Diagnosis, treatment and management of UTI in children RHC Glasgow
exp date isn't null, but text field is
Objectives
The aim of this guideline is to produce consistent clinical practice across secondary care for infants and children with infection of the urinary tract. The guideline is based on the NICE guidelines (2018) with some adaptations for local antimicrobial use.
Scope
All patients under 16 years of age with signs or symptoms of a urinary tract infection.
Audience
The guideline is aimed for use by all clinicians at the Royal Hospital for Children (RHC) Glasgow.
Paediatric UTIs are becoming more problematic to treat due to increasing levels of antimicrobial resistance. This guideline aims to encourage the appropriate collection of urinary samples, the prescription of appropriate empiric antimicrobials and the timely chasing of urine culture results. Routine use of antibiotic prophylaxis is no longer recommended after UTIs in all ages (NICE 2018). Prophylaxis may still be considered in specific circumstances.
|
Upper tract symptoms |
Lower tract symptoms |
Features of atypical UTI |
|
Fever Lethargy Malaise Vomiting Loin pain |
Non specific abdominal pain Urgency of micturition Frequency Enuresis Frank haematuria |
Seriously unwell* Sepsis Poor urine flow Abdominal/bladder mass Failure to respond to sensitive antibiotic within 48 hours Elevated creatinine Non E.Coli, Klebsiella or enterococcus organism |
*Note ‘seriously unwell’ includes patients who have had a septic screen
* NICE. 2013. Fever in under 5s: assessment and initial management [CG160]. Paragraph 1.2.2 (last updated August 2017
Recurrent UTI:
- two or more episodes of proven UTI with upper tract symptoms within 12 months
OR
- one episode of proven UTI with upper tract symptoms plus one or more episode of UTI with lower tract symptoms within 12 months
OR
- three or more episodes of proven UTI with lower tract symptoms within 12 months.
Particularly in children < 1 yr of age, signs and symptoms of a UTI can be vague. Collecting a urine for analysis should be considered in any infant or child with a temperature >38◦C with no clear source or in the context of a non specific illness.
Table 1 Presenting symptoms and signs in infants and children with UTI (NICE 2018)
|
Age group |
Symptoms and signs Most common ------------------> Least common |
|||
|
Infants younger than 3 months |
Fever Vomiting Lethargy Irritability |
Poor feeding Failure to thrive |
Abdominal pain Jaundice Haematuria Offensive urine |
|
|
Infants and children, 3 months or older |
Preverbal |
Fever |
Abdominal pain Loin tenderness Vomiting Poor feeding |
Lethargy Irritability Haematuria Offensive urine Failure to thrive |
|
Verbal |
Frequency Dysuria |
Dysfunctional voiding Changes to continence Abdominal pain Loin tenderness |
Fever Malaise Vomiting Haematuria Offensive urine Cloudy urine |
|
A clean catch (CCU) in infants or mid stream specimen urine (MSSU) in children are the recommended methods for obtaining a urine sample. Only social cleanliness and dryness are required. If it is not possible to obtain a urine sample by these methods then it should be obtained by catheter or suprapubic aspirate (SPA). All samples for microscopy and culture should be sent in a boric acid container (red top).
Culture results provide the definitive information about the presence of a UTI and the causative organism. A positive UTI is defined as > 100 000 bacteria colony forming units/ml urine. Antibiotic therapy may be guided by sensitivities obtained during culture. Unfortunately, this information is not available at presentation and a decision on whether to initiate treatment is based on clinical symptoms, urinalysis and microscopy.
Urinalysis interpretation for all children under 16 years (NICE 2018)
|
Leucocytes |
Nitrites |
|
|
Positive |
Positive |
Treat as UTI. Send urine for culture.
|
|
Negative |
Positive |
Treat as UTI. Send urine for culture.
|
|
Positive |
Negative |
Send urine for microscopy and culture and await results. Not for antibiotics unless good clinical evidence. Caution with children under 12 months with UTI as can be nitrite negative. |
|
Negative |
Negative |
Unlikely to be UTI. Only send urine for culture if specific urinary symptoms. |
Microscopy
Microscopy will routinely be performed on all urine samples sent to microbiology for culture from children < 3 years of age. For any microbiology samples that are sent for children over 3 years of age, microscopy will have to be specifically requested if required. Indications for microscopy in this age group are if urinalysis is leucocyte positive and nitrite negative.
The other groups of patients who should automatically have urine microscopy, regardless of age, are those who are post renal transplant or are immunocompromised.
