Newborn Blood Spot Screening
exp date isn't null, but text field is
This guideline is applicable to all medical, nursing and midwifery staff caring for the newborn in the West of Scotland. It has been written to comply with the recommendations laid out in the QIS (Quality Improvement Scotland) Clinical Standards Document1 published in October 2005 and updated in July 20082. These standards aim to ensure that Newborn Blood spot screening is offered to all babies. The standards also aim to ensure that the collection of samples, laboratory testing and initiation of treatment in positive cases are completed efficiently so that affected babies achieve maximum benefit from early and appropriate treatment.
More detailed information for Healthcare Professionals is available at http://www.pnsd.scot.nhs.uk/newborn
Staff should also familiarise themselves with the contents of the updated information leaflets for parents:
From 20th March, 2017 the Scottish Newborn blood spot screening programme will include nine conditions:
- Phenylketonuria (PKU)
Autosomal recessive
Incidence in Scotland approximately 1 in 8,000
Test detects elevated levels of phenylalanine
Early treatment prevents the development of serious, permanent learning disability
Screen positive babies are reviewed immediately: the diagnosis should be confirmed and treatment with a low phenylalanine diet started by 21 days of life
- Congenital hypothyroidism (CHT)
Incidence 1 in 3,500
Test detects raised levels of TSH (thus will not detect rare cases of hypothalamic hypothyroidism)
Early treatment essential to prevent or minimise learning disability
Screen positive babies are reviewed immediately at the neonatal unit, thyroid function checked and investigations ordered after discussion with the on-call endocrinologist Thyroid replacement therapy is usually started at this visit or the following day, and arrangements must be made (by telephone) for prompt follow up at Yorkhill
- Cystic Fibrosis (CF)
Autosomal recessive
Incidence 1 in 2,500
Test detects raised levels of immunoreactive trypsin: confirmation is by DNA testing from the same blood spot
Cases referred to respiratory team, and for genetic counselling. Babies should be seen and started on treatment by day 35
Screening will identify some carriers who will be offered an appointment with a genetic counsellor (this is dealt with in general practice)
- Medium Chain Acyl-CoA Dehydrogenase Deficiency (MCADD)
Autosomal recessive
Incidence 1 in 10,000 to 1 in 20,000
Impaired fat metabolism places the child at risk of severe hypoglycaemia, particularly with intercurrent illness. First presentation may be sudden death
Average age at presentation in unscreened populations is 14 months. Mortality is 15-20% and up to 30% of survivors sustain brain damage
Management is to prevent metabolic crises by ensuring an adequate supply of carbohydrate
- Sickle Cell Disease (SCD)
Autosomal recessive
Incidence 1 in 2500, mostly in Black African children
Carries a risk of sickle crises which may be complicated by infections, anaemia, stroke and/or death
Affected babies should receive pneumococcal vaccine and prophylactic penicillin
Testing may detect carriers: they will be offered an appointment with a genetic counsellor
- (As of 20th March, 2017)
Maple syrup urine disease (MSUD)
Isovaleric acidaemia, (IVA)
Glutaric aciduria type 1 (GA1)
Homocystinuria (HCU)
These four rare recessively inherited metabolic conditions were added to the newborn blood spot screening programme for babies born on or after 20th March, 2017. They are incorporated in a testing panel together with MCADD and PKU – parents can elect to have all six conditions tested for, or to have all six excluded from testing, Note that for technical reasons, parents can no longer opt out of only some of the metabolic conditions for which testing is available.
The incidence of MSUD, IVA, GA1 and HCU is very rare, at between 1 in 100,000 and 1 in 200,000; the test only detects affected children who will then be offered dietary advice and follow up. Early dietary treatment of each of these inherited metabolic disorders improves prognosis.
QIS Standard 4b - All Women / Parents / Carers receive clear information (written or in other formats) to help them to make an informed choice about newborn screening.
- Outline information about newborn blood spot screening is available in the “Ready Steady Baby” book which is given to all mothers-to-be at booking.
- Following the birth all mothers should be given the leaflet 'Your Guide to Newborn Screening Tests'. The leaflet is available in a number of other languages via the Health Scotland website
If the mother does not speak any of these languages then an interpreter should be arranged to ensure that an informed decision can be made. Individual arrangements must also be made for parents and/or carers with visual or learning difficulties which prevent them from reading the printed material. - Information about the test should have been received at least 48hours before the blood spot specimen is taken and parents/carers must be given the opportunity to ask questions of an appropriately trained health professional, using an interpreter if required. If the questions asked by the parents/carers cannot be answered by the health professional then they should be referred to a senior member of the medical staff.
