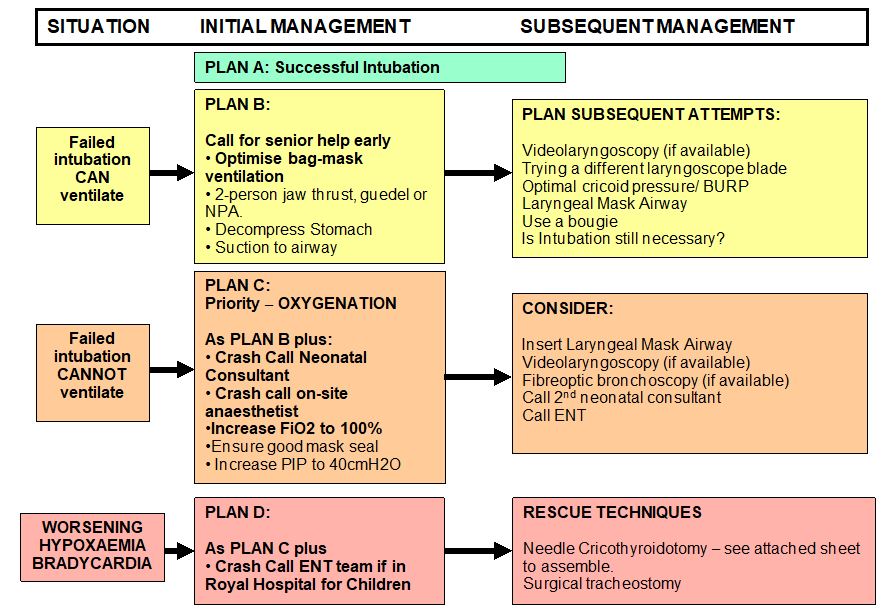
Management of the difficult airway, neonates
exp date isn't null, but text field is
Objectives
The rapid provision of effective ventilation is the single best predictor of successful neonatal resuscitation (1). Ineffective ventilatory support leads to hypoxia and increased morbidity and mortality (2). Endotracheal intubation is a highly-skilled procedure providing a secure airway for effective positive pressure ventilation. There are situations where intubation can be difficult either at, or after, delivery. Before undertaking any intubation attempt it is important to consider the experience of the person intubating, if the appropriate help and equipment is available, if there are any indicators that might make intubation more difficult and what steps you will take in the event that intubation is not possible.
This guideline provides an approach to difficult neonatal intubation. It must be remembered that the primary goal is to adequately oxygenate the baby until a definitive airway can be established. Intubation is not always required in order to achieve this. Multiple unsuccessful intubation attempts can further compromise a difficult airway.
In situations where an airway is deemed as ‘difficult’, this should clearly be stated at the front of the patient notes.
Users of this guideline should be aware of the West of Scotland MCN guideline: “Intubation & Premedication of neonates” which outlines the pathway for uneventful intubation.
In most babies, laryngoscopy results in a clear view of the larynx. However, this is not always the case. The view of the larynx is classified as follows (3):
- Grade 1 – visualisation of the entire laryngeal aperture. There should be little difficulty with intubation.
- Grade 2 – visualisation of the posterior portion of the laryngeal aperture. There may be some difficulty passing the ETT. We can attempt to improve this view by applying ‘cricoid’*.
- Grade 3 – only the epiglottis can be visualised. This can result in severe difficulties. Cricoid/ BURP may help visualisation.
- Grade 4 – only visualisation of the soft palate is possible. Intubation is always difficult and usually accompanies obvious pathology but may also occur unexpectedly (Figure 1).
Figure 1: Laryngoscopy views
* By ‘cricoid’ we actually mean ‘BURP’ which stands for applying Backwards, Upwards, Right Pressure to the larynx. Cricoid in the truest sense of the word means compression of the oesophagus to prevent aspiration.
Figure 2: ‘BURP’
 |
1 - ‘Backward’ pressure towards cervical spine 2 - ‘Upward’ pressure towards jaw 3 - ‘Right pressure’ – push larynx towards baby’s right. |
Whilst the majority of neonatal intubations are straightforward there are some situations where intubation can be very difficult. In the majority of cases, these situations can be predicted beforehand however there are occasions when difficulties with intubation occur unexpectedly (2).
