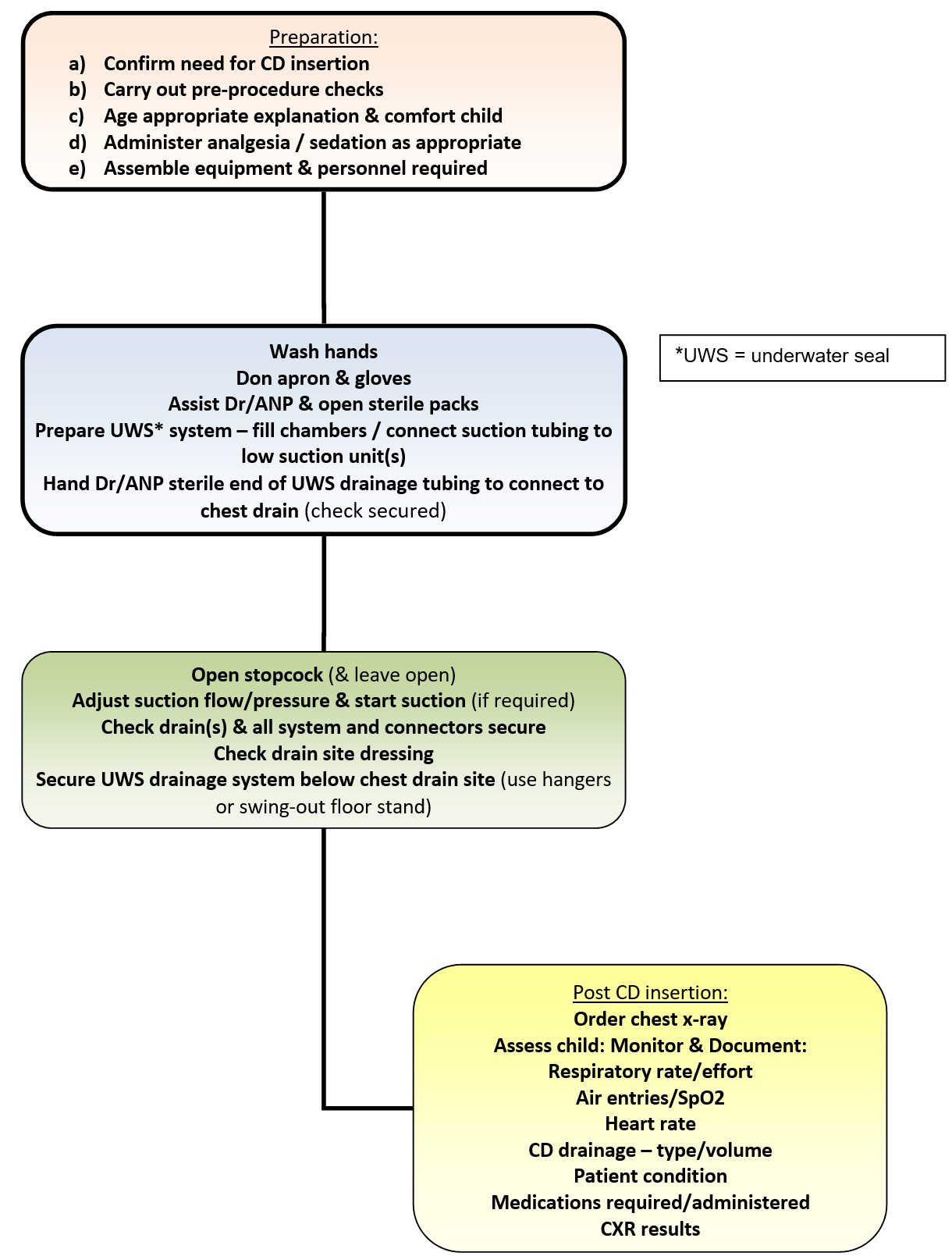
Underwater seal chest drainage in the highly dependent or critically ill infant or child: nurse role: chest drain insertion
Objectives
Chest drains and chest drainage systems are used frequently in the paediatric critical care unit. There are many reasons for chest drain insertion but primarily they are used whenever there are specific conditions that interfere with the normal mechanism of lung expansion and altered intrathoracic pressures.
Pleural chest tubes are inserted to evacuate blood, pus, air and fluid, from the thoracic cavity, to re-establish negative pressure in the intra pleural space and thereby expand the lungs following collapse resulting from surgery or trauma.
Mediastinal chest tubes are placed in the mediastinum following open heart surgery, via a medial sternotomy in order to prevent accumulation of blood and clots around the heart, which could cause cardiac tamponade – a life threatening situation.
