Prolonged jaundice Neonates (NHSGGC)
Objectives
- To detect important disorders presenting as prolonged jaundice that require further evaluation
- To avoid over investigation of well babies
- To avoid unnecessary hospital visits for well babies and their families
Historically prolonged jaundice screening has been a common reason for attending hospital. The great majority of those attending are well with simple breast milk jaundice and require no more than a split bilirubin as a screen for underlying disorders. To avoid unnecessary hospital visits while ensuring appropriate safety, a new process that minimises the need for attendance has been developed in collaboration between the three GG&C neonatal units and Community Midwifery Colleagues. This process has been successfully trialled and is now fully implemented.
The following pathways have been developed to ensure safe practice based on community lead screening based on three risk categories:
- Well, thriving, breast fed term babies, not at risk of G6PD
- Well, thriving, breast fed <37 week babies, not at risk of G6PD
- Formula fed babies, babies with pale stools/dark urine, clinical concerns or at risk of G6PD
The process can simply be described as- well babies having bloods in the community rather than in hospital, with hospital appointments being reserved for babies with clinical concerns, a higher suspicion of underlying pathology (formula fed babies) and those requiring additional bloods (those at risk of G6PD). Preterm babies are managed slightly differently to reflect the fact that acute jaundice issues can be more persistent in this group so additional sampling may be required for immediate jaundice management, and that jaundice may go on until day 21 in this group. These processes are described in boxes below, with flow charts as well for additional clarity
Applicability
Newborns 14- 21 days of life under the care of NHS GG&C Community Midwives, or in hospital settings in GG&C.
For babies being cared for in the NHS Lanarkshire area, the usual process of seeing in hospital should be followed as blood taking is not currently possible in the community in those areas
Prolonged jaundice is used to describe neonatal jaundice persisting beyond 14 days of life. At this point the emphasis is no longer on prevention of kernicterus, but on investigation to rule out an underlying abnormality that is causing the jaundice to persist at this point. The overwhelming majority of infants who remain jaundiced at 14 days of age will have benign self-resolving breast milk jaundice. A small number will however have an underlying disorder which requires further evaluation and treatment, principle amongst those is extrahepatic biliary atresia for which the prognosis is improved by early diagnosis.