ANTICIPATED
- Babies with diagnoses suspected antenatally which may predispose to a difficult airway should be discussed with fetal medicine at the RHC, Glasgow with a view to delivery at the QEUH.
- This guideline does not include planning for EXIT procedure.
- In cases where intubation is expected to be difficult, a full resuscitation team of neonatal consultant, registrar, SHO and senior nurse should be assembled prior to attempting intubation where possible.
- In cases where there is expected to be an issue with the airway at delivery, a full resuscitation team including Neonatal Consultant should be present at the delivery. These babies should, where possible, be known to the neonatal team through antenatal ‘high risk’ discussions. The possibility of a problematic airway in baby should clearly be highlighted in the mum’s notes antenatally.
- If the intubation/ delivery are taking place in the QEUH, alert the on-call consultant paediatric anaesthetist and ENT surgeon at the RHC prior to starting.
- Avoid muscle relaxation to preserve spontaneous respiratory effort. Sedation can be used although consider lower doses of opiates.
- If the intubation/ delivery are taking place in other hospitals, consider alerting the on-site anaesthetic team.
- In cases where this is not possible (i.e. emergency intubation is required on the NICU or baby delivered out of hours), the Neonatal Consultant should be contacted immediately to attend and intubation should be attempted by the most experienced member of the team. Consultant anaesthetist and ENT help should be considered early.
- The following abnormalities should raise the suspicion that intubation may be difficult:
- Craniofacial abnormalities:
- Achondroplasia
- Beckwith Weidemann syndrome
- Cleft palate
- Goldenhar syndrome
- Laryngeal cysts
- Pierre-Robin sequence
- Treacher-Collins syndrome
- Downs syndrome
- Cystic Hygroma
- Vascular malformations involving the head and neck
- Recurrent previous intubations leading to laryngeal oedema
- Previous difficult intubation.
UNANTICIPATED
- In cases where a baby is unexpectedly difficult to intubate, call for help immediately as per the WoS ‘Management of the Difficult Airway’ flowchart (appendix 1). This may include calling:
- 2nd neonatal consultant,
- on-call for anaesthetics
- on-call for ENT.
- Intubation should be attempted by the most experienced member of the team. Where possible, LIMIT THE NUMBER OF ATTEMPTS TO 2 PER PERSON.
- Continue to attempt effective Neopuff ventilation. Pressures should be titrated based on the baby’s heart rate and saturations.
- The following situations can lead to unexpected airway issues:
- Subglottic stenosis
- Laryngeal atresia
- Tracheal agenesis
- Laryngeal or tracheal webs
- Airway oedema post extubation
- Airway trauma
All equipment must be checked regularly and after usage by a named member of nursing staff. The difficult airway packs must be kept fully stocked at all times with all equipment in date. Any problems should be reported during the morning safety brief.
