Management of the Child with a Non-Blanching Rash (NBR): (i.e. Petechiae, Purpura & Ecchymoses)
exp date isn't null, but text field is
Objectives
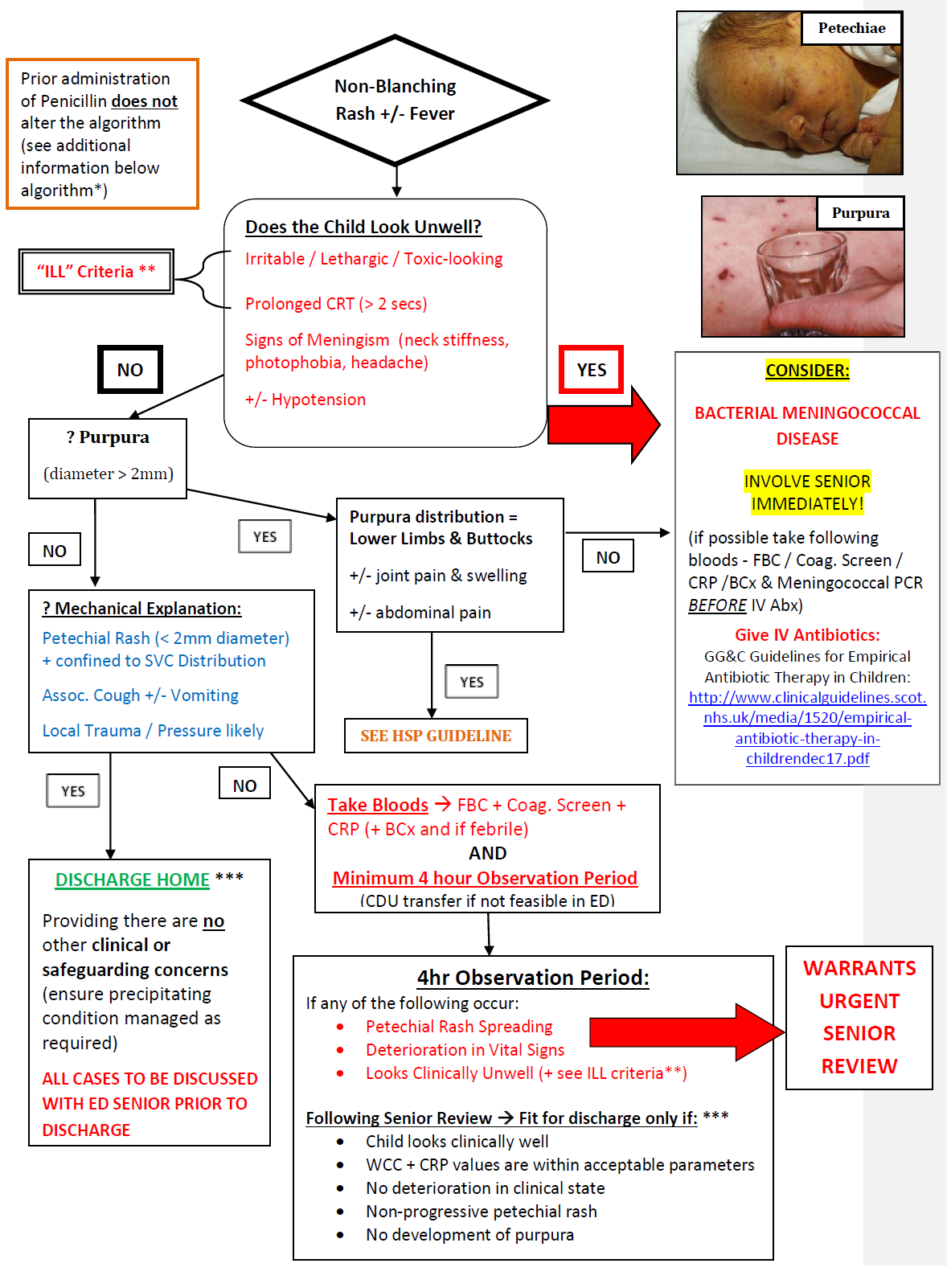
Guidance for the diagnosis and management of children presenting with a non-blanching rash. It includes a management algorithm and photos to aid the clinician.
Scope
Children presenting with a non-blanching rash.
Audience
Medical and nursing staff in the Emergency Department and Acute Care Environments.
November 2023: This guidance is currently under review as it has gone beyond the standard review date. It reflects best practice at the time of authorship / last review and remains safe for use. If there are any concerns regarding the content then please consult with senior clinical staff to confirm.
Management of the Child with a Non-Blanching Rash Algorithm go straight to algorithm if patient unwell.
