Home monitoring programme for children with shunt or ductal stent dependent congenital heart disease
exp date isn't null, but text field is
Objectives
- Maximise morbidity-free survival for children with shunt and stent dependent pulmonary blood flow prior to further planned surgery, driven by reliable and regular contact with the Cardiac Nurse Specialist (CNS) team and Dietitian.
- Ensure early identification of potential complications which may require surgery or cardiac catheterisation.
- The purpose of monitoring is not to deal with emergency situations if the patient acutely deteriorates at home. The normal procedure of dialling 999 and contacting Emergency Services should be followed.
For children with duct-dependent pulmonary blood flow, palliative management may include creation of a surgical systemic-pulmonary shunt, or stenting of the arterial duct. Following either procedure, patients enter a window of high risk due to the potential for acutely obstructed pulmonary blood flow. Attention has increasingly been turned therefore to improving the early detection of shunt or duct complications, in an effort to reduce inter-stage morbidity and mortality.
The Home Monitoring Programme (HMP) was pioneered by the Children’s Hospital of Wisconsin because of a concern of high mortality between hospital discharge and the second surgical stage of management in children with Hypoplastic Left Heart Syndrome (HLHS). Implementation of the HMP was based on the hypothesis that a drop in oxygen saturation from baseline, poor weight gain or weight loss may predict the presence of serious anatomic lesions or evolving illness and prompt life-saving intervention. The introduction of this programme has been proven to reduce inter-stage mortality. This practice has been adopted in many centres with HLHS programmes in the USA, and increasingly the United Kingdom. The Royal Hospital for Children (RHC) in Glasgow introduced a HMP for children with HLHS in 2011.
At RHC, the HMP developed for children with HLHS was extended and adapted for use in all children with conditions in which pulmonary blood flow is shunt or stent-dependent. The discharge of infants with such conditions is conditional upon fulfilling the discharge criteria dictated by the HMP, including optimised medication, nutritional status and the demonstration of parental understanding and program compliance.
Principally this service will be delivered by the CNS Team and Paediatric Cardiology Dietetics, and supported where appropriate by:
- Consultant Paediatric Cardiologists/Registrars/Cardiac Advanced Nurse Practitioners.
- Ward 1E duty medical and nursing teams.
This protocol is applicable to every infant with shunt or ductal stent-dependent pulmonary blood flow.
Any patient on the HMP who turns one year of age, will ordinarily cease being on the programme unless they remain shunt or stent dependent, and to remain on the programme, the named Cardiologist will need to request this.
The HMP criteria may no longer be applicable and suitable for patients over one year of age, and so this will need to be considered.
Please see “Children who are over one year of age and no longer shunt or stent dependent” section below for further information.
- Patient suitability for commencement on the HMP is decided by the patient’s named Consultant Cardiologist, and this decision is then to be communicated with the Cardiac Nurse Specialist (CNS) Service, Cardiac Dietitian, Ward Staff and the patient’s parents.
- Patients identified to commence on the HMP should be transferred appropriately to Ward 1E for training to be facilitated; if patient not already placed in 1E.
- HMP training is carried out by a Cardiac Nurse Specialist (CNS) and supported by Ward 1E staff.
- The patient is discharged home in possession of user-friendly baby weighing scales, an oxygen saturation monitor and a HMP patient diary containing call criteria.
- Parents are trained in all aspects of the HMP including how to use the equipment provided, how to document the infants HMP data within the diary and call criteria is explained.
- The medication, feeding and home monitoring plans (with specified weight, SaO2 and feed intake parameters) are signed off prior to discharge.
- The Paediatric Cardiology Dietitian will meet with the patient’s parents prior to discharge to discuss feeding and expected growth.
- There is a clear understanding of contact numbers and who to contact:-
- Parents can contact the CNS Service Monday to Friday 8am-4pm on HMP phone 0141 451 5807.
- Outside office hours, calls are directed to Ward 1E.
- For feed/growth related questions parents are given the contact number for the Paediatric Cardiology Dietitian.
- The CNS team contacts the Scottish Ambulance Service with patient’s details to be logged as a priority call out.