- Written consent must be taken before the sample is acquired and the completed form retained in the Health Record. See Appendix for Consent form
NB. The consent form should be completed and retained even if testing is declined. - Consent will usually be taken from the mother. If this is not possible then consent may be sought from another person with parental responsibility (See Appendix 1). If no person with parental rights is available to give consent then advice should be sought from the Central Legal Office.
- If one or more of the screening tests is declined parents/carers should be informed of the action they should take if they change their minds or if symptoms or signs of the condition appear in their child. Signs and symptoms may be non-specific, and so any change in the child’s condition should result in prompt review by either the midwife or GP. Parents should also be informed that some or all of the benefits of screening may be lost if the test is delayed. Note that parents must accept all decline all 6 metabolic conditions; it is no longer possible to opt out of some. Parents may opt out of all 6 metabolic conditions, but still accept other screening tests.
- This information is available in written form (See Appendix) but staff must still ensure that the parents/carers understand the information. A standard letter should be sent to the General Practitioner informing them that the infant has not been tested (See Appendix).
- If parents change their mind shortly after the screening test was offered then the blood spot screen should be performed. A subsequent change of mind should be dealt with by the GP or Health Visitor who can liaise with the screening laboratory or local Paediatrician to determine the most appropriate means of testing.
- If the infant is premature, generally unwell, or shows specific signs or symptoms of one or more of the conditions covered by the newborn screening programme then testing for these conditions should proceed in the child’s best interests. Hopefully the parents will be persuaded of the clinical need for these investigations but failing this advice should be sought from the Central Legal Office.
CHT, metabolic, CF and SCD screening tests are offered for all babies between 96 and 168 hours of life.
QIS Standard 4a2
95% of positive CHT and PKU cases have started treatment by 14 days of age, unless deliberately delayed for further testing. QIS Standard 4e2
- The blood spot specimen should be obtained on day 5 of life wherever possible including bank holidays and weekends. The date of birth is counted as day 0, regardless of the time of birth (NB this is at variance with the Badger information system which counts date of birth as day 1).
|
Local Arrangements to ensure that a blood spot specimen is obtained prior to a red cell transfusion
|
- The timing of the first specimen should not be delayed, even if the baby is premature, unwell or parenterally fed. Repeat specimens are required for premature infants - see below.
- The specimen should be mailed to the screening laboratory the same day.
When parents decline the screen the unfilled blood spot card must still be returned to the screening lab with all the patient information complete. - A repeat specimen may be required where the initial specimen is inadequate or where the result was equivocal. Repeat sampling will be performed by midwifery/neonatal nursing staff irrespective of the age of the child. Repeat samples must be taken and mailed to the laboratory within 24 hours of notification by the laboratory.
A protocol is in place for screening babies who are ill, transfused or born prematurely - QIS Standard 4a3
Repeat testing will be required in the following circumstances
- Transfused Babies If the baby has received a transfusion before the 5 day bloodspot the result of thyroid and cystic fibrosis screening may be unreliable so the laboratory will request a repeat sample, 72 hours after the last transfusion. Note that this is in addition to the pre-transfusion sample required to exclude Sickle Cell Disease.
- Premature Babies
If the baby was very premature (<32 weeks)
A further sample should be taken for retesting for hypothyroidism at 28 days of life
NB – it is no longer necessary to repeat a sample from a baby who was not enterally fed at the time of the 5th day sample
Where a previous sibling is affected by one of these disorders, or the parental carrier status is known to put this infant at increased risk the baby may need to be managed differently. This varies according to the condition, as described below:
Phenylketonuria
Risk - Siblings of a child known to have PKU will have a 1 in 4 risk, reducing to approximately 1 in 200 if one parent is a carrier and 1 in 100 if one parent is affected. It will be 1 in 2 where there is an affected parent and a carrier parent. The risk is 100% if both parents are affected.
Early testing (ie at 48 hours) may allow the parents of an affected sibling to know if their new child is affected or not a few days before the normal screening result becomes available. It may not however be as reliable as the day 5-8 test, and as there is no risk of neonatal disease, early testing should reserved for cases where there is significant parental anxiety expressed, and following counselling regarding the risk of a false negative result. For those families at lower risk or where there are mild (non-classical) elevations of then early testing is not recommended.