There are many different types of chest drains available including one-way flutter valve drains such as the Heimlich device or portable drains. However, for the majority of patients in the paediatric critical care unit an underwater seal chest drainage system will be used. These systems provide an underwater seal, fluid collection chamber and suction chamber.
In paediatric intensive care it is normally the physician or Advanced Nurse Practitioner who inserts chest drains. However, the bed side nurses’ role is pivotal in ensuring the patient is cared for safely throughout the insertion procedure.
This guideline is intended as a resource for staff involved in caring for children in Paediatric Critical Care 1D (PICU) that require chest drain insertion. The guideline has been constructed after literature search and review of sourced textbooks, national guidelines & recommendations British Thoracic Society, Medline and CINHAL, and external nurse expert peer review and opinion.
Further information on chest drainage in: ‘Tutorial Notes-Chest Drainage’ Maxwell (2018) and additional chest drain system resource at: www.atriummed.com/
See also recommendations and precautions.
Scope
This nursing procedural guideline is intended to be followed by nurses involved in caring for the highly dependent or critically ill infant or child requiring underwater seal chest drainage within the Paediatric Critical Care Unit 1D (PICU) at the Royal Hospital for Children, Glasgow.
Audience
All nursing staff involved in caring for infants or children requiring underwater seal chest drainage in Paediatric Critical Care (PICU) should be familiar with this nursing procedural guideline.
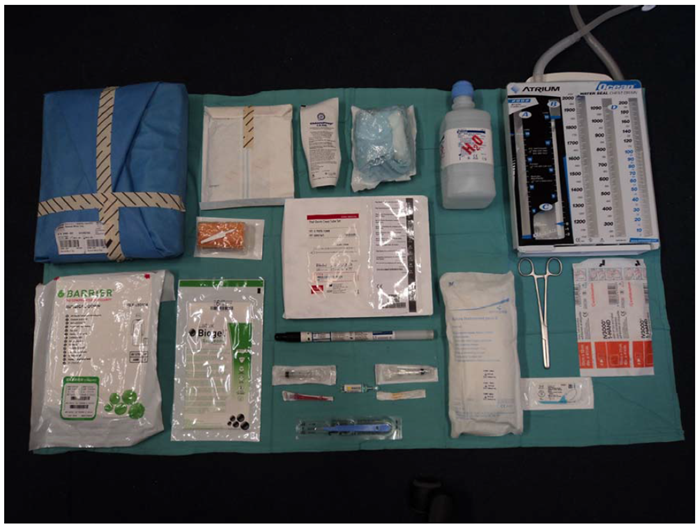
Chest Drain Insertion Trolley (Fig. 1) containing (Fig. 2):
- Appropriate Size/Type Chest drain (E.g. Thal-quick drain)
- Underwater seal chest drainage unit (E.g. Atrium® Ocean Chest Drainage system)
- Dressing pack & sterile drapes
- Sterile gloves & gown
- Sterile Chest drain ‘tray’
- Skin cleaning solution (Chloroprep®)
- Sutures
- Suction suitable connecting tubing
- Sterile water
- Local anaesthetic (Lignocaine 1% or 2%)
- Chest drain clamps
- Chest drain wound site dressing (eg IV 3000/Tegaderm over top of non-adherent dressing)
- At bed space: Wall suction gauge – low flow
Fig 1: Chest drain trolley

Fig 2. Equipment used for chest drain insertion
| Procedure: Chest drain insertion | Rationale |
|
PRE-PROCEDURE: |
|
| Provide age appropriate explanation for procedure | To help alleviate any anxiety and ensure the child (and parent) understand and consent to the procedure. |
| Assess patients pain and conscious level and discuss with doctor to ensure appropriate analgesia and/or sedation is administered prior to the procedure. | Chest drain insertion can be painful and requires medication to promote patient comfort. Sedation may also be required to ensure the patient co-operates with the procedure. |
| Assemble equipment (See Fig. 1 & 2 above) and take to bedside. |
The nurse must be present to reassure the child throughout the insertion procedure and in case of any deterioration in the child’s condition during or after the chest drain has been inserted. Therefore, it is advisable to have all necessary equipment at the bedside to avoid the nurse having to leave the patient. |
| Assisting nurse: wash hands thoroughly with appropriate antimicrobial skin cleanser and don apron | To minimise the risk of cross infection. |
|