- The CNS team enrols the patient on the hospital’s Patient Alert System, identifying him/her as high risk and as a potential candidate for a capillary blood gas and lactate in the event of presentation to the Emergency Department.
- Prior to discharge home, the CNS team will check if the infant’s local hospital has a Patient Alert System that can identify the child as high risk. They will request that a message is logged advising that if admitted to A&E or hospital consideration should be given to performing a capillary blood gas and lactate and that the On-call Cardiologist or Cardiology Registrar are informed immediately.
- Discharge is approved only after the parents, CNS, Dietitian and Cardiology team are satisfied HMP training is complete and all discharge criteria met.
- Parents record the patient’s weight at the same time on a Monday and Thursday before a feed.
- Parents spot check the patient’s saturation at the same time daily.
- The patient’s weight and saturation are logged in the Diary.
- Feeds volumes are documented in the Diary.
- There is at least weekly telephone contact with the CNS team and the Paediatric Cardiology Dietitian to review the diary and any concerns.
- The patient’s hydration is prioritised to assist in shunt protection.
- If a patient has a vomiting and diarrhoeal illness the CNS team, Dietetics or Medical staff should be notified.
- Notification should also be given to the CNS team of any breach in agreed parameter limits or of any concerns as soon as possible.
- The CNS team are to be notified immediately, either by a parent or health care staff, if the patient presents for medical attention of any nature.
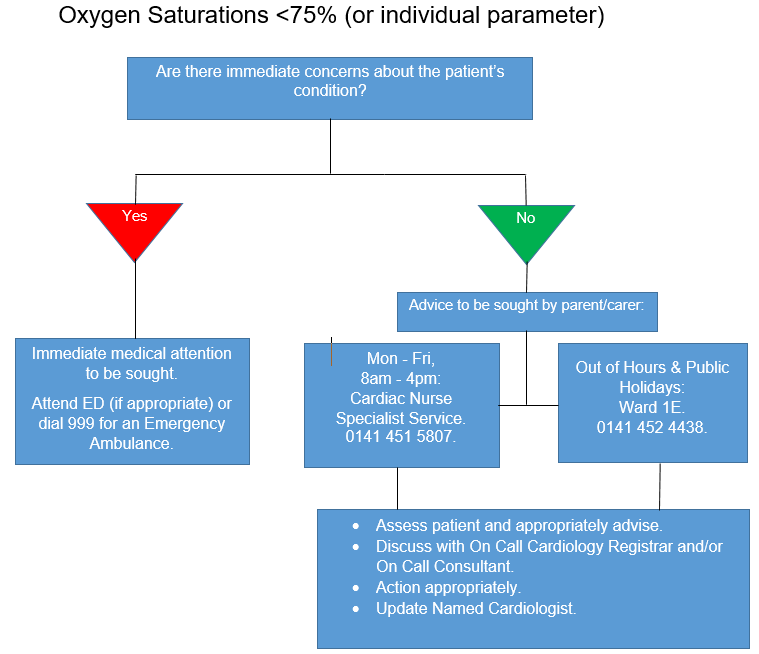
- Resting oxygen saturation drops below 75% (this may be modified following discussion with the named Cardiologist). Please see actions in Appendix A.
- Difficulty recording the infant’s oxygen saturations.
- The infant’s breathing has become laboured or otherwise unusual.