Screening process
At 48 hours (optional)
Send 2 drops of blood on a newborn screening card for phenylalanine and tyrosine measurement to:
Department of Biochemistry, Queen Elizabeth University Hospital, 1345 Govan Rd, Govan, Glasgow G51 4TF
Write on newborn blood spot card ‘Family history of PKU'
Day 5 – 8:
Routine newborn screen (5 drops on a newborn screening card), write on newborn blood spot card ‘Family history of PKU’.
Management
The baby should be breast fed or formula fed as normal. He is not at risk of becoming ill in the neonatal period
For further advice the attending metabolic consultant should be contacted via Yorkhill Switchboard during daytime hours.
Other inherited disorders of amino acid metabolism
For siblings of a child with one of the other inherited disorders of amino acid metabolism the risk is similarly 1 in 4. The case should be discussed antenatally with the metabolic team on an individual basis, and a plan of management clearly documented in the maternal notes.
Congenital Hypothyroidism
This is rarely an inherited disorder so no specific measures need be taken unless specified antenatally. This should be specified on the paediatric section of the yellow alert sheet of the maternal notes.
Cystic Fibrosis
Where both parents are carriers of Cystic Fibrosis this should be discussed antenatally and a plan made. The plan should be clearly documented in the paediatric section of the yellow alert sheet in the maternal notes.
In most circumstances cord blood is taken at birth and genetic testing for the parental CFTR mutations performed. For this to be successful, knowledge of the parental mutations is required, which should be dealt with antenatally if early neonatal testing is planned. If in doubt cord bloods can be taken, sent to the DNA lab in clinical genetics and stored pending discussion with the family and the attending consultant geneticist.
Medium Chain Acyl-CoA Dehydrogenase Deficiency (MCADD)
Where there is a previously affected child/and or parental carrier status suggests an increased risk to an infant, guidance has been issued by the NPSA on neonatal management pending results of testing (http://www.nrls.npsa.nhs.uk/resources/type/alerts/?entryid45=132858). This advises that the specialist paediatric inherited metabolic disorder services be contacted antenatally and a post birth plan made. As with other disorders it is vital that this is highlighted in the paediatric section of the yellow alert sheet in the maternal notes.
The following generic advice has been taken from the newborn screening handbook and updated by the Inherited Metabolic diseases team.
Testing
Additional testing should be offered to siblings of a child known to have MCADD (1 in 4 risk) - or where there is an extended family history which causes concern. The risk to the infant is approximately 1 in 200 if one parent is a carrier and 1 in 100 if one parent is affected. It will be 1 in 2 where there is an affected parent and a carrier parent. The risk is 100% if both parents are affected)
When to test and samples taken
24-48 hours:
- Diagnostic acylcarnitine profile (2 drops of blood on a newborn screening card), Write on newborn blood spot card ‘Family history of MCADD’
- Qualitative urinary organic acids (3 to 5 ml urine needed)
- MCADD mutation analysis (0.5 to 1.0 ml blood in an EDTA bottle).
These should be sent to the local biochemistry lab (after telephoning), along with the request form in appendix 4.
Day 5 – 8:
Routine newborn screen (5 drops on a newborn screening card)
Write on newborn blood spot card ‘Family history of MCADD’
Management
Prior to results
This baby is at risk of illness or death in the neonatal period. The aim of treatment is to prevent mobilisation of fatty acids by providing ample glucose - enterally or intravenously. It is essential to ensure that the baby maintains a good milk intake. A term baby should be fed every 4 hours and a preterm baby at least every 3 hours. Exclusively breast fed babies are particularly at risk in the first 72 hours when the supply of breast milk is poor; top up feeds of expressed breast or formula milk may be necessary in the first 48-72 hours until a good milk supply is established. If oral feeds are not tolerated, or if the baby is unwell in any way, urgent referral should be made to a paediatrician for review and consideration of nasogastric tube feeds or commencing intravenous glucose. It is not safe to base the management on monitoring of blood glucose as a baby may be seriously ill even if the blood glucose is normal. A baby should not be discharged until it is certain that he or she is feeding well.
Sickle Cell Disease (SCD)
Where both parents are Sickle Cell disease carriers, there is a 25% risk of the child being affected. This is of no clinical consequence in the neonatal period and so there is no clinical need for testing before the routine day 5 test. The latter should be carried out as normal, with a note on the test card regarding the family status to aid the screening laboratory.
In circumstances where there are particularly high levels of parental concern, consideration can be given to taking a blood spot for screening earlier (this must not be cord blood), but this is not encouraged. Testing should done only be after discussion with a consultant neonatologist, and it must be made clear that the routine day 5 test is still required to screen for other disorders. The card should be clearly marked as an early sample, and sent to the newborn blood spot screening lab, with the laboratory called in advance to discuss. Samples should not be sent to local haematology laboratories for analysis. A clear plan for feedback of results to the family must be made.