It is not uncommon for children to present to the Emergency Department with a non-blanching rash (accounting for approx. 2% of all attendances) +/- fever and other systemic features of illness. 1, 2
The minority of children with invasive bacterial infections, such as meningococcal disease (MCD), must be distinguished from the majority of individuals presenting with a non-blanching rash secondary to a benign self-limiting illness (90% of paediatric hospital presentations with NBR do not have MCD; furthermore petechiae can be found in up to 3% of well infants). 3, 4, 5
Meningococcal disease remains the leading infectious cause of death amongst the paediatric population within both the UK and the developed world. The highest rates of invasive infection are in children < 5yrs (particularly those under 1yr of age); a second peak occurs amongst 11 – 22yr olds. Early recognition & treatment has been shown to improve outcome. 6, 7
- Petechiae: pinpoint-sized capillary haemorrhages (< 2mm in diameter)
- Purpura: essentially coalesced petechiae measuring > 2mm
- Ecchymoses: lesions of a similar appearance to purpura, but > 1cm in size (i.e. bruises) 8
If in any doubt – Treat as Meningococcal disease
Differential Diagnoses:
- Invasive Meningococcal Disease
- Sepsis with other Bacteria
- Trauma / Non-Accidental Injury
- Thrombocytopenia
- Viral Illness
- Mechanical (secondary to transient increases in vascular pressure e.g. straining, coughing or vomiting; manifestation of petechiae in the distribution of the superior vena cava – i.e. above the patient’s nipple line)
- The following groups are distinct diagnoses and often have specific signs and symptoms:
|
Once the above differentials have been excluded, this leaves us with a further group of children in whom we need to distinguish invasive meningococcal disease and other underlying bacterial sepsis from self- limiting viral illness or a traumatic / mechanical cause. The algorithm in this guideline is based on observation & investigation of these children and acts as a guide to their initial assessment and management. |
Management of the Child with a Non-Blanching Rash: 6, 7, 15, 16
|
* Children who have received pre-hospital IM / IV Benzylpenicillin:
|
|
**The “ILL” Criteria: Children should be considered unwell when they have the following features:
|
|
***ESSENTIAL PROCESS PRIOR TO DISCHARGE FROM RHC: Ensure clear & appropriate indications for return advice given to child’s parent / guardian. See this parent information leaflet for additional guidance on return advice |
|
Important Points: Indicators of meningococcal disease (or other serious bacterial infection) include:
Evidence is based on both retrospective and prospective observational studies; the salient points include:
|

Click to view larger version of image
- Most common haematological cause of a non-blanching rash
- Affected children are typically well (with an absence of fever / other signs of infection)
- Majority present between the ages of 2 – 5yrs
- 60% have a preceding viral infection
- Petechiae, purpura and bruising are often present in sites of frequent mild trauma
- Physical examination is usually otherwise unremarkable (i.e. no hepatosplenomegaly)
- Caused by destruction of circulating platelets by IgG-based platelet antibodies
- The platelet level at which petechiae appear spontaneously is usually ≤20 x 109/L
- Suspicion of ITP always necessitates taking a FBC + Blood Film (demonstrating isolated thrombocytopenia with an otherwise normal blood film appearance)
- A self-limiting disorder overall; > 80% spontaneously resolve within 6 – 8 weeks 8, 10

Click to view larger version of image
- An IgA-mediated systemic small vessel vasculitis
- Classical symmetrical distribution of palpable purpura - predominantly over the child’s buttocks, lower limbs and ankles
- Often associated with arthritis, peripheral oedema and colicky abdominal pain
- May have associated renal involvement (with haematuria +/- proteinuria)
- Diagnosis is uncommon < 2yrs of age; usually manifests between 3 – 10yrs
- Incidence peaks throughout the winter months; often preceded by an URTI
- Take blood for: FBC (platelet levels should be within normal range), Coagulation Screen, U&Es and Bone Profile (to monitor renal profile)
- Blood Pressure measurement (determine BP centile based on child’s sex, age + height)
- Urinalysis; plus send urine samples to quantify protein : creatinine ratio and for microscopy, culture & sensitivity
- Most cases have a benign course with remission occurring within ~ 6 weeks 8, 10, 11
See RHC Clinical Guidelines for further information regarding initial assessment and management
- Most common paediatric malignancy → accounts for 1/3rd of all childhood cancers
- Typically short history (manifesting over days-to-weeks)
- Consider in children with: hepatosplenomegaly, lymphadenopathy, easy bruising, petechiae (in absence of trauma), pallor, fatigue, weight loss, bone + / - joint pain etc.
