Umbilical catheters
exp date isn't null, but text field is
Audience
This guideline is applicable to all medical staff, ANNPs or extended role practitioners placing umbilical catheters in neonates.
Reference should also be made to separate guidelines for aseptic technique, for the priming and calibration of arterial catheter sampling devices and guidance on arterial blood sampling techniques. Users should also refer to pharmacy monographs for heparinised saline and other infusion fluids. Trainees inserting catheters must have undergone competency based assessment for insertion of umbilical lines and for taking blood samples from arterial catheters (DOPS) or they must be supervised by a middle grade or senior colleague who is skilled in these procedures.
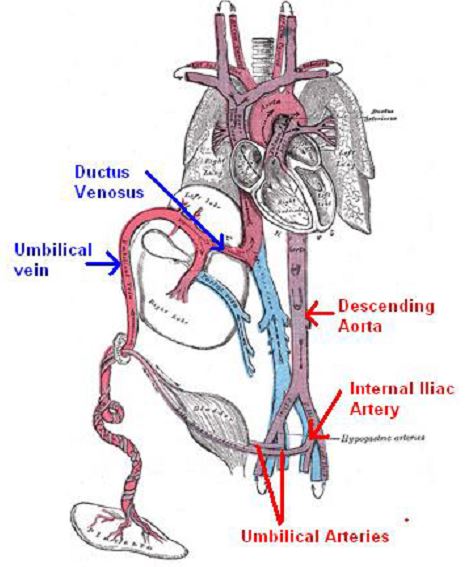
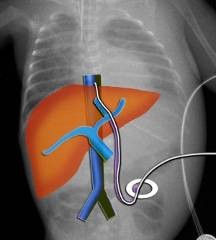
Fig 1. Diagrammatic representation of the fetal circulation
- Umbilical venous catheter (UVC)
- Secure, central venous access in neonates in the first 1-10 days of life
- Delivery of drugs and parenteral nutrition
- Emergency vascular access
- Exchange transfusion
- Umbilical arterial catheter (UAC)
- Monitoring arterial blood pressure
- Where frequent blood gas analysis is required
- Regular blood sampling
- Anterior abdominal wall defects
- Exomphalos, Gastroschisis, Umbilical fistula
- Infection
- NEC, Peritonitis, Omphalitis
- Evidence of local vascular compromise in lower limbs
- Abdominal surgery requiring an incision above the umbilicus
Double or single lumen catheters are available. Double lumen UVCs should be used as preference for those infants requiring multiple infusions as, although associated with increased risk of catheter malfunction; multi-lumen catheters decrease the need for peripheral access in the first month of life.
There is mandatory placement of a single lumen UVC for babies requiring balloon septostomy. For other purposes such as exchange transfusion or resuscitation a single lumen venous catheter may be advisable.
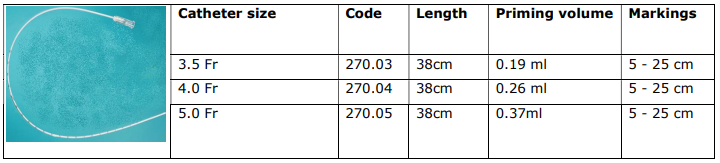
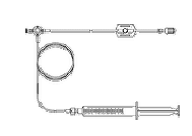
Arterial lines: Figure 2: Vygon PVC umbilical catheters and product characteristics
Venous lines: Figure 2: Vygon dual lumen UVC and product characteristics
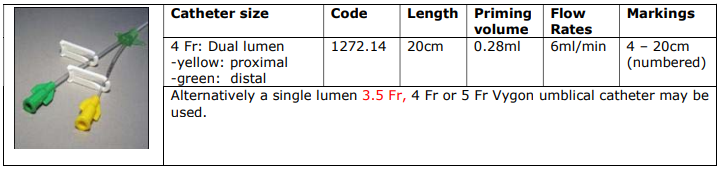
NOTE: The median diameter of the ductus venosus (DV), which is the narrowest point in the hepatic venous circulation, has a linear relationship with gestation2. For a UVC to be inserted without undue vascular trauma its external diameter should not exceed the DV diameter for gestion. Therefore at less than 25 weeks gestation a 3.5Fr catheter may be considered if there is difficulty advancing a 4Fr double-lumen catheter to the required insertion distance.
Prior to commencing the procedure it is essential to calculate insertion distance. Two of the most commonly used methods are described by Dunn and Shukla and Ferrara. Recent work has demonstrated that calculation methods are more accurate than measurement of the shoulder to umbilical length therefore this guidance only contains calculation method as detailed below.