Positive results obtained through the routine (day 5) screening process will be dealt with by the screening laboratory with a direct referral to the haematology services in RHSC Yorkhill, or to genetic counselling services where carrier status is identified.
Method
- Wash hands and put on gloves
- Check baby's name and age with the parents (or identity bands if in hospital)
- Expose baby's heel
- If cleansing is required allow to dry completely before sampling
- Do not use Vaseline on the heel
- Hold foot firmly, encircling heel with thumb and index finger
- With one movement pierce the soft tissue of the outer aspect of the heel with the safety lancet
- Release pressure and allow blood to flow
- Completely fill all circles on blood spot card with blood ensuring that the blood soaks right through the card. Fill the circles from the centre. Try to avoid contact between the absorbent paper and the baby's heel or your gloves (note that samples where blood has been applied inappropriately or where the spots have been compressed/layered will be rejected – see below)
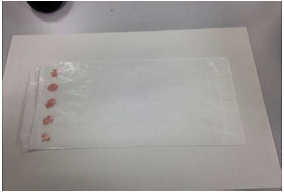
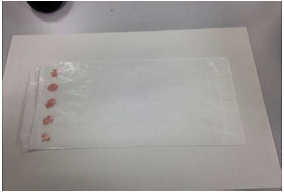
- Allow the blood spots to air dry completely before placing in the glassine sleeve. Only one card per glassine sleeve
- Using the cotton wool ball, apply slight pressure to the puncture site to stop the bleeding
- Apply spot plaster if required; this should be removed during the next episode of care
- Dress baby and leave comfortable
- Dispose of safety lancet in sharps box
- Wash hands
- Ensure the card is placed in a FREEPOST envelope and posted the same day
From the 12th of October 2015 the Scottish Screening laboratory has employed enhanced criteria for accepting blood spot samples, bringing the Scottish Screening laboratory into line with evidence based agreed UK national criteria for sample quality.
Why does the blood spot quality matter?
Good quality blood spot screening samples are vital for ensuring that babies with rare but serious conditions are identified and treated early. Poor quality samples can result in delayed referral and diagnosis of affected babies.
The most significant effects of poor quality samples are:
Falsely low analyte concentrations (false negative results), which can be caused by:
- Small volume spots (i.e. under-filled circles)
- Compression of the sample
Falsely high analyte concentrations (false positive results), which can be caused by:
- Layering of blood samples
- Applying the blood to the front and the back of the card
The Newborn Bloodspot Screening Card now has four circles instead of the previous five; the aim of this change in 2015 was to improve the quality of each circle.
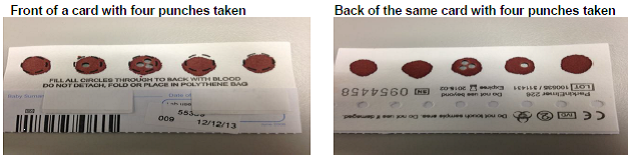
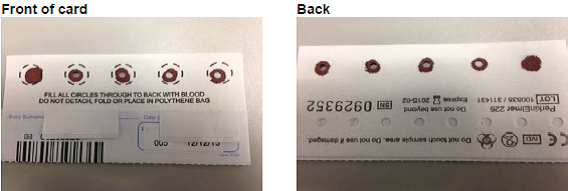
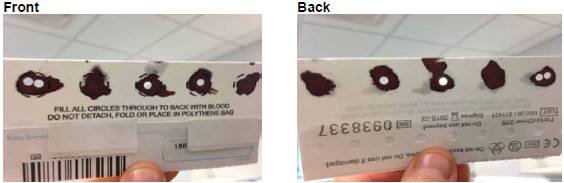
Please remember that it is extremely important that the blood fills the circles and soaks through to the back of the card. If the bloodspots are too small or not soaked through to the back of the card it is very likely that the sample will have to be repeated.
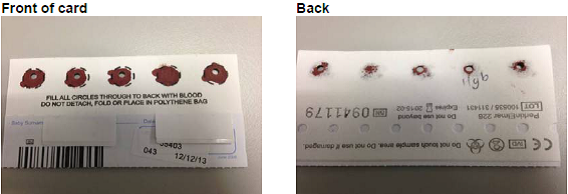
Examples of samples- good and bad (NB – photos from old 5 spot screening cards)
Good quality samples:
Insufficient samples:
Blood not soaked through to the back of the card:
Layered sample
This is where one spot of blood is layered directly on top of another, or the blood has been applied to one side of the card and then turned over and reapplied to the other side.
