for review and possible admission.
Mild Head Injury
Any patient with significant co-morbidities (including CSF drainage devices-“shunts”) should be discussed with the ED Consultant.
Any patient on anticoagulants or with an underlying coagulation or haematological disorder should be discussed with the ED Consultant.
Always consider the need for appropriate analgesia.
All patients being discharged from ED should have satisfactory home circumstances and be discharged with their parent/responsible carer.
Written head injury advice should be given to, and discussed with, parents/carers before a child is discharged. This should include clear instructions regarding symptoms that, if observed in their child, should prompt an immediate return to ED.
Link: Head Injury/concussion advice leaflet for parents/guardians
Consider the need for discharge analgesia.
Refer the patient to the appropriate specialty team for admission to hospital as per the Pathway.
Ensure all medical and nursing documentation is completed including a drug kardex, IV fluid prescription chart if indicated and a SBAR form.
The ED doctor should complete a “Notification of Concern” form for any child in whom there has been a child protection concern.
The ED doctor should explain to the parents that a possible child protection concern has been raised, the nature of this concern and that this requires to be investigated.
Any child protection concern should be documented clearly in the clinical notes.
Neurological observations should continue on the ward. The minimum requirement after the GCS has returned to normal is:
- 1 hourly neurological observations for the first 4 hours
- 2 hourly neurological observations for the next 8 hours
- 4 hourly observations thereafter
Admission for Patients who have not had a CT scan
There will be a small number of patients who, although they have not fulfilled the criteria for a CT head scan, have had 4hrs observation in the ED and the responsible clinician does not feel they can be safely discharged and require a prolonged period of observation. This could be because the patient lives further away, or because of significant parental anxiety, but is more likely to be because there is concern that the patient has sustained an additional associated injury e.g. after a fall down some stairs.
When an ED Consultant is present in ED, these patients should be directly reviewed by them.
When an ED Consultant is not present in ED (usually after midnight), then they should be reviewed by the ED middle grade and their management plan discussed with the ED Consultant.
The ED consultant will decide who the best specialty is to accept the patient.
This applies to any patient presenting more than 24 hours after a head injury.
These patients’ symptoms should be assessed both in relation to the head injury at the time, and the development of their symptoms following the head injury.
If the symptoms have persisted from the time of injury then an intracranial injury is more likely.
If, however, there has been a period of time from the injury where the patient has returned to normal and then develops new onset of symptoms, it is much less likely that their symptoms are related to the head injury. New onset symptoms developing more than 48-72hrs after a head injury are very unlikely to be related to an associated intracranial injury.
A full clinical examination looking for other features that may explain their symptoms, such as presence of fever, should be performed.
When an ED Consultant is present in ED, these patients should be directly reviewed by them.
If a CT head scan is required, this should be discussed with the Consultant Radiologist.
If the patient does not require a CT head scan, but requires admission to hospital for investigation of their ongoing symptoms, this should be a direct Consultant to Consultant referral to the most appropriate specialty.
When an ED Consultant is not present in ED (usually after midnight), then they should be reviewed by the ED middle grade and their management plan discussed with the ED Consultant.
Base of skull fracture:
- Check pneumococcal vaccine up to date
- Only need ENT review if involving ear canal
- If concerns, should be discussed with paediatric neurosurgical team
Closed depressed skull fracture:
- Minimally depressed skull fractures, require no operative intervention.
- Patients can be discussed with paediatric neurosurgical team.
- Do not require intervention if no intracranial injury
Open depressed skull fracture:
- If minimally depressed, often no operative intervention is required. Wounds should be cleaned and closed by ED team wherever possible.
- For significant depressed fracture / severe contamination / required theatre to close wound, discuss with paediatric neurosurgical team.
- Antibiotics for severe contamination, as per microbiological advice / guidelines
- NICE. Head injury: assessment and early management. Clinical guideline [CG176] Published date: 22 January 2014 Last updated: 13 September 2019
- Hong J, Han K, Jung J, Kim JS. Association of Exposure to Diagnostic Low-Dose Ionizing Radiation With Risk of Cancer Among Youths in South Korea. JAMA Netw Open. 2019;2(9):e1910584.
Last reviewed: 12 July 2021
Next review: 12 March 2024
Author(s): Fiona Russell
Approved By: RHC Head Injury Group: Emer Campbell (Neurosurgery), Owen Forbes (Child Protection), Greg Irwin (Radiology), Rania Kronfli (Paediatric Surgery), Mark Lilley (Major Trauma Coordinator), Allison McKie (Paediatrics), Fiona Russell (Paediatric Emergency Medicine)
Reviewer Name(s): Paediatric Clinical Effectiveness & Risk Committee