Routine microscopy at RHC will be available from 9am – 8pm. If microscopy is required urgently out with these hours then it needs to be requested specifically and the biomedical scientist will need to be contacted at home to discuss this. Urgent microscopy is indicated in infants < 3 months of age with a suspected UTI or as part of a septic screen for sepsis of unknown origin. (It should be noted that even with a positive urine microscopy, a lumbar puncture should still be performed in all infants with fever who are less than 1 month and in all infants who are unwell between 1-3 months)1.
Microscopy will report the presence of white cells and organisms as scanty, moderate or numerous. Definitions of these terms according to local RHC protocols are listed in the table below. Numerous organisms are more suggestive of a UTI than moderate or scanty but the only definitive result is culture. Microscopy can help to aid clinical decision making in the context of individual patients.
|
|
Scanty |
Moderate |
Numerous |
|
White Cells (per µl urine) |
< 40 |
40 – 100 |
>100 |
|
Organisms (per µl urine) |
<500 |
500-1000 |
>1000 |
The following risk factors for underlying pathology in the context of UTI should be considered within the history and examination
|
*VUR can be familial and increases risk of upper tract UTI
**blood pressure should be assessed according to height centiles
Paediatric Renal Unit, RHC Clinical Guideline: Hypertension in Paediatrics
Urine culture is advised for all infants, children and adolescents for whom empiric antibiotic treatment for a UTI is considered. If a child is known to nephrology or urology services or has had previous UTIs then please check previous urine culture results as this may influence empiric prescribing.
Any ESBL (Extended spectrum beta lactamase) producing organisms should be discussed with a microbiologist and/or the infectious diseases team.
Please see empirical antibiotic therapy guideline for guidance on antibiotic treatment. Please record duration of treatment on Kardex if admitted.
For those patients discharged from the Emergency Department, advise the child’s parent/carer that the child should be improving within 48 hours. If the child is not improving or is clinically worsening, then the child should re-present to the Emergency Department.
The UTI factsheet should be issued to parents and carers in all cases where UTI is suspected. Most urine cultures will be reported at 48 hrs and all effort should be made to chase these results and amend the clinical management plan accordingly. If a bacterium grows which is resistant to the prescribed antibiotic and the child remains symptomatic, then change antibiotic as per sensitivities.
The routine use of antibiotic prophylaxis after UTI is no longer recommended by NICE (2018), the American Academy of Pediatrics (2011), and the Canadian Pediatric Society (2015) due both to the lack of efficacy in preventing renal damage and the increasing prevalence of antibiotic resistance.
This guidance does not apply to patients already known to nephrology or urology services who should be discussed with these services if the question of prophylaxis arises.
In the cases of infants under 3 months with UTI, children/infants with an atypical UTI (particularly under 6 months old) or recurrent UTIs (see definitions above), prophylaxis will be discussed on an individual basis during working hours with the consultant in charge of the patient’s care.
Whether antibiotic prophylaxis is prescribed or not parents and GPs should be aware that the child may have further UTIs and that subsequent symptoms suggestive of a UTI should result in:
a) the collection of a sample of urine for microbiological testing
b) the consideration of early empiric antibiotic treatment if clinically warranted
c) the pursuit of the urine test result and rationalisation of antibiotic prescription based on that result.
Where antibiotic prophylaxis is prescribed the risks/benefits should be discussed with parents and should be reviewed after 3-6 months with a view to stopping. In some cases the renal or urology team may consider cycling of prophylaxis after discussion with microbiology and/or infectious diseases.
Where antibiotic prophylaxis is prescribed, trimethoprim is the first line choice antibiotic. The use of broad spectrum antibiotics e.g. co-amoxiclav or cefalexin should be avoided or used for a short period only in select cases. If a child’s UTI is trimethoprim resistant, then consideration should be given to adopting an early empiric management approach. If prophylaxis is considered essential, then a risk/benefit discussion should happen with microbiology and/or infectious diseases. Liquid nitrofurantoin is currently £460 per bottle and its use as prophylaxis should be in exceptional cases only. (As previously mentioned, it is also contraindicated in infants < 3 months).
All male infants < 3 months of age who have a UTI should have an USS, an MCUG and a DMSA. Female infants < 3 months will all require an USS but will only require an MCUG and DMSA if they in the atypical UTI category (See UTI definitions). A febrile infant of < 3 months will often be considered to be seriously unwell and therefore in the atypical UTI category – for example, if they have had a septic screen. (NICE 2013. Fever in under 5s assessment and initial management [CG160]. Paragraph 1.2.2 ).