Calculation (Shukla and Ferrara, Figure Four)
|
- UVC: 1.5 x Birth Weight (kg) + 5cm - UAC: 3 x Birth Weight (kg) + 9cm |
Remember to add the stump length to this calculation!
All central catheter tips must be x-rayed to confirm appropriate position.
Arterial Figure 5
|
Arterial Catheter Position |
 |
|
HIGH: T6-T10 ‘above the diaphragm’ Above the celiac and mesenteric roots and renal arteries |
|
|
LOW: L3-L5 ‘above aortic bifurcation’ Below most vessel roots though the inferior mesenteric artery arises from L3-L4 |
High UAC position is associated with significantly lesser risks of clinical vascular compromise as it avoids the origins of the major arteries. This position should be used exclusively unless a low position is the only position that can be obtained and a UAC is deemed necessary for optimum patient care. If the UAC is inadvertently placed too low it should be withdrawn to a position below the inferior mesenteric artery, that is below L4.
Venous Figure 6
All central venous catheter tips should ideally be sited at T8/9, assuming this is outside the cardiac silhouette.
|
Venous Catheter Position |
 |
|
T8-T9 ‘just below diaphragm on xray’ Pass through the ductus venosus and at the junction of the inferior vena cava with the right atrium |
If the catheter does not pass though the ductus venosus it usually comes to lie within the portal vein and cannot be further advanced - If so it should be withdrawn until it is possible to sample blood easily via the distal (green) lumen. This should be sufficient to allow free flow of infusate through the catheter when used. Alternatively consider inserting a smaller diameter catheter.
A UVC tip sited below T10 carries a significantly higher risk of extravasation. These should only be used in the short term (24 to 48 hours) if absolutely necessary while alternative access is sought.
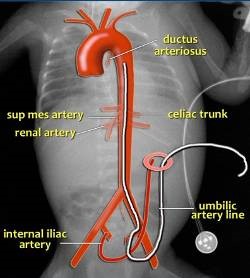
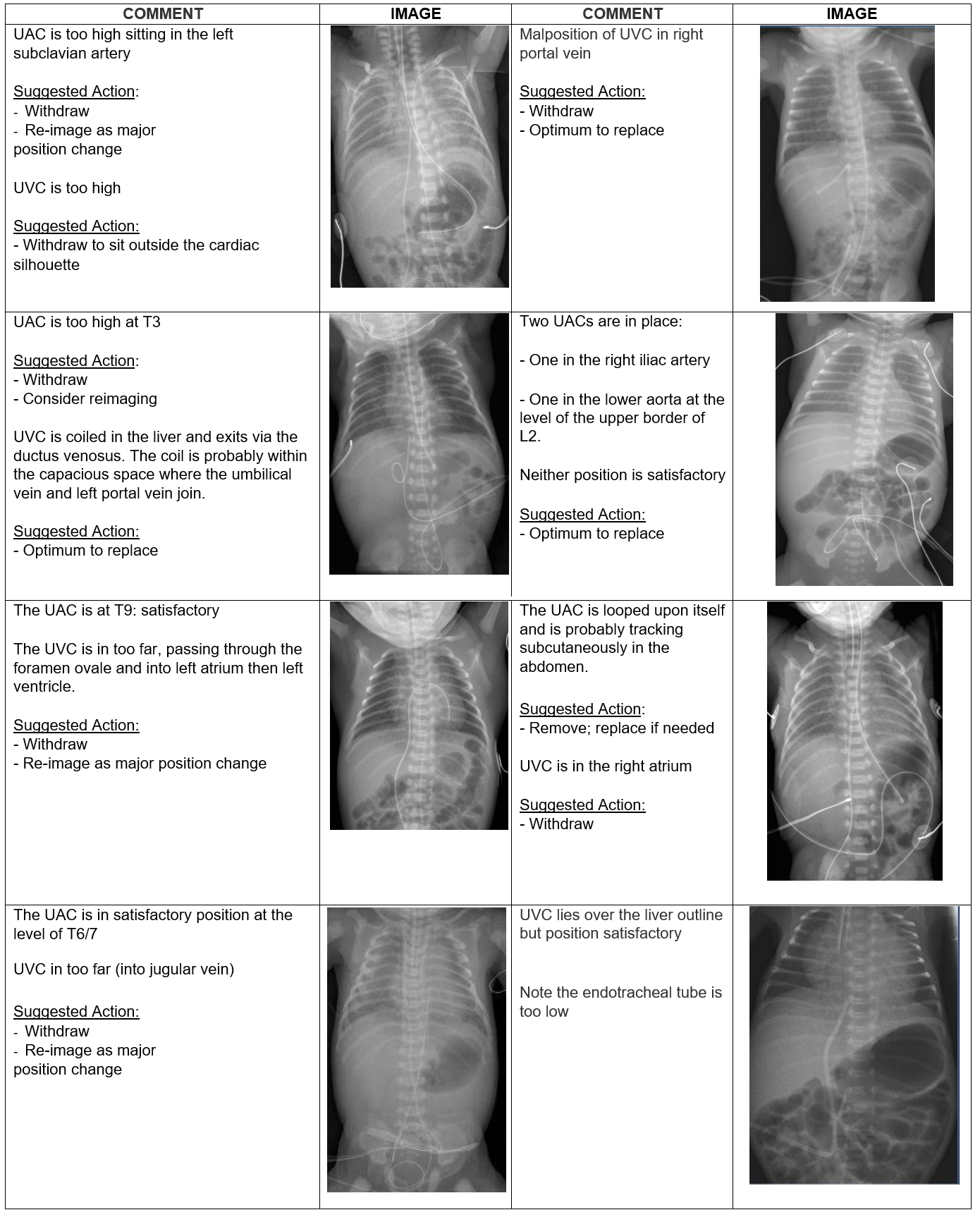