Sample placed in glassine envelope before it had completely dried:
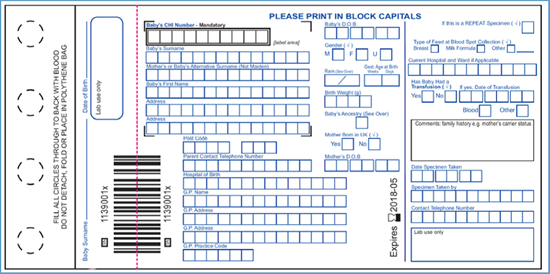
- The Blood spot card - Accurate completion of the data requested on the blood spot card cannot be over emphasised. Too much time is wasted in checking incorrect or missing information. Ensure all details on the blood spot card are completed (especially the CHI number) and sign the card. If the baby fulfils any of the criteria for repeat screening (see above) record this in the comments box on the blood spot card along with other important clinical information (eg delayed passage of meconium or echogenic bowel on antenatal scan).
- Computerised Discharge Report / Discharge documentation – A copy of the postnatal discharge documentation is sent to the GP on discharge from the postnatal ward. This will contain details of the blood spot test if performed before discharge
- Scottish Handheld Maternity Record (SWHMR) - Record heelprick sampling (or refusal of the test) in the postnatal record within the SWHMR.
- Neonatal Case Records - Babies who are in the neonatal unit at the time of testing must have a record of the blood spot test(s) in the medical/nursing notes according to local policy. This will include an entry in the Badger electronic record in units where this is in use. If the baby fulfils any of the criteria for repeat testing a plan for a repeat testing should be carefully documented.
- Transfer letter / Badger Discharge summary – If the baby is transferred to another hospital written documentation regarding newborn screening should form part of the transfer documentation
|
Additional Local Arrangements for documentation
|
All Women /parents / carers are informed of the timescale within which the results will be made available and the format in which they will be communicated and by whom - QIS Standard 4c1
95% of results are issued from the laboratory to an appropriate health care professional within 2 working days of the receipt of the specimen by the laboratory - QIS Standard 4f2
All positive results are communicated to women / parents /carers as soon as possible after the screen and no later than 14 days from the specimen collection for PKU and CHT and 27 days from specimen collection for CF - QIS Standard 4c3
Currently there are no arrangements to communicate all screening results to the parents/carers. They should be told that the test results are available within 2 working days of receipt of the sample by the screening laboratory, and that they will be contacted directly if the screen indicates that repeat testing or further investigation is required. This contact would usually occur within 1-2 days of the screen result being obtained by the laboratory. It is important to ensure that accurate contact telephone details are obtained from parents at the time of testing.
Newborn Blood Spot Screening Information for Healthcare Professionals - 2017
Parent Information Leaflet - “Your Baby, Tests offered – Scottish Screening Tests” will be available from the Health Scotland Pregnancy and Newborn Screening Page
Leaflets for each of the specific conditions, and links to external patient support groups, are available at: www.newbornbloodspot.screening.nhs.uk/public
Blood spot Screening Consent Form – See Appendix 1
Parental Information leaflet to be issued when screening declined – See Appendix 2
Letter to GP informing them that screening has been declined – See Appendix 3
|
Who has Parental Rights? The child’s father may have parental rights and responsibilities if:- (1) he is married to the mother (2) he is named as the father on the birth certificate (3) he has been assigned parental rights by a court order (4) the mother has sought a ‘parental responsibilities and parental rights agreement’. Parental Responsibilities and Parental Rights Agreement (Scotland) Amended Regulations 2006. Another person may have parental responsibilities if they have been appointed legal guardian by court order. However most other carers, whether they are relatives of the mother or foster carers assigned by social work, will not have parental rights. If a baby is going to be cared for by a person without parental responsibility consent should be obtained from the mother prior to discharge from the maternity unit. |
Last reviewed: 24 April 2024
Next review: 24 April 2027
Author(s): Dr Helen Mactier – Consultant Neonatologist, PRM; Dr Allan Jackson - Consultant Neonatologist, PRM; Dr Andrew Powls – Consultant Neonatologist PRM
Co-Author(s): Sarah Smith – Newborn Screening Coordinator - Scottish Newborn Screening Laboratory; Liz Chalmers – Consultant Haematologist QEUH
Approved By: West of Scotland Neonatology Managed Clinical Network