The testing is based on a risk based clinical assessment followed by targeted investigations, which mean that well breast-fed infants with pigmented stools need just a “split bilirubin” to confirm that the jaundice is all unconjugated- with further investigations if a significant conjugated fraction is detected. Unwell babies, particularly those with pale stools will require a more comprehensive evaluation.
The pathway described below should be used in conjunction with the West of Scotland MCN Neonatal Jaundice Guideline which describes in detail the management of neonatal jaundice including prevention of kernicterus. All acute jaundice issues should be resolved before utilising this pathway.
Aims
- To detect important disorders presenting as prolonged jaundice that require further evaluation
- To avoid over investigation of well babies
- To avoid unnecessary hospital visits for well babies and their families
|
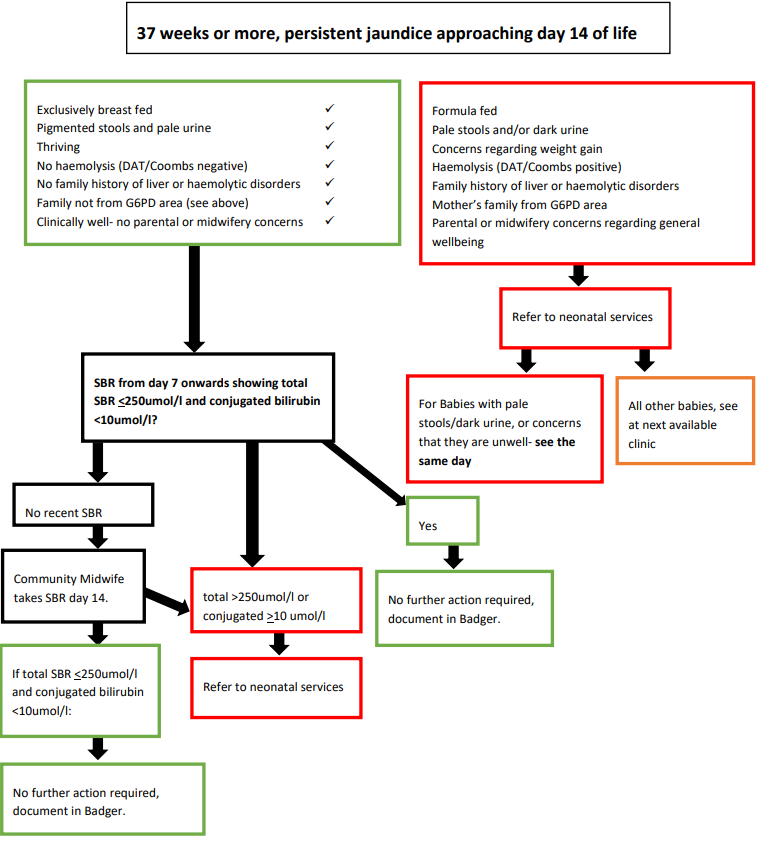
Well, thriving, breast fed term babies, not at risk of G6PD*: Community Management
Management: SBR from day 7 onwards showing total SBR < 250 umol/l and conjugated bilirubin <10umol/l
No recent (after day 7) SBR? Community Midwife takes SBR during scheduled visit - day 10 or more, day 14 ideally. If total SBR >250umol/l or conjugated bilirubin >10umol/l: |
|
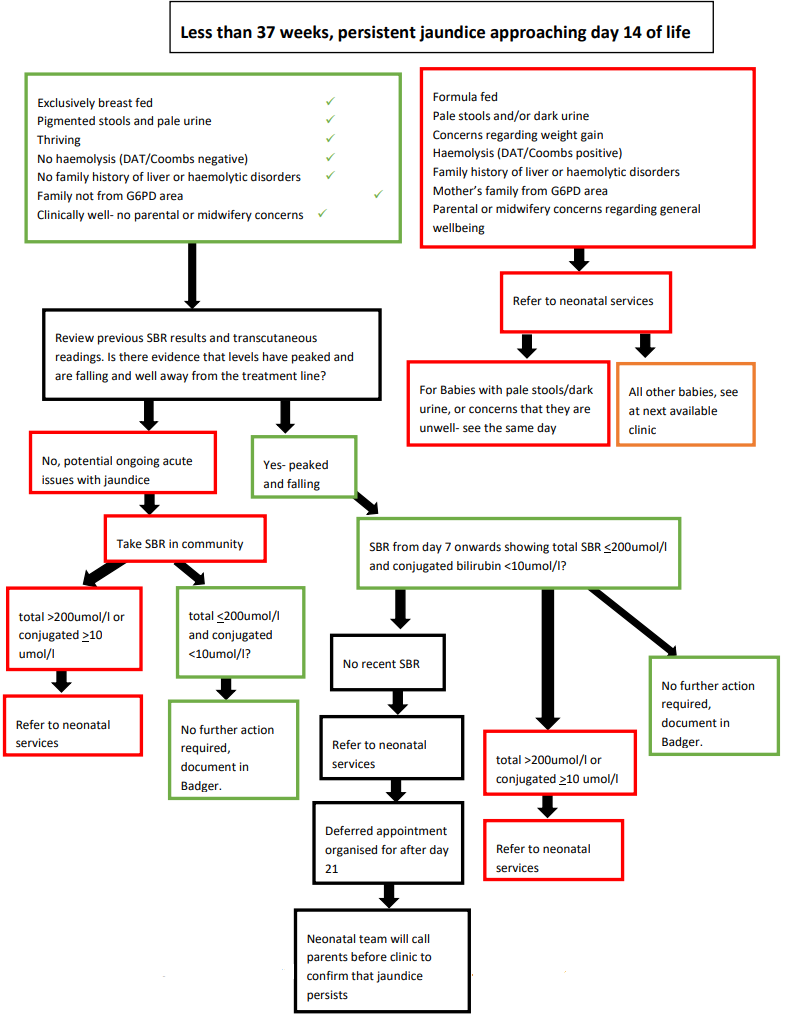
Well, thriving, breast fed <37 week babies, not at risk of G6PD*: Assess as follows
Management: Assess need for further SBR at 10-14 days:
|
|
Formula fed, pale stools/dark urine, clinical concerns, G6PD risk: Refer to Hospital Babies not meeting the Community management criteria:
Management: Refer to Neonatal services - number below For babies with pale stools/dark urine, or concerns that they are unwell - see the same day |
|
For advice, or to make a referral, call the following numbers: RHCG: 0141 452 4965 PRM: 0141 451 5222 RAH: 0141 314 7035 |
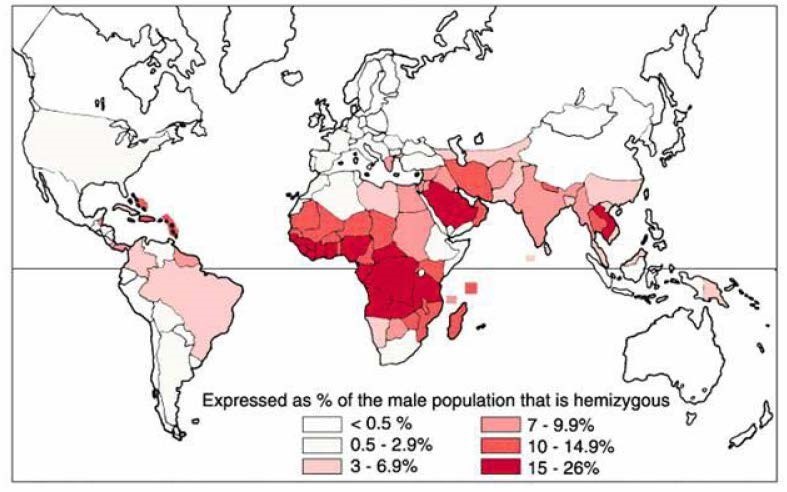
*G6PD Risk – If the mother’s family (or both parents, but not the father alone as G6PD is X linked) are from:
- Sub-Saharan Africa
- The Middle East
- South East Asia
As denoted on the map below then the baby will require additional sampling for G6PD and so will be referred for hospital management.
Last reviewed: 06 July 2021
Next review: 01 July 2022
Author(s): Allan Jackson, consultant neonatologist PRMH, Andrew Powls, consultant neonatologist PRMH, Lesley Jackson, consultant neonatologist RHCG, Anne Marie Heuchan, consultant neonatologist RHCG, Hilary Conetta, consultant neonatologist RAH, Jennifer Mitchell, Consultant Neonatologist RHCG, Veronica McArthur, community midwife (retired)
Co-Author(s): Other professionals consulted: Julie Boyd RCM representative