All umbilical catheters must be x-rayed to confirm appropriate position. This image must contain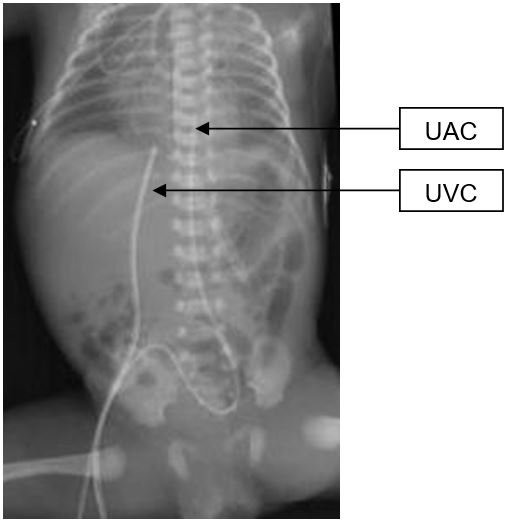 the abdomen as well as the chest to include the entire route of the catheter [Figure 7].
the abdomen as well as the chest to include the entire route of the catheter [Figure 7].
Remember only by demonstrating that the route of the catheter descends to meet the internal iliac artery before ascending the aorta can you be certain that the catheter has been placed in the artery rather than the umbilical vein.
UVCs that are inserted too far must be withdrawn to the correct position. A UVC in the portal vein has an increased risk of venous thrombosis and this may limit the length of time that the catheter should remain in situ.
[Figure Seven: X ray showing correct UAC and UVC positioning]
There is no evidence to support the practice of ‘railroading’ a second UVC beside
one which is thought to be malpositioned. This practice is to be avoided since it may increase the risk of vessel trauma and consequent extravasation.
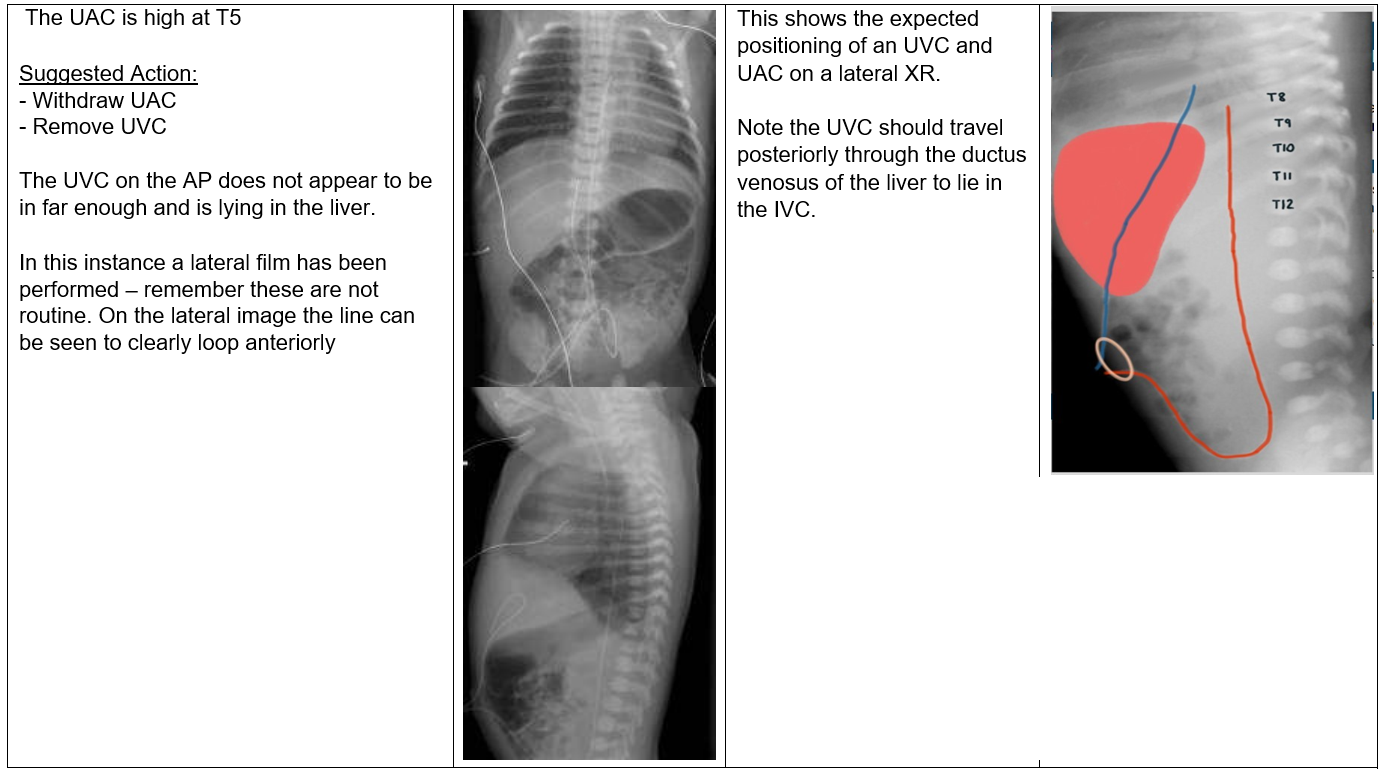
A repeat x-ray should be performed following major positional change of a catheter to confirm correct tip position. Repeat imaging should be considered when small positional adjustments have been made. If a line is suspected to follow an atypical route into the liver or is not functioning as normal consider use of a lateral film: lateral imaging for line position is NOT considered routine and should only be used in exceptional circumstances.
See Appendix A for further x-rays of umbilical catheter position.
The use of point-of-care ultrasound is an evolving technique to confirm catheter position and can be used where the facilities and skill mix allow.
Evidence has shown that up to 50% of UVCs will migrate at some point2 likely due to the Wharton’s jelly around the cord shrinking and exerting a ‘pull effect’ on the catheter. Clinicians therefore should be aware to assess line position on any further imaging undertaken to ensure ongoing adequate positioning.