- Diagnostic tests: Baseline Bloods (including: FBC, Blood Film, U&Es, Bone Profile, LFTs, LDH); CXR (to exclude mediastinal mass)
- Discuss any suspected new diagnoses with on-call consultant haematologist 9, 10
- Rarely causes petechiae or purpura
- Commonest cause of acute renal failure in Scotland
- Usually follows a diarrhoeal prodrome (often bloody)
- Most cases due to verotoxin-producing Escherchiae coli
(0157:H7 most prevalent subtype) - A triad of:
- Microangiopathic Haemolytic Anaemia
- Thrombocytopenia
- Acute Renal Failure
- Mainstay of management involves acute assessment of patient’s intravascular status with subsequent fluid resuscitation as appropriate
- Correction of electrolyte abnormalities thereafter
- Avoidance of NSAIDS e.g. Ibuprofen
- See link to HUS guideline below for preliminary tests and further management 10, 12
See RHC Clinical Guidelines for additional information
Further Considerations:
- Petechial rash may be associated with viral illnesses (of which, enterovirus & adenovirus are the most prevalent causes)
- Presentation is often with an URTI +/ - ‘flu-like symptoms or gastroenteritis
- In a study of 69 children with a petechial rash in Germany: Schneider et al. (2013) found that petechial rashes restricted to an SVC distribution + a CRP value within normal parameters (quantified as < 6mg/L) did not have Invasive Meningococcal Disease 5, 8, 9, 13
Where there are concerns that a NBR may be due to non-accidental injury:
- Address safeguarding concerns & discuss with Senior Medic / Consultant
- See existing Child Protection Guideline for further details regarding appropriate management: 4, 5, 8, 14
- Wells LC, Smith JC, Weston VC, et al. The child with a non-blanching rash: how likely is meningococcal disease? Arch Dis Child 2001; 85 : 218 – 22.
- Mandl KD, Stack AM, Fleisher GR. Incidence of bacteremia in infants and children with fever and petechiae. J Pediatr 1997; 131 : 398 – 404.
- Brogan P, Raffles A. The management of fever and petechiae: making sense of rash decisions. Arch Dis Child2000; 83: 506 - 507.
- Riordan F.A. et al. Non-Blanching Rash Audit Group. Validation of two algorithms for managing children with a non-blanching rash. Archives of Disease in Childhood 2016:101(8): 709 - 713.
- Barnetson L et al. Petechial rash in children: a clinical dilemma.Emergency Nurse: The Journal Of The RCN Accident And Emergency Nursing Association 2016: 24(2): 27 - 35.
- NICE Clinical Guideline [Internet]. Bacterial meningitis and meningococcal septicaemia: management of bacterial meningitis and meningococcal septicaemia in children and young people younger than 16 years in primary and secondary care. National Institute for Health and Clinical Excellence; 2010: CG102. [updated Feb. 2015; cited 2018 March 28th 2018].
- SIGN National Clinical Guideline [Internet]. Management of invasive meningococcal disease in children and young people. Scottish Intercollegiate Guidelines Network; 2008: CG102. [cited March 28th 2018].
- May N. Don’t Be Rash: Petechiae in well kids at St. Elmyn’s [Internet]. Manchester; 2003. [cited March 28th 2018].
- Waterfield T, Dyer E.M, Lyttle M. D. Fifteen-minute consultation: the child with a non-blanching rash. Archives of Disease in Childhood - Education and Practice.
- Tasker R.C, McClure R.J, Acerini C.L, editors. Oxford handbook of paediatrics. 2nd Oxford (UK): Oxford University Press; 2013.
- Royal Hospital for Children. Clinical Guideline on: Henoch-Schonlein Purpura (HSP); renal management on presentation with. [Internet] GG&C Guidelines [updated Feb. 2017; cited March 28th 2018].
- Royal Hospital for Children. Clinical Guideline on: Haemolytic Uraemic Syndrome; investigation and management of. [Internet] GG&C Guidelines [updated Oct. 2016; cited March 28th 2018].
- Schneider H, Adams O, Weiss C et al. Clinical characteristics of children with viral single and co-infections and a petechial rash. The Pediatric Infectious Disease Journal 2013; 32 (5): 186 - 191.
- Royal Hospital for Children. Clinical Guideline on: Child Protection Protocol. [Internet] GG&C Guidelines [updated Oct. 2016; cited March 28th 2018].
- Royal Children's Hospital. Clinical Practice Guideline on: Fever and petechiae – purpura. [Internet] Melbourne, Australia. [cited March 28th 2018].
- Thomas A.E, Baird S.F, Anderson J. Purpuric and petechial rashes in children: initial assessment. [Internet] BMJ Best Practice [cited March 28th 2018].
Last reviewed: 23 November 2020
Next review: 31 October 2024
Author(s): Dr Aoife Ryan (Paediatric Medicine Trainee, RHCG)
Co-Author(s): Link clinician for general paediatrics: Dr Ruth Bland (Consultant in General Paediatrics, RHCG) on behalf of Department of Paediatrics, RHCG; Correspondence author: Dr Steve Foster (Consultant in Paediatric Emergency Medicine) on behalf of Department of Paediatric Emergency Medicine, RHCG.
Approved By: Paediatric Emergency Medicine & Acute Paediatric Medicine Clinical Governance Groups
Reviewer Name(s): Paediatric Clinical Effectiveness & Risk Committee