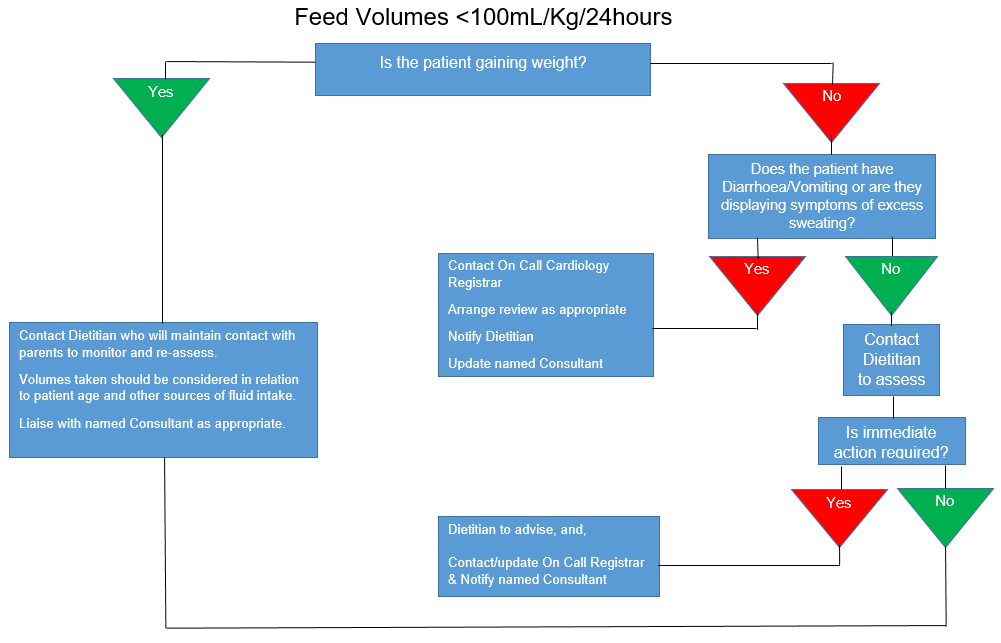
- The infant is not meeting fluid volumes advised by Dietitian (Please see actions in Appendix B - ‘Feed Volumes <100ml/kg/24hours’).
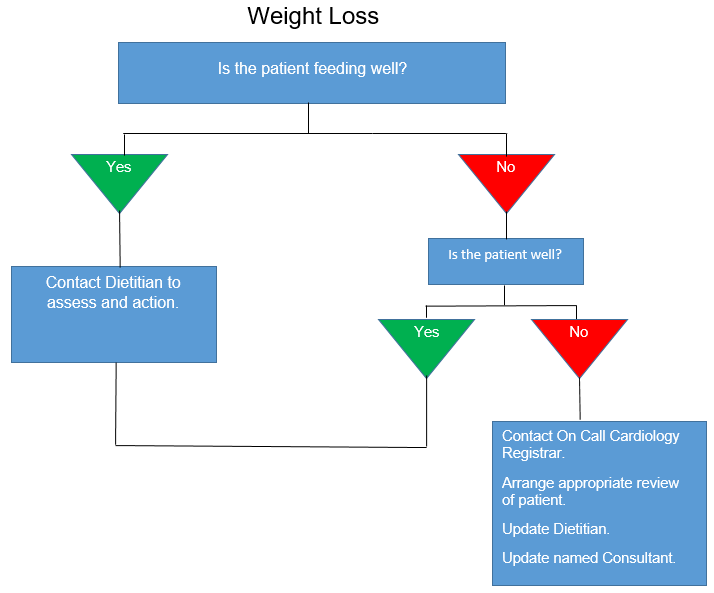
- If infant loses weight (Please see actions in Appendix C - ‘Weight Loss’).
- Any parental question or concern.
- If medical attention is sought, whether primary, secondary or tertiary level.
It must be remembered that each child will have an individually-prescribed set of normal parameters. It is critical that deviation from the norm for a particular patient be associated with a low threshold for early medical review.
In the first instance this may be at GP (if appropriate), Local Hospital, or RHC.
The Cardiologist, CNS Team and Paediatric Cardiology Dietitian are to be notified of A&E attendances immediately
- Oxygen saturation, weight and feed intake data will be documented on Heartsuite.
- A weekly summary of the patient’s data will be added to Clinical Portal.
- Feeding Data are logged on Clinical Portal within Dietitian Notes.
- All parental calls for breach of parameter limits or general questions will be documented on Heartsuite and Clinical Portal.
- All HMP patients are followed routinely in a Cardiology Clinic and are seen when possible by the Consultant and CNS during each visit.
- HMP Diary reviewed in Clinic.
- Dietetics review frequently by phone and attend clinics when possible.
CNS update the CNS team and Dietitian on a weekly basis. This includes each HMP patient’s weekly data and the highlighting of any concerns.