PROCEDURE: The doctor/ANP should scrub and prepare for chest drain insertion as an operation using sterile gloves and gown. The assisting nurse should open all equipment needed for the procedure onto the sterile drapes. The nurse should open the under water seal chest drain system onto sterile drapes on trolley. |
To minimise the risk of infection. To ensure the doctor/ANP has all necessary sterile equipment readily available for chest drain insertion |
|
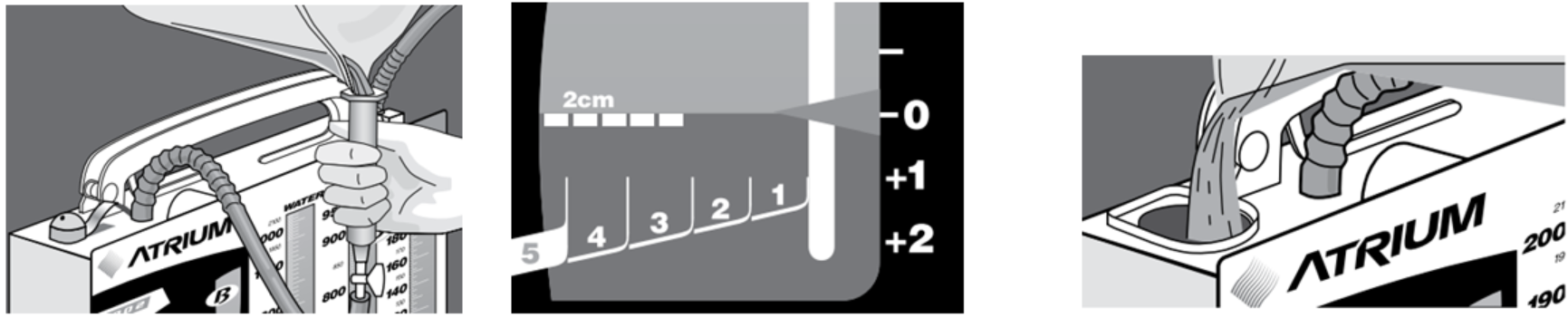
Before use, the water seal chamber (B) should be filled as below* (Fig. 3):
Once filled, water becomes tinted blue for improved visibility of air leaks and convenient monitoring of patient pressures. Once chamber (B) (Fig. 3) filled, disconnect funnel ensuring suction tubing stopcock switched off. This end of the tubing is the suction tubing connection for wall suction if required. Note: Whether or not suction is required it is better to fill the suction chamber (A) (Fig. 3) at this point also. Usually fill to level -20cmH2O. If the doctor/ANP wishes to do this then they will follow the above steps*, keeping the entire system on the sterile drape. The, assisting nurse will only need to pour the water in. (Fig 4 & 5) OR If the assistant nurse is to fill the chambers, the chest drainage system should be handed to the nurse by the doctor/ANP *Note: the sterile end of the tubing will be kept on the sterile drape by the doctor/ANP. The assistant nurse should follow the steps above* (Fig. 6) ensuring sterile end of drainage system connection, remains on sterile drapes until connection to chest required. |
Water Seal Chamber (B) (Fig. 3) must be filled first and maintained at 2cm level to create a seal for closed drainage and keeping air from entering the cavity. This is filled regardless of whether suction is applied from the wall (Atrium 2016).
After set-up, routinely monitor the water level for evaporation and fill with sterile water as necessary. NOTE: It is the water level that determines the amount of negative pressure (Atrium 2016). |
|
Seldinger insertion technique will beused to insert chest drain. Details in: ‘Tutorial Notes-Chest Drainage’ Maxwell (2018) |
|
|
Once drain in correct position it is sutured into place to secure it. Once drain secured, hand physician or ANP the sterile distal end of drainage connecting tubing so it can be attached to the tapered sterile connector when tube is in. |
Two sutures will be used – one solely to secure the drain and the other, a ‘mattress’ or similar suture for closing the wound post drain removal. The suture & type chosen must be suitable for a linear incision. To ensure entire system remains sterile and intact. When hemothorax is suspected, blood exposure can be reduced by connecting drainage tubing to Atrium® drainage system prior to insertion. |
|
If suction required, connect chest drain system to suction source using clear hospital suction connecting tubing. The suction used must be a high volume/low pressure system. Never connect a chest drain on its own to wall suction. It is recommended that each separate chest drainage system has a separate suction source Ensure the chest drain, connectors (single or Y) and suction tubing are all connected to each other securely. Ensure suction tubing stopcock is switched ON. Adjust wall suction gauge (after connecting to patient's chest tube), until there is constant gentle bubbling in the suction control chamber (A) (Fig. 3). Negative pressure of -20cmH2O are most common. |