THE ‘DIFFICULT AIRWAY PACK’
The following equipment can be found in the Difficult Airway Pack:
- Laryngoscope handles
- Miller blades size 00, 0, 1
- Macintosh blades size 0, 1
- Robert Shaw blades size 0, 1
- Blades for videolaryngoscopy (if available)
- Endotracheal tubes size 2.0, 2.5, 3.0, 3.5
- Introducers
- Neonatal bougies
- Guedel airways size 00, 0, 1
- Yankauer suction catheters
- Neonatal size Magill’s forceps
- Size 00, 0, 1 laryngeal masks airways/ iGels
- ‘Neobar’ ETT fixators of all sizes
- Pedicap
- Elastoplast
- Lubricating gel
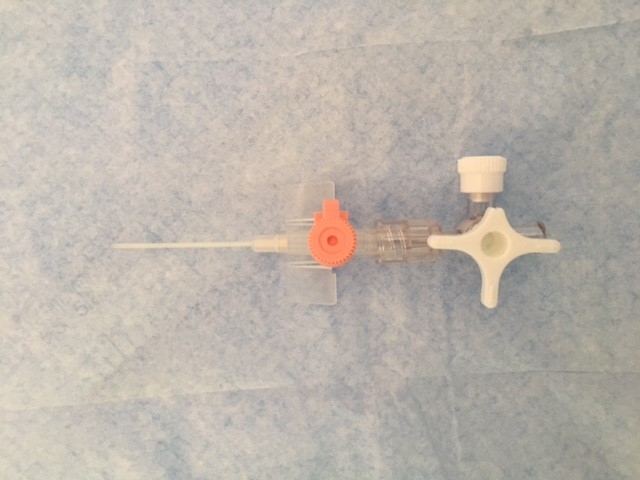
- Pink & green cannulae
- 3 way taps
- Green oxygen tubing
- 5ml IV syringes
- Scissors
Attached to the pack there should also be the following laminated charts:
- The ‘West of Scotland Difficult Airway Flowchart’
- Easy assembly of needle cricothyroidotomy equipment
LMA use is widespread amongst anaesthetists and it can be a life-saving device in situations where maintaining an airway or intubation is proving difficult. Once the skill is developed, insertion of an LMA takes around 5 seconds (4) and studies indicate it can allow pressures of up to 40cmH2O to be delivered (4). It takes practice and instruction and can make things worse if done incorrectly. Although recommended for babies >2kg in weight, there is evidence of successful use of LMAs in babies as small as 1kg (5).
LEARNING POINT: In the West of Scotland, we use the i-Gel™ supraglottic airway (Intersurgical, Liverpool, NY, USA). The i-Gel uses a non-inflating, soft gel cuff which may reduce trauma to soft tissue.
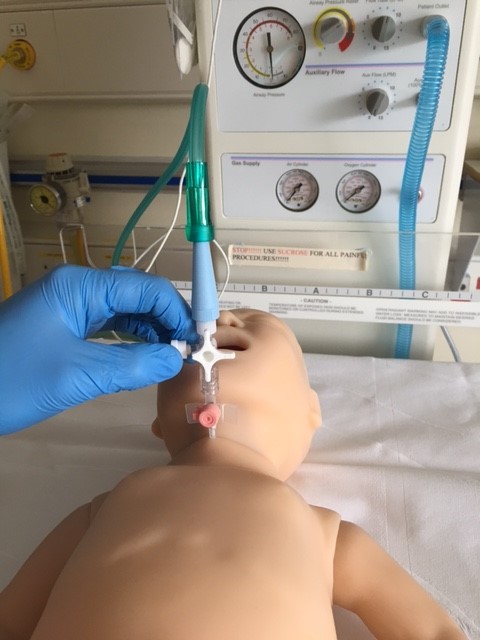
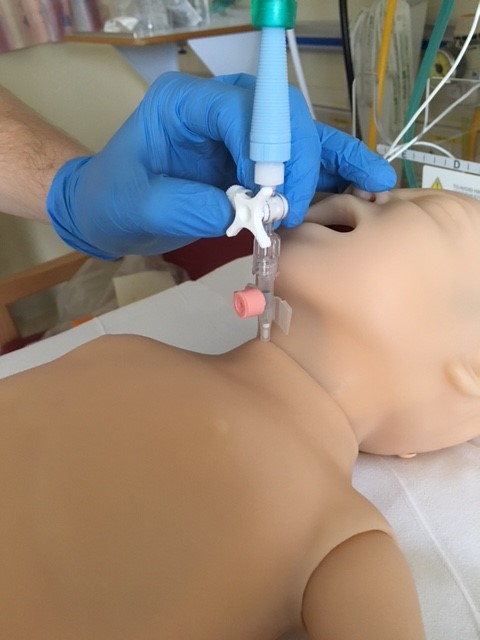
Insertion of a supraglottic airway
- Where possible, using a T-piece, pre-oxygenate
- Lubricate the back and sides of the LMA/iGel
- Tilt the babies head back slightly, open the mouth and apply jaw thrust.
- Insert the tip of the LMA/iGel along the hard palate with the open side facing the tongue.
- Continue inserting the LMA/iGel along the posterior pharyngeal wall. Resistance is felt when the LMA/iGel tip sits on the oesophagus. The opening of the mask should cover the entrance to the larynx (See figure 2).
- If using an LMA, inflate the cuff until a good seal is formed.
- Secure the LMA/iGel to the ‘Neobar’ ETT fixator with adhesive tape (See figure 3).
Figure 2: The final position of the iGel in the airway
Figure 3: Fixation of the iGel
VIDEOLARYNGOSCOPY
The use of videolaryngoscopy for intubation is a new development in neonatology. It is a useful tool in the teaching of intubation to junior trainees and reduces the stress of the intubator (6). It’s use in the difficult airway allows viewing of a larger image onto a screen enabling potentially improved view of the larynx.
FLEXIBLE BRONCHOSCOPY
Flexible Bronchoscopy can be used in cases of difficult intubation. For cases in the RHC NICU where elective intubation is predicted to be difficult, a bronchoscopist skilled in intubation (Dr Coutts or Dr Peters) should be on standby wherever possible.
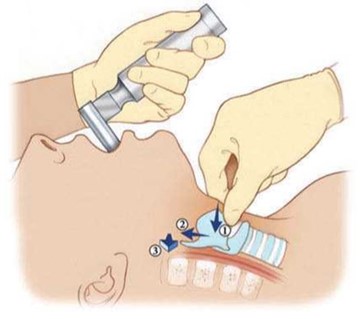
NEEDLE CRICOTHYRODOTOMY
This involves the insertion of a pink or green cannula through the cricothyroid membrane. This is a ‘last resort’ scenario and should only be used when the baby cannot be adequately enough oxygenated to maintain heart rate.
Remember: this procedure allows oxygen delivery to the lungs. It is not an effective means of ventilating and is used as a means of oxygenating until a surgical airway can be established.
See Appendix 6: Set-up for needle cricothyroidotomy
SURGICAL TRACHEOSTOMY
- For babies in the RHC NICU– contact the RHC on-site paediatric anaesthetist and on-call paediatric ENT Consultant via switchboard who will attend urgently.
- Tracheostomy equipment is available in the unit.
- For babies in the PRMH and RAH NICUs - there is currently no out of hours ENT cover available to attend these units. The on-call ENT consultant at the RHC should be contacted as well as the on-call transport consultant. Where possible, arrangements should be made to transfer the baby urgently to the RHC.
- For babies in Forth Valley, Wishaw and Ayrshire Maternity NICUs – contact the local ENT on-call team to attend urgently. The local ENT team can contact the RHC on-call paediatric ENT Consultant for advice.
Although intubation allows a definitive airway, it is not necessary for adequate ventilation provided the baby receives good bag-mask ventilation. Effective bag-mask ventilation is indicated by chest wall expansion with a rising heart rate remaining greater than 100.
LEARNING POINT: effective bag-mask ventilation can be as effective as ventilation through an endotracheal tube
If, however, the baby continues to require respiratory support with bag-mask ventilation, it is reasonable to attempt intubation as long as clinician with adequate experience is available.
- Ensure a resuscitation team is assembled and everyone is aware of their job within the team. The most senior member of the team should be allocated the ‘leader’. Ideally, in cases of an expected difficult airway, the team leader should not be the person taking charge of the airway. This allows the person managing the airway to concentrate fully on this.
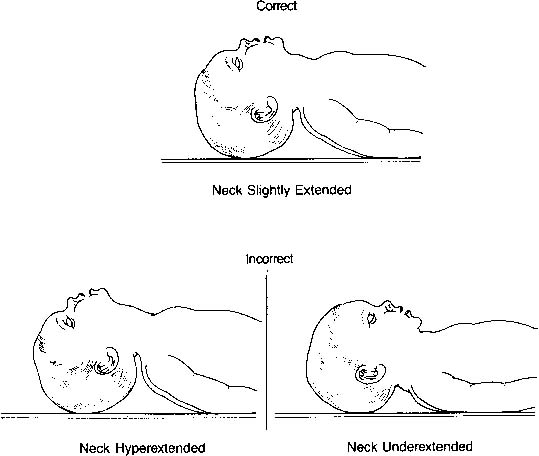
- Position the airway to achieve adequate chest wall movement. Remember the ‘neutral position’ in babies (Figure 4). A towel roll can be used to improve the position.
- In situations where the heart rate and saturations remains adequate, it is reasonable to premedicate the baby with fentanyl and suxamethonium for intubation - See West of Scotland MCN guideline: “Intubation & Premedication of neonates”
- Preoxygenate as much as possible. Remember, achieving saturations of 100% in a baby can be difficult.
- Attempt intubation a maximum of twice. If the first attempt does not succeed, consider calling for help and readjusting position for example to facilitate intubation.
If intubation is successful, confirm position by:
- Maintenance of heart rate
- ‘Pedicap’ colour change to yellow
- Equal air entry – listening in the axillae and also over the stomach.
Fix ETT in place using nasal-tragal length as a guide for depth of insertion.
Ensure ETT remains above the carina on chest X-ray
Figure 4: Correct positioning of the neonatal airway
In this situation, effective bag-mask ventilation is absolutely necessary. We would advise a maximum of 2 attempts at intubation in total by the Registrar. Each attempt should last no more than 30 seconds. In between attempts, the resuscitator should return to bag-mask ventilation via the T-piece.
LEARNING POINT: repeated attempts at intubation can cause damage to the airway and should be avoided.
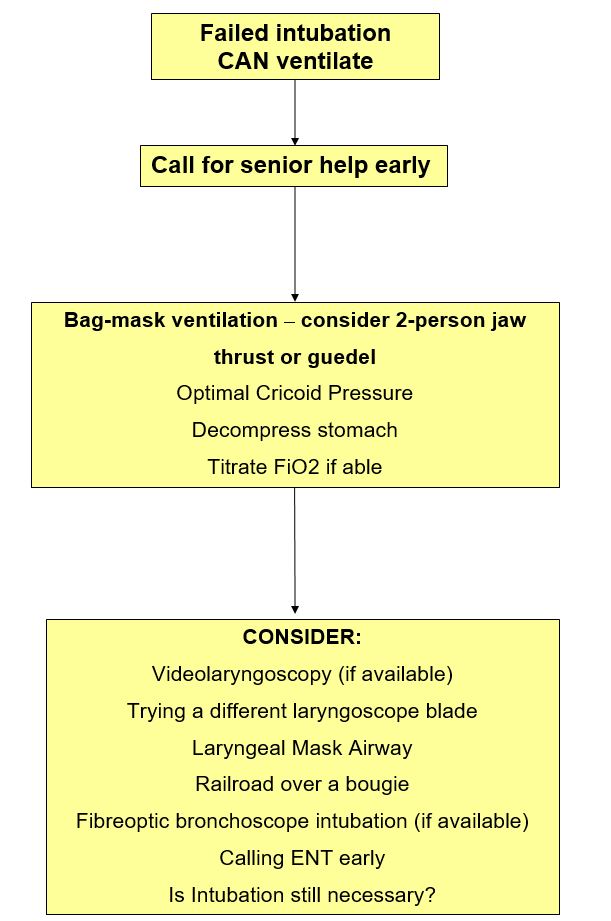
Where intubation is proving difficult, the resuscitator should:
- Call for help from the on-call neonatal consultant
- THINK: Does this baby definitely require intubation and ventilation?
- Continue bag-mask ventilation
- Aspirate the nasogastric tube regularly to decompress the stomach.
- Use a 2 person jaw thrust or insert a guedel to make bag-mask ventilation easier.
Where ventilation is adequate through bag-mask ventilation however intubation is proving difficult, it is important to remember that repeated intubation attempts can damage the airway and make bag-mask ventilation more difficult. The resuscitator should await senior support.
In situations where intubation is proving difficult for the consultant, consider the following:
- Call a 2nd consultant
- Consider try a different-sized laryngoscope blade which may improve the view of the cords,
- If familiar with the use of a bougie, consider inserting through the cords and ‘railroading’ the ETT over this.
If intubation continues to prove difficult:
- Continue bag-mask ventilation
- Aspirate the NG regularly
- Consider LMA.
- Consider fibreoptic intubation if Dr Coutts or Dr Peters available.
- If in RHC NICU or PRM NICU:
- Contact the paediatric ENT and anaesthetic team for assistance
- For all other hospitals:
- Contact the local anaesthetic team for assistance.
- Reversal of anaesthetic is usually not required due to the short-acting nature of fentanyl and suxamethonium. However, one can consider using:
- Naloxone (200 micrograms I.M.)
- Sugammadex (2mg/kg) can be used in babies muscle-relaxed with rocuronium.
See Appendix 2 – ‘The Can’t Intubate, Can Ventilate’ Flowchart
LEARNING POINT: Call for help early!
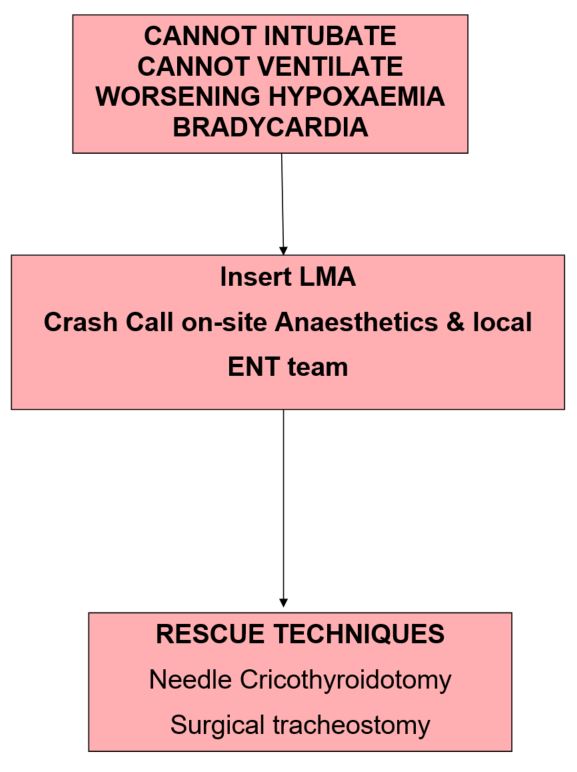
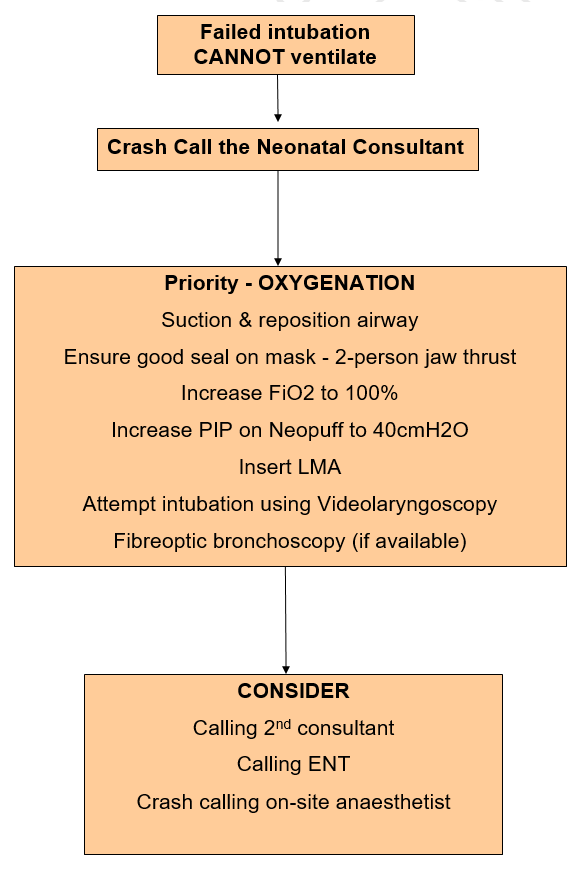
This is the situation where intubation has proven unsuccessful and bag-mask ventilation is proving inadequate as shown by low saturations and a falling heart rate.