In each situation where umbilical catheters need to be placed an assessment should be made as to who is the most appropriate person to undertake the procedure. Practitioners acknowledge that they must maintain their personal competence with the procedure and familiarity with local equipment.
Trainees new to the procedure must undergo appropriate training and supervision including completion of DOPS. Prior to undertaking this procedure, it is recommended that the practitioner review and complete the following learning resources:
- E-module available on RCPCH website: certificate of completion and 1 CPD point
- RCPCH 15-minute consultation: ‘Is this UVC safe to use?’ ADC Education & Practice Edition.2
Sterile gloves [2 pairs], Sterile gown, Umbilical catheter(s) as needed
Antiseptic solution relating to gestation: see other available guidance
Umbilical catheter placement equipment:
|
Measuring tape |
Gauze |
Drapes |
Umbilical tie |
Syringes |

Figure 8: Equipment for umbilical catheterisation
Green needles x 2, Needle-free adaptor x 2, NaCl 10ml or pre-made saline flush, Suture (additional)
Elective insertion of a CVC should be discussed with the parents in advance wherever possible although formal consent in emergency situations is not always practical. These discussions should be documented clearly. Provision of written information sheets can be helpful.
Prior to commencing the procedure:
- Position patient supine
- Ensure you have an assistant: MANDATORY for line insertion
- Ensure satisfactory cardiorespiratory monitoring and endotracheal tube secure if applicable
- Avoid placing items on patient during the procedure
- ‘Double-gloving’ for the procedure is advised
Consider the use of measures to relieve distress during the procedure such as containing the infant by swaddling or holding or expressed breast milk (EBM) or sucrose as analgesia. Refer to the following WoS guidelines for guidance about the use of oral sucrose for procedural pain (WoS Guideline – Oral Sucrose for Procedural Pain)
NB - Remember to calculate your catheter length prior to commencing!