For infants < 6 months (Edited from NICE 2018)
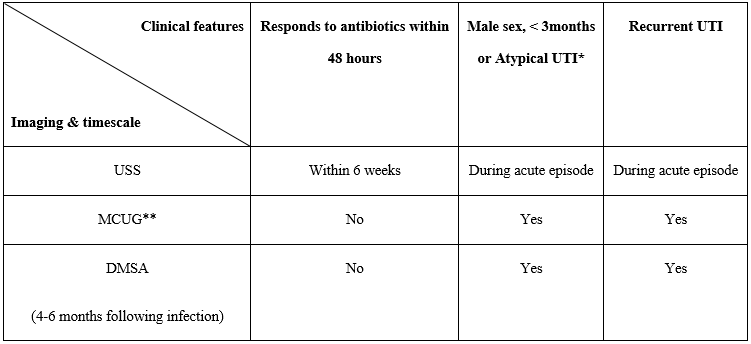
* If the only feature of atypical UTI is infection with a NON E.coli, Enterococcus or Klebsiella organism UTI, and infant is responding well to antibiotics and with no other features of atypical infection, USS can be performed within 6 weeks.
**When an MCUG is requested, it is the requestor’s responsibility to organise antibiotic cover (prophylactic dose) for 5 days with the MCUG occurring on day 3. In patients who are already on prophylaxis, they should receive treatment dose antibiotics for 3 days with the MCUG occurring on day 2.
If any infant has an abnormal USS, particularly if an obstructive uropathy is suspected, they should be discussed with the renal/urology team regarding timing of further imaging and ongoing management.
Imaging 6 months to 3 years (NICE 2018)
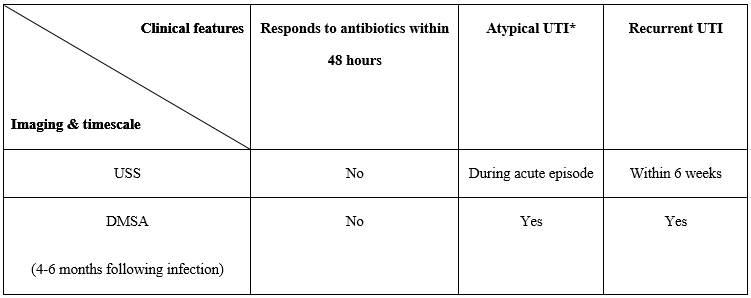
* In an infant or child with a non E.coli, Enterococcus or Klebsiella organism UTI, who is responding well to antibiotics and with no other features of atypical infection, USS can be performed within 6 weeks.
MCUG is not routinely indicated in this age group but may be considered if there is dilatation on USS, poor urinary flow, atypical causative organism or family history of vesicoureteric reflux (VUR). In the continent child, a MAG 3 is an alternative study to give information about reflux and drainage.
Children ≥ 3 years (NICE 2018)
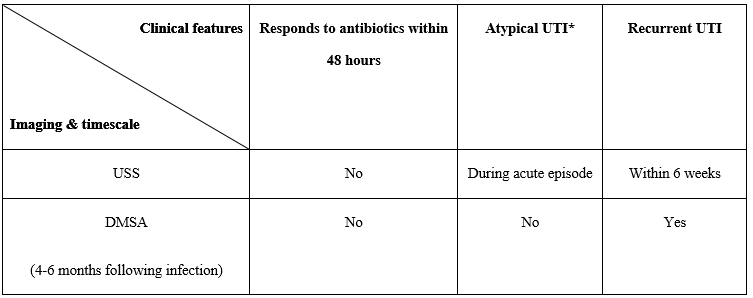
* In an infant or child with a non E.coli, Enterococcus or Klebsiella organism UTI, who is responding well to antibiotics and with no other features of atypical infection, USS can be performed within 6 weeks.
As with the 6 months – 3 year age group, if USS suggests dilatation, further discussion with renal/urology is recommended for consideration of further imaging to give information on reflux and drainage.
For information about imaging tests parents can be directed to www.infokid.org.uk
Positive urine culture noted. ED consultant will review the case and:
- Ensure an appropriate antibiotic has been prescribed / check culture sensitivities – contact parent / GP to arrange prescription if action required.
- If patient <3 months of age then refer to acute paediatric team to arrange clinical review in CDU.