Continuous suction may be applied through the suction port in the drainage system to enhance drainage and help manage a non-resolving pneumothorax. There is loss of suction if more than one chest drainage system is connected to one suction source Poor tube connections can lead to air leaks in the system. Vigorous bubbling is not only noisy but unnecessary as it can lead to faster evaporation of water in the suction control chamber (A) (Fig.3) but will not increase suction. High levels of negative pressure can cause damage to lung tissue and perpetuate any existing air leaks. |
| A non-adherent dressing with adhesive with transparent occlusive dressing on top, or similar, should then be placed around insertion site. | Large amounts of tape and padding are unnecessary. The dressing should be inspected regularly. If not dry and exudate noted then contact tissue viability nurse for wound care advice. |
|
Use multi-position hangers to hang unit from bedside or place on floor using swing-out floor stand incorporated into base. (To further avoid tipping - base of unit may be secured to floor using tape provided tape is clearly seen E.g. Sleek) |
To ensure the chest drainage unit is kept below the patient’s chest and in plain view to prevent accidental damage or breakage. |
| Ensure a portable chest x-ray is ordered and carried out post chest drain insertion. | A chest x-ray is necessary to verify proper chest drain placement. |
|
Post insertion the nurse should ensure that the patient & family are updated the following are documented:
|
These observations should be carried out pre and post chest drain insertion and thereafter so that they may be compared and the nurse may determine whether the chest drain insertion has improved the patient’s condition or not. |
Fig 3. Underwater seal chest drain unit
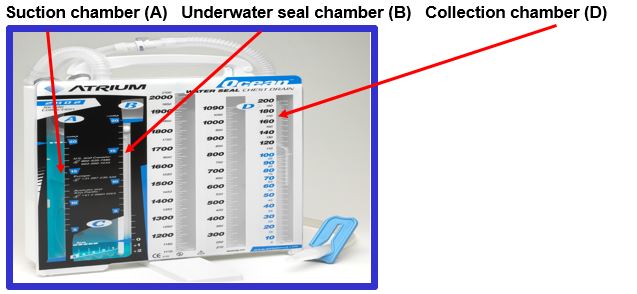
Fig 4. Doctor/ANP filling chamber (B) underwater seal
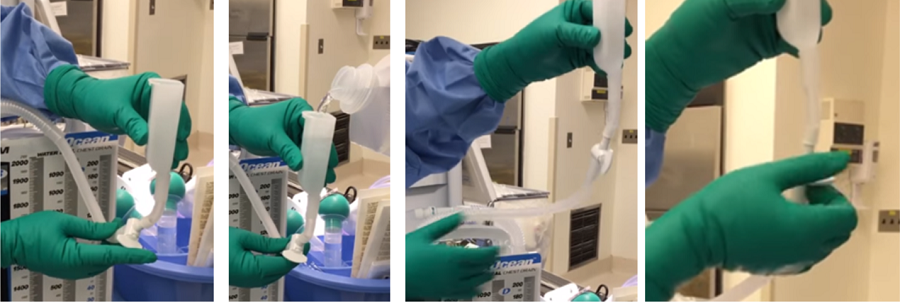
Fig 5. Doctor/ANP filling chamber (A) suction chamber
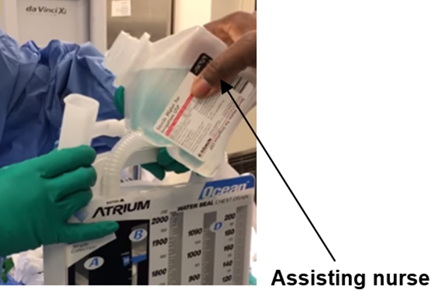
Fig 6. Assistant nurse filling chamber (B) and then (A)
Chest drain insertion is a procedure that is performed by the doctor or ANP in paediatric critical care. However, it is important that the nurse, as well as the physician/ANP inserting the drain, has an understanding of not only the benefits but the risks of such a procedure. It is recommended that all personnel involved with insertion of chest drains be suitably trained and supervised. As such it is recommended that all nursing staff have an understanding of the concepts of chest drainage including the following: anatomy, respiration, indications for chest drainage, risks and ongoing care and management.
Risks: The decision to insert a chest drain is based on clinical findings and patient need and, may be urgent. However, where possible it is prudent to adequately prepare the patient for the procedure. This includes discussion with child and parents, consideration of what sedation, analgesia and anaesthesia may be required, patient positioning and correction of blood clotting or platelet counts.
Sutures: Much of the literature supports the use of a non-absorbable suture (silk) to secure the drain in place and another to close the incision wound once the drain is removed. Physicians/ANP’s should use a suture as recommended as per the PICU Medical Chest Drain Insertion protocol (separate document pending).