|
Flush |
Never leave catheters open to atmospheric pressure. The abdominal venous system is under negative pressure so on deep inspiration air can enter the catheter and cause an air embolism. Connect needle-fee adaptors to the end of venous lines and flush all lumens with NaCl, line clamps should be closed when the catheter is not in use and 3way taps should not be used. A syringe with NaCl should remain attached to the arterial line. |
|
Clean |
An assistant should hold the cord with a gloved hand by the cord clamp. Care should be taken that this does not touch the field following cleaning as this will result in contamination. Clean around the umbilical cord and surrounding skin. Particular care must be taken to avoid any pooling of antiseptic solution. The solution must be used sparingly and, if inadvertently spilled, it should be cleaned off and dried. The patient must not be allowed to lie in excess solution. |
|
Drape |
The entire baby and all surfaces from the baby’s neck to the foot of the incubator should be draped to create a sterile field. Only the cord should be visible or exposed. Ensure ET can be seen if applicable. Remove ‘dirty’ pair of gloves at this point. |
|
Tie |
Tie umbilical tape around the base of the cord – tightly enough to minimise blood loss but loosely enough that the catheter can pass. |
|
Clamp |
Clamp across the cord using straight forceps. |
|
Cut |
Using scalpel cut cord cleanly 1-1.5cm from skin. Place the edge of the scalpel patient side of the forceps and cut away in one direction. Try NOT to make a sawing action. Your assistant should remove the section of cord with clamp that is cut off and dispose of it. Take care that this does NOT touch the sterile field. |
|
Identify |
|
|
Dilate |
If needed GENTLY insert closed tips of curved iris forceps into the lumen until the cut end of the artery is at the bend in the forceps. Allow the spring of the forcep to gently open and the artery can be dilated. Dilator probes may also be used. |
|
Insert |
Grasp the catheter with forceps or thumb and fingers. Insert into the lumen. You may need to support the stump. Note: you may encounter resistance at the anterior abdominal wall. Gentle steady pressure with slight rotation may help overcome this. Repeat probing or excessive pressure must be avoided to prevent pushing the catheter outside the vessel lumen causing false tracking. |
|
Aspirate |
All central catheters should allow free aspiration of blood in their final position, and this aspiration should be documented. |
|
Observe |
Careful observation periumbilically and distally in the lower limbs and buttocks, if visible, for blanching, cyanosis or mottling throughout the procedure. If persistent the catheter should be removed. |
|
Image |
To avoid the risk of occlusion catheters should have fluid running whilst awaiting xray. Arterial catheters should be connected to a continuous infusion of heparinised 0.45% saline (1 unit of heparin/ml) at a rate of 0.5ml/hour (1ml/hour may be used in babies >36 weeks gestation or >2.2kg birth weight) and venous lines should be used for infusions of 0.9% saline, glucose 10% or standard TPN. Other drugs or infusions should be avoided until appropriate positioning is confirmed by X-ray unless required for acute resuscitation. If not used in this manner the lines should be flushed intermittently whilst the xray is awaited. |
| Document |
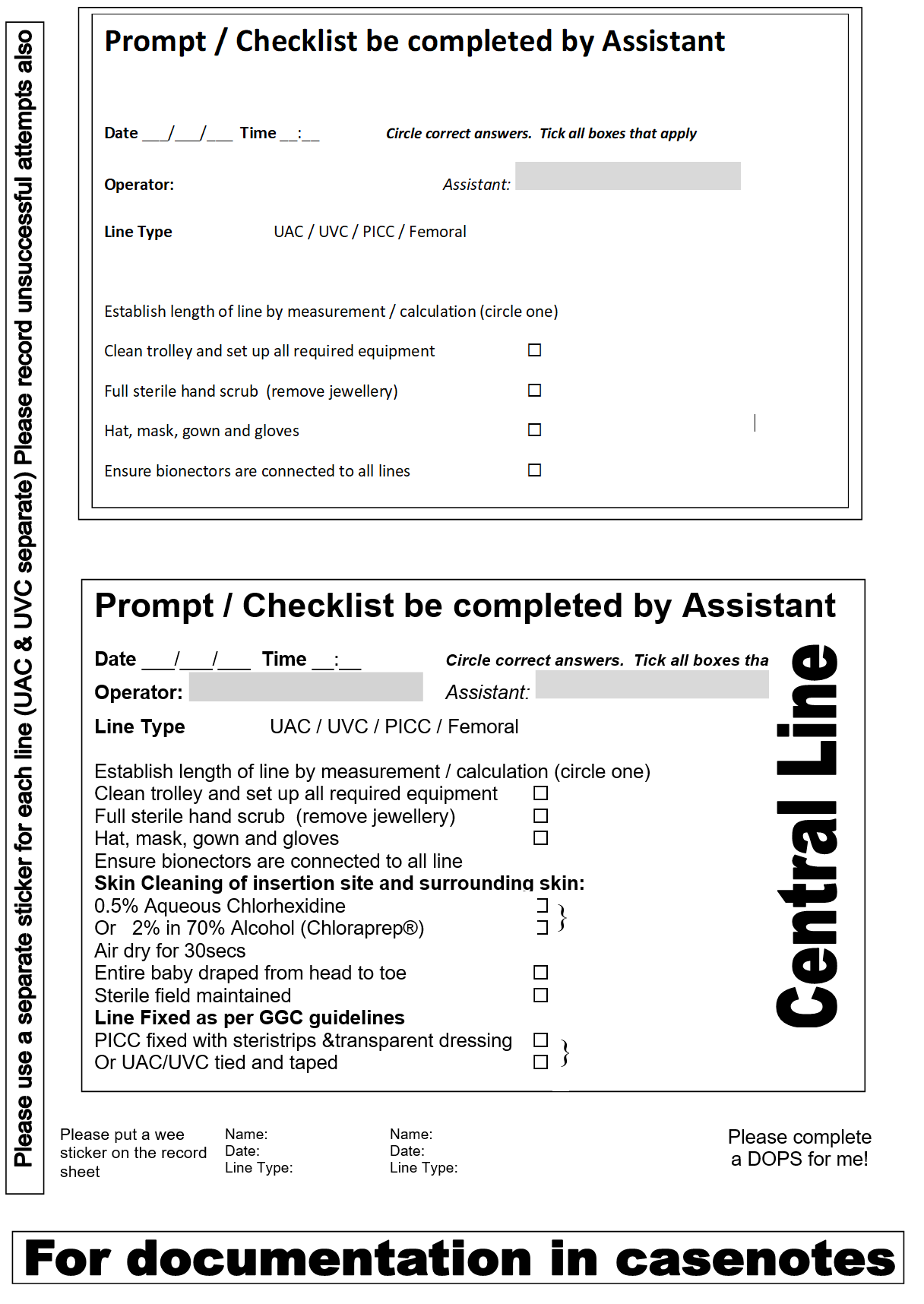
Contemporaneous documentation is essential. Insert central line sticker into patients case notes recording indication, line type, number of attempts, insertion length, position on X-ray and any adjustments subsequently made. The accepted position should be verified in writing within 24 hours of insertion by a consultant neonatologist. Ensure the care bundle is initiated. [Appendix B] |
Catheters should NOT be used if it is not possible to sample blood from them
One of the most frequent and potentially avoidable complications of umbilical catheters is inadvertent displacement which can result in significant blood loss and the loss of vascular access. Catheters must be sutured to the cord. Each catheter and securing suture should then be secured together with tape.
Each catheter requires separate fixation and the UVC and UAC should never be secured together.
In practice lines are secured with sutures prior to imaging allowing easy adjustment of position if required following. They are then taped securely in final position.
Label to distinguish arterial and venous catheters.
|
1. Suture through a large chunk of cord. A purse-string suture- using 3 bites of umbilicus around its circumference – may increase the security of this suture |
 |
|
2. Tie a knot around the umbilical catheter close to the insertion point. The knot should be tight to prevent slippage and ideally 2-4 hitches should be used to avoid the knot slacking. Each one should be tied in a reverse direction to the previous |
|
|
3. Pass the suture around the catheter again, 1-2mm higher up, and tie another knot in identical fashion. This step can be repeated a maximum of two times for additional security if required |
 |
|
4. Using highly adhesive tape stick the catheter to the suture material ensuring the latter is taut. The tape should be close to the catheter base |
|
|
5. Loop the catheter through 180 degrees and apply to tape |
 |
|
6. Stick both ends of the suture to the tape at an angle to each other as shown and then wrap the tape back on itself ensuring no adhesive surface is left exposed. Tip- if you fold over a small segment of the tape at each end it will be easier to unpeel the tape if required |
 All arterial catheters should be connected to a blood pressure transducer and the infants blood pressure should be monitored continuously. This provides an early warning of inadvertent disconnection as well as providing blood pressure measurements. An intermediate sampling point is also required and should be inserted between the arterial line and the pressure transducer – a closed circuit blood sampling set is routinely used to minimise the risk of infection Medex DPS Kids Kit (neonatal). The arterial line should be connected directly to this set and no additional connector.
All arterial catheters should be connected to a blood pressure transducer and the infants blood pressure should be monitored continuously. This provides an early warning of inadvertent disconnection as well as providing blood pressure measurements. An intermediate sampling point is also required and should be inserted between the arterial line and the pressure transducer – a closed circuit blood sampling set is routinely used to minimise the risk of infection Medex DPS Kids Kit (neonatal). The arterial line should be connected directly to this set and no additional connector.
Refer to the following WoS guidelines for guidance about the use of these sets (WoS Guideline - Arterial Lines: Priming and calibration) and procedures for taking arterial line samples (WoS Guideline - Arterial catheter blood sampling).
The need for continued use of a central catheter should be reviewed daily. There is little evidence around the optimum dwell duration of central venous catheters in the neonatal population. Two single-centre studies suggested that the use of umbilical catheters for greater than 7 days is associated with an increased risk of central line associated bloodstream infection compared with use less than 7 days. If it is anticipated that a catheter is likely to be necessary for longer than 7 days then it should be replaced with a PICC. There is no trial data to compare early removal versus expectant management although observational data shows early removal will decrease incidence of infection.
All umbilical catheters should be monitored following insertion. The umbilicus should be examined at every care episode to ensure no bleeding, purulent discharge or peri-umbilical cellulitis. Ensure the catheter remains adequately fixated and is securely attached with no tension applied to the lines following change of position. Such observation is easier when the baby is in the supine position in an incubator, however prone positioning may be required on occasion. For either prone lying or kangaroo care it is important that an additional check of the umbilical catheter(s) is performed before moving the baby into the new position. It may be necessary for two people to assist such a move with one person caring for the line whilst the other adjusts the baby’s position. The commonest scenario is that of an ELBW baby who has recently been extubated to CPAP in whom prone positioning improves respiratory mechanics. In other infants it may also be desirable to permit a period of kangaroo care whilst an umbilical line remains in place. Ensure regular review of position, minimise catheter access and maintain strict asepsis.
Consider running an infusate through or regular flushing of any unused lumen to prevent blockage or occlusion. Ensure this is not to the detriment of nutrition for your patient.
- Care must be taken whilst cutting the sutures - holding the umbilical lines, to avoid the potential risk of the line being cut. Stitch cutters should be used to cut the retaining sutures rather than a scalpel or scissors.
- Artery forceps should be available at the cot side during umbilical catheter removal so that the catheter or umbilical stump can be clamped immediately in the event of acute blood loss
- Complications arising from accidental severing of umbilical catheters include blood loss (more common with UAC) and intra-abdominal entrainment of the catheter (more common with UVC)
The latter is an emergency and requires transfer of the infant to a unit with surgical / cardiac catheter expertise
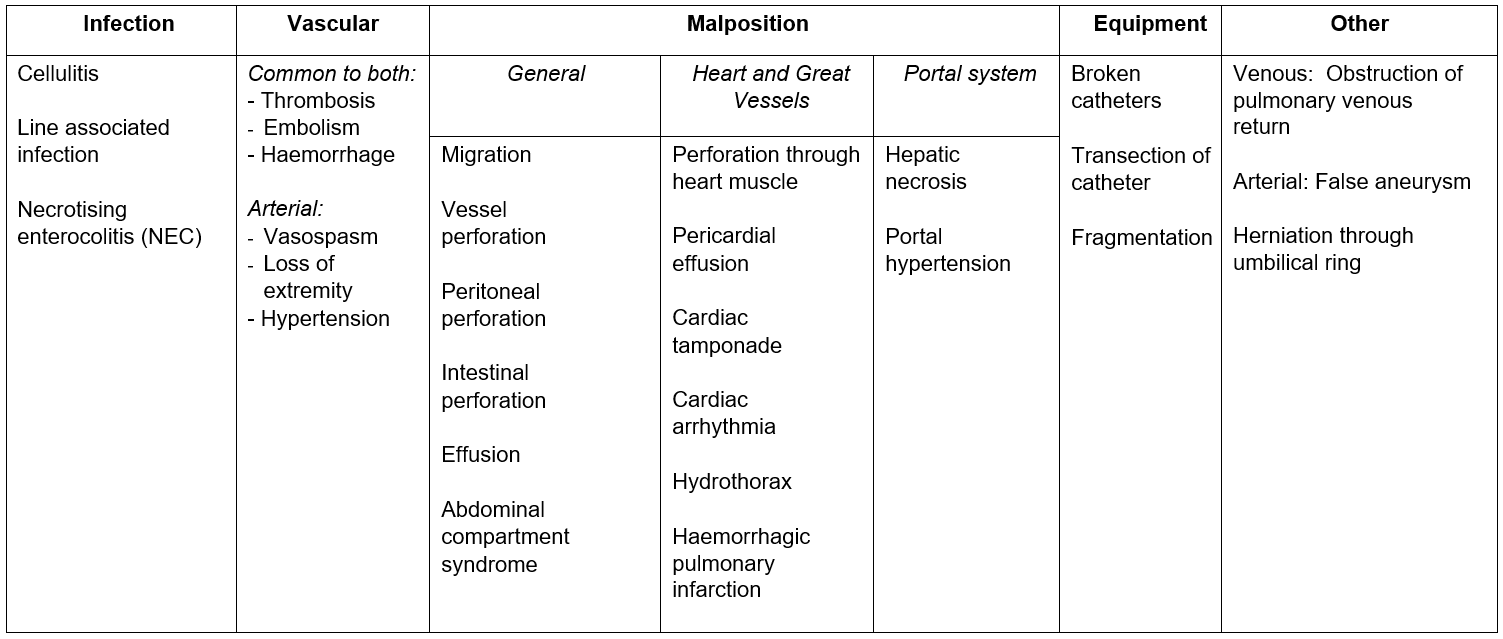
Any clinical deterioration in an infant with a central venous catheter in situ should raise the question of potential catheter related complication, particularly infection, extravasation and tamponade.
Abdominal compartment syndrome is a complication secondary to extravasation of low-lying UVCs and presents with marked abdominal distention, respiratory distress, oliguria, haemodynamic instability and compromise to lower limb perfusion 2.
Abdominal paracentesis may be required for an infant in extremis and might need to be considered prior to patient transfer. A guide to performing abdominal paracentesis is included in Appendix B.
Emergency abdominal paracentesis for abdominal compartment syndrome due to massive ascites/ pneumoperitoneum
This should be considered when abdominal distension is causing haemodynamic or respiratory compromise and an x-ray has excluded intestinal dilatation as a cause.
Procedure
- Position infant at a 30 degree tilt (nappy/roll under right flank to position baby with left side down)
- Consider analgesia if time/clinical state allows (morphine or fentanyl bolus, local anaesthesia, oral sucrose)
- Prepare equipment:
- Green or grey cannula
- 3-way tap
- 10 ml syringe
- Catheter
- Clean skin with appropriate cleansing solution for gestational age (see appropriate WOS guidance)
- Attach 3-way tap to cannula and syringe and ensure tap is “open” to baby and syringe
- Location:
- Halfway between umbilicus and symphysis pubis, anterior superior iliac spine on left side of abdomen
- Slowly advance cannula at 45° angle toward umbilicus while gently aspirating syringe
- Stop when fluid/air obtained and push advance cannula catheter off over needle
- Remove needle stylet, attach 3-way tap and syringe to catheter
- Aspirate desired amount of fluid/air
- Remember to send fluid for:
- Biochemistry: LDH, Protein, Albumin, glucose, triglycerides, amylase, electrolytes, urea and creatinine
- Microbiology: Gram stain, culture and sensitivity
- Haematology: Lymphocyte count (if suspect chylous)
- Secure with adhesive dressing
- Leave 3 way tap in place but “switched off” to baby – can be re-aspirated if fluid/air accumulates in transfer
Note: Monitor haemodynamic parameters / urine output as fluid shift may occur
- Documentation – (Appendix D provides a sticker for the notes to act as a prompt and checklist for the operator and their assistant)
- Indication for line insertion
- Insertion length
- Flushing and sampling
- X-ray position
- Any adjustment required
- Final position if adjusted
- Catheter type and serial no
- CVC care bundle used
- Parental communication
- Removal information
- Length of time in situ
- Reason for removal
- Changed for alternative access as still in situ 7-10 days
- Catheter malfunction – not sampling, sepsis, inadvertent removal, suboptimal positioning, extravasation
- BAPM Framework - Use of Central Venous Catheters in Neonates - a Framework for Practice
- Manea C, Pryce R, Ramadan G. Fifteen-minute consultation: Is this umbilical venous catheter safe to use? Arch Dis Child Educ Pract Ed 2023; 108: 173-180.
Last reviewed: 02 October 2023
Next review: 02 October 2026
Author(s): Dr Emily Mullan, Neonatal Trainee
Co-Author(s): Other Professionals consulted: West of Scotland Neonatal Guideline group, Dr L McGlone, Mr T Bradnock, Mr G Walker
Approved By: West of Scotland Neonatology Managed Clinical Network


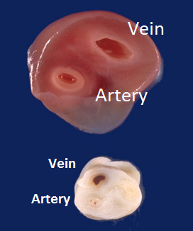 Identify vessels. Typically -
Identify vessels. Typically -