However, in most situations the situation can be improved by simple ‘trouble-shooting’ techniques:
- Check that airway is clear
- Suction under direct vision
- Reposition the airway – remember neutral position
- Check T-piece system is working correctly
- Attempt bagging with high pressures (up to 40cmH2O)
- Ensure a good seal with the mask around the baby’s face:
- Try a 2-handed technique
- Insert a Guedel airway or iGel
If these have been worked through and the situation remains critical, this is a medical emergency.
- The Neonatal Consultant must be ‘crash-called’
- The on-site anaesthetist should also be ‘crash-called’
- Try inserting a LMA – maximum 2 attempts (See figure 2)
- Set-up for needle cricothyroidotomy – See Appendix 4
- If in RHC NICU:
- Contact the on-call ENT team.
- For all other hospitals:
- Contact the local anaesthetic team to attend urgently
- Contact the on-call paediatric ENT team at RHC for advice
- Proceed to needle cricothyroidotomy OR
- ENT perform emergency tracheostomy
LEARNING POINT: Needle cricothyroidotomy only helps with oxygenation. It cannot provide ventilation.
See Appendix 3 – ‘The Can’t Intubate, Can’t Ventilate’ Flowchart
See Appendix 4 – ‘The Critical Situation’
See Appendix 5 – ‘Checklist for the Problematic Intubation’


West of Scotland Managed Clinical Network
The Expected Difficult Airway Checklist
Prior to commencing intubation, the WoS Intubation & Premedication Guideline should be read and understood.
|
Does this baby have a condition making intubation likely to be problematic? |
Yes / No |
|
Is there an appropriate team available?
|
Yes / No |
|
Is the ‘difficult airway pack’ fully stocked? |
Yes / No |
|
Is the ‘difficult airway pack’ readily available |
Yes / No |
|
Are anaesthetics/ ENT aware of the situation prior to starting? |
Yes / No |
|
Does each team member have an allocated role? |
Yes / No |
|
Is there a clear plan for escalation based on the WoS difficult airway flowchart? |
Yes / No |
|
Is the WoS difficult airway flowchart clearly accessible? |
Yes / No |
|
Is an LMA readily available? |
Yes / No |
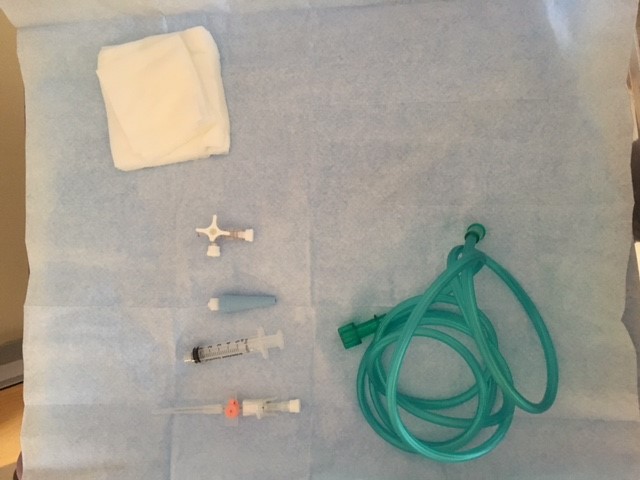
Required Kit:
- Dressing pack
- Gauze swabs
- 3 way tap
- 5 ml syringe
- Green or pink IV cannula
- Oxygen tubing connector
- Green Oxygen tubing.
Procedure:
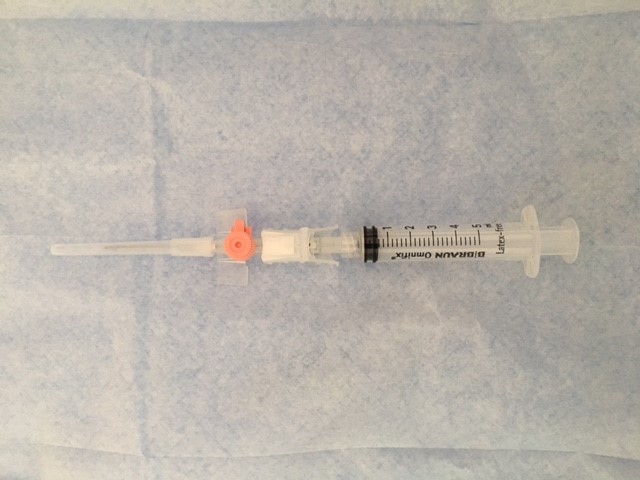
- Extend baby’s neck and palpate for the thyroid cartilage (superior) and the cricoid cartilage (inferior). The space in between this is the cricothyroid membrane.
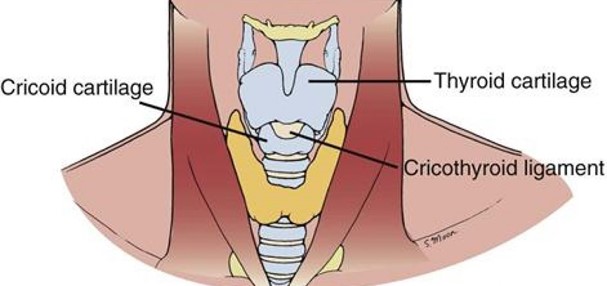
- Stabilise the cricothyroid membrane with one hand between finger and thumb. At an angle of 45 degrees, pierce the cricothyroid membrane with the cannula and aspirate the syringe at the same time. When the cannula enters the trachea, air should be easily aspirated.

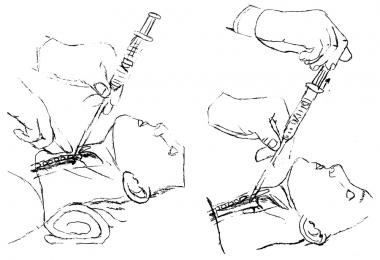
- Advance the cannula over the introducer needle into the trachea. Be careful not to kink the plastic cannula.
- Small tidal volumes can be delivered 2 ways:
- Repeated opening and closing of the 3 way tap. Opening allows oxygen to be delivered to the baby allowing a degree of lung inflation. To allow exhalation, close the 3 way tap.
- Pierce a small hole in the green oxygen tubing. This hole can be covered and uncovered with a finger in order to deliver a breath.
|
Open (inspiration) |
Closed (expiration) |
- Kattwinkel J. Textbook of Neonatal Resusitation. 4th Edition. Illinois. American Academy of Pediatrics: 2000.
- Johansen L.C., Mupanemunda R.H., Danha R.F. Managing the newborn infant with a difficult airway. Infant 2012; 8(4): 116-19.
- Walker RWM, Elwood J. The management of difficult intubation in children. Pediatric Anesthesia 2009; 19 (Suppl. 1): 77–89
- Trevisanuto D., Micaglio M., Pitton M. et al. Laryngeal mask airway: is the management of neonates requiring positive pressure ventilation at birth changing? Resuscitation 2004;62:151-57.
- Gandini D., Brimacombe J.R. Neonatal resuscitation with the laryngeal mask airway in normal and low birth weight infants. Anaesth Analg1999;89:642-43.
- O'Shea JE, Thio M, Kamlin CO, McGrory L, Wong C, John J, Roberts C, Kuschel C, Davis PG. Videolaryngoscopy to Teach Neonatal Intubation: A Randomized Trial. Pediatrics. 2015 Nov;136(5):912-9. doi: 10.1542/peds.2015-1028.
Last reviewed: 11 December 2020
Next review: 01 November 2023
Author(s): Dr Andrew MacLaren – Neonatal Grid Trainee – GG&C
Co-Author(s): Other Professionals consulted: Dr Kathleen O’Reilly – Neonatal Consultant – RHC; Dr Colin Peters – Neonatal Consultant - RHC; Dr Jonathan Coutts – Neonatal Consultant – RHC; Dr Joyce O’Shea – Neonatal Consultant – RHC; Dr Rob Ghent – Consultant Anaesthetist - RHC
Approved By: West of Scotland MCN for Neonatology