- Any ESBL producing organisms should be discussed with microbiology and/or the infectious diseases team.
- Assess if follow up imaging is required:
- If recurrent UTI in <6month old or atypical organism in all ages the the patient should be discussed with general medical team for consideration of assessment +/- imaging.
- All other children requiring follow up imaging (USS / MCUG / DMSA) will be referred to UTI service using ‘Out-patient UTI Service Referral proforma’. Imaging will be arranged by UTI service team.
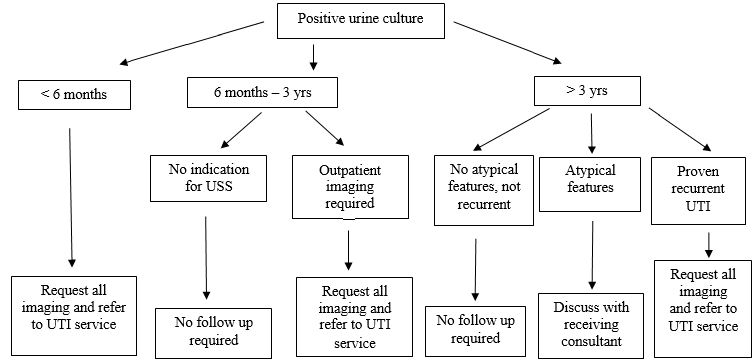
Any infant or child who has had imaging requested as an outpatient requires outpatient clinic follow up. This will include all infants under 6 months, children under 3 years with atypical features and any children who have had recurrent UTIs. At times it may be difficult to establish if a child fits the definition of proven recurrent UTIs. If there is any ambiguity, these patients should be discussed with the receiving general paediatric consultant prior to requesting imaging and referral. Prophylaxis for proven recurrent UTIs in patients who do not require admission should be discussed in outpatient clinic and not commenced in the acute setting. Follow up for children over 3 years who have had an atypical UTI but with a normal USS during the acute episode and no further imaging is required, should also be discussed with their general paediatric consultant.
For all patients in Greater Glasgow and Clyde, follow up is with the UTI service in RHC Glasgow. Referral to the UTI clinic is made by completing a UTI referral proforma which should be given to the ward clerk at the time of discharge. Please ensure that as much detail as possible is put onto the form, including a patient label.
- 2013. Fever in under 5s: assessment and initial management [CG160]. (last updated August 2017)
- Antibiotic management/Empirical antibiotic treatment – taken from guidelines by Ysobel Gourlay (Antimicrobial utilisation committee, November 2017)
- Prophylaxis of paediatric urinary tract infections guidance. Ysobel Gourlay (Antimicrobial utilisation committee, November 2017)
- 2018. Urinary tract infection (lower): antimicrobial prescribing [NG109].
- 2018. Pyelonephritis (acute): antimicrobial prescribing [NG111].
- 2018. Urinary tract infection (recurrent): antimicrobial prescribing [NG112].
- 2007. Urinary tract infection in under 16s: diagnosis and management [CG54] (last updated October 2018)
- American Academy of Pediatrics. 2011 (reaffirmed 2016). The diagnosis and management of the initial urinary tract infection in febrile infants and young children 2–24 months of age. Pediatrics, 138(6).
- American College of Radiology. 2016. ACR appropriateness criteria: urinary tract infection, child.
- Canadian Paediatric Society. 2014 (reaffirmed 2017). Urinary tract infection in infants and children: diagnosis and management. Paediatr Child Health, 19(6):315-19.
Last reviewed: 01 August 2022
Next review: 31 May 2026
Author(s): Primary author – Dr Sheena Logan (ST8 in Paediatric Medicine, RHCG); Correspondence author – Dr Steve Foster (Consultant in Paediatric Emergency Medicine, RHCG)
Co-Author(s): Co-authors/stake holders – Dr Ruth Allen (Consultant in Paediatric Radiology), Dr Ruth Bland (Consultant in General Paediatrics, RHCG), Dr Conor Doherty (Consultant in paediatric infectious diseases and immunology, RHCG), Ms Ysobel Gourlay (Lead Antimicrobial Pharmacist, North Sector, GG&C), Ms Susan Kafka (Specialist Pharmacist, RHCG), Dr Ian Ramage (Consultant in Paediatric Nephrology, RHCG), Dr Amita Sharma (Consultant in General Paediatrics, RHCG), Ms Evelyn Thomas (UTI Clinical Nurse Specialist, RHCG).
Approved By: RHC Acute Services Approval Group