The HMP MDT Team meet on a monthly basis as a channel of communication surrounding the HMP patients.
As outlined in the application section of this protocol, ordinarily the programme will be discontinued in children who reach one year of age and/or who are no longer shunt or stent-dependent, as the programme may no longer be suitable and applicable.
In the instance of a child reaching one year whilst on the HMP, the named Consultant Cardiologist must review the child’s clinical status and the suitability of the programme for the child. If it is deemed to remain appropriate, it must then be requested by the Consultant that the child continues with the programme.
This decision should then be communicated between the team and documented in the child’s records. Any amendments to the programme for the child should also be communicated and clearly documented.
- Adherence to the HMP protocol will be assessed by regular review of patient data available on Heartsuite database and Clinical Portal.
- Audit of the HMP will occur regularly, including the administration of parental satisfaction questionnaires.
- The HMP protocol will be subject to formal annual review, which will be brought forward in the case of evidence to suggest earlier modification is needed.
- Any significant patient event will trigger review of the HMP as it pertains to that patient, to ensure the HMP objectives were achieved in that instance.
Azakie. T. et al (2001) Evolving strategies and improving outcomes of the modified Norwood procedure: A 10-year single institution experience. Annals of Thoracic Surgery. Vol. 72(4):1349-1353.
Bridges, N.D. et al (1990) Bidirectional cavopulmonary anastamosis as interim palliation for high-risk Fontan candidates. Circulation. Vol. 82(suppl IV):IV-170-IV-176.
Carlo WF et al. (2017) Practice trends over time in the care of infants with hypoplastic left heart syndrome: A report from the National Pediatric Cardiology Quality Improvement Collaborative. Congenital Heart Disease. Vol.12, Pages 315–321.
Crawford, R. et al (2020) A systematic review examining the clinical and health-care outcomes for congenital heart disease patients using home monitoring programmes. Journal of Telemedicine and Telecare. Vol. 0(0), Pages 1-16.
Gaynor, J.W. et al (2002) Risk factors for mortality after the Norwood procedure. European Journal of Cardio-thoracic Surgery. Vol. 22:82-89.
Giglia, T.M. et al (2019) Interstage monitoring: Yes it makes a difference! Progress in Pediatric Cardiology. Vol. 54(1), 101140.
Mahle, W.T. et al (2001) Unexpected death after reconstructive surgery for hypoplastic left heart syndrome. Annals of Thoracic Surgery. Vol. 76:61-65.
Mahle, W.T. et al (2000) Survival after reconstructive surgery for hypoplastic left heart syndrome: A 15-year experience from a single institution. Circulation. Vol. 120(suppl III): III-136-III141.
Metcalf, M.K., Rychik, J. (2020) Outcomes in Hypoplastic Left Heart Syndrome. Pediatric Clinics of North America. Vol. 67(5), Pages 945-962.
Nievesa, J., Rudd, N.A., Dobrolet, N. (2018) Home surveillance monitoring for high risk congenital heart newborns: Improving outcomes after single ventricle palliation - why, how & results. Progress in Pediatric Cardiology. Vol.48, Pages 14-25.
Rudd, N.A. et al on behalf of the American Heart Association Council on Cardiovascular and Stroke Nursing; Council on Lifelong Congenital Heart Disease and Heart Health in the Young; Council on Arteriosclerosis, Thrombosis and Vascular Biology; Council on Clinical Cardiology; and Council on Lifestyle and Cardiometabolic Health. (2020) Interstage Home Monitoring for Infants With Single Ventricle Heart Disease: Education and Management: A Scientific Statement From the American Heart Association. Journal of the American Heart Association. Vol. 9(16), e014548.
Tweddell, J.S. et al (2002) Improved survival of patients undergoing palliation of hypoplastic left heart syndrome: Lessons learned form 115 consecutive patients. Circulation. Vol. 106(12) suppl I:182-189.
Last reviewed: 22 December 2023
Next review: 30 September 2026
Author(s): Lorraine Mulholland; Dr Ben Smith; Laura Flannagan
Approved By: Scottish Paediatric Cardiac Service