Practical chest drainage system issues: When there is no air leak, the water level in the water seal chamber should rise and fall with the patient's respirations, reflecting normal pressure changes in the pleural cavity during respiration. During spontaneous respirations, the water level should rise during inhalation and fall during exhalation. If the patient is receiving positive pressure ventilation, the oscillation will be just the opposite. Oscillations may be absent if the lung is fully expanded and suction has drawn the lung up against the holes in the chest tubes.
A patient with mediastinal chest tubes (and a ‘closed’ chest) should have no bubbling or fluctuations in the water seal chamber. As one of the risks of accumulation of fluid, blood or clots around the heart is cardiac tamponade, it is particularly important for nurses caring for patients with mediastinal chest tubes to be watchful for signs of cardiac tamponade with special attention paid to the volume and consistency of drainage in the collection chamber (D) (Fig. 3).
- Allibone, L (2003) Nursing Management of chest drains. Nursing Standard, Vol.12 (17), pp. 45-54.
- Allibone, L (2005) Principles for inserting and managing chest drains. Nursing Times, Vol. 101 (42), pp. 45-48.
- Atrium (2016) A personal guide to managing chest drainage. Atrium teaching resource accessed at: http://www.atriummed.com/EN/chest_drainage/ocean.asp and http://www.atriummed.com/EN/Chest_Drainage/Documents/Ocean-BlueHandbook010140.pdf
- Balfour-Lynn, IM Abrahamson, E Cohen, G Hartley, J King, S Parikh, D Spencer, D Thomson, AH Urquhart, D (2005) BTS guidelines for the management of pleural infection in children. Thorax, Vol. 60, Suppl. I, pp. i1-i21.
- Bar-El, Y Ross, A Kablawi, A Egenburg, S (2001) Potentially dangerous negative pressures generated by ordinary pleural drainage systems. Chest, Vol. 119 (2), pp 511-514.
- Coughlin, AM Parchinsky, C (2006) Go with the flow of chest tube therapy. Nursing, Vol. 36 (3), pp 36-41.
- Dougherty, L, Lister, S (2004) Intrapleural Drainage: Chest Drain Insertion. In: The Royal Marsden Hospital Manual of Clinical Nursing Procedures. (6th ed). Blackwell Publishing, London.
- Gray, E (2000) Pain management for patients with chest drains. Nursing Standard, Vol. 14 923), pp 40-44.
- Havelock, T Teoh, R Laws,D Gleeson,F (2010) on behalf of the BTS Pleural Disease Guideline group. Pleural procedures and thoracic ultrasound: British Thoracic Society pleural disease guideline 2010, Thorax, Vol. 65 (Suppl.2), pp 61-76
- Lehwaldt, D Timmins, F (2007) The need for nurses to have in service education to provide the best care for clients with chest drains. Journal of Nursing Management, Vol. 15, pp 142-148.
- Luketich, JD Kiss, M Hershey, J Urso, GK Wilson, J Bookbinder, M Ginsberg, R (1998) Chest tube insertion: A prospective evaluation of pain management. The Clinical Journal of Pain, Vol. 14 92), pp 152-154.
- Maxwell, S (2018) Chest Drain Tutorial Notes. Paediatric Critical Care , Royal Hospital for Children, Glasgow
- National Patient Safety Agency (2008) Risks of chest drain insertion: Rapid Response Report NSPA/2008/RRR003.
- NHS Greater Glasgow & Clyde (2016) Infection Prevention and Control: Core prevention policies: Decontamination of Equipment and the Environment; Standard Precautions. NHS Greater Glasgow Control of Infection Committee Policy. NHSGGC.
- Strutt, J Kharbanda, A (2015) Pediatric chest tubes and pigtails: an evidence-based approach to the management of pleural space diseases. Pediatric Emergency Medicine Practice, Vol. 12 (11), pp. 1-24.
- Sullivan, B (2008) Nursing management of patients with a chest drain. British Journal of Nursing, Vol. 17 (6), pp388-393
- Thorn, M (2006) Chest drains: A practical guide. British Journal of Cardiac Nursing, Vol. 1 (4), pp180-185
- Tooley, C (2002) The management and care of chest drains. Nursing Times, Vol. 98 (26), pp 48-50.
- Wrightson, J.M., Fysh, E., Maskell, N.A. & Lee, Y.C.G. (2010) Risk reduction in pleural procedures: sonography, simulation and supervision, Current Opinion in Pulmonary Medicine, Vol.16, pp.340-350
Last reviewed: 01 November 2018
Next review: 01 November 2021
Author(s): Jeanette Grady, Claire Cairney - Clinical Nurse Educators, Paediatric Critical care
Approved By: PICU Clinical Guideline